Additional Information on Anatomy and Physiology of Normal Breasts
Breast Development
- 4-6 weeks in utero
- Breast development begins
- 8 months in utero
- Nipples appear
- 34 weeks in utero
- Breast bud appears
- 8-13 years
- Onset of pubertal breast development
- Adipose tissue and ductal tissue grow from estrogen
- Progesterone initiates lobular growth and alveolar budding
- Breasts usually develop over a 2-4 year span
- Onset of pubertal breast development
Reference
De Silva NK, 2012
Additional Information on Extramammary Breast Pain
Pain originating in areas other than breasts caused by:
- Musculoskeletal pain
- Cardiac pain
- Gastrointestinal pain
- Tietze Syndrome
- Shingles
- Medications:
- Digoxin
- Spironolactone
- Chlorpromazine
Reference
Chase C, et al., 2011
Additional Information on Mastalgia
Breast Exam
- Entire breast area should be examined (lymph nodes, cervical and thoracic spine, chest wall, and arm pits)
- Patient should be in supine position to determine if pain is extramammary or breast pain
- If breast mass is felt during the examination – refer for radiographic work
Reference
Rodden AM, 2009
Mastalgia Diagnosis
| Diagnosis | Discussion |
|---|---|
| Breast Pain Diary |
|
| Urine Pregnancy Test |
|
| Breast Exam |
|
| Imaging |
|
Reference
Rodden AM, 2009
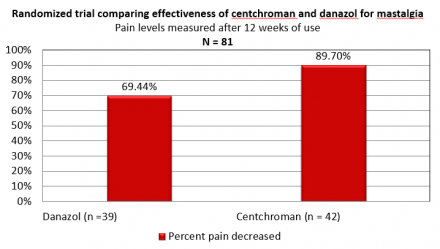
Comparison of Effectiveness of Centchroman and Danazol for Mastalgia
Additional Information on Age Related Breast Pain
Adolescents – Benign Breast Disease
Risk factors for developing benign breast disease from adolescent health:
- Thin – More adipose in childhood (OR, 0.91; P=.04) associated with lower risk of developing Benign Breast Disease (BBD)
- Tall – Girls with rapid height growth were most at risk (OR, 2.12; P=.09)
- Rapid growing – Girls with history of maternal breast cancer and rapid growth had higher risk of developing BBD (OR, 1.47; P= .02)
Study Design
- 9-15 year old females completed annual questionnaires from 1996-2001, 2003, 2005, and 2007 about menarche, height, weight
- On the 2005-2007 surveys, 6899 females (ages 18-27) reported if a healthcare provider ever diagnosed them with Benign Breast Disease (n=147) and if it was confirmed through a biopsy (n=67)
- Based on the results from the questionnaires, risk factors were identified for developing benign breast disease
Reference
Berkey CS, et al., 2011
Adolescents - Mastalgia
Mastalgia is common in adolescents.
- Conduct a history and physical examination
- Because mastalgia can be a symptom of pregnancy, a pregnancy test should be administered
- Conduct nutritional history for potential aggravating agents
Greydanus DE, et al., 2006; De Silva NK, 2012
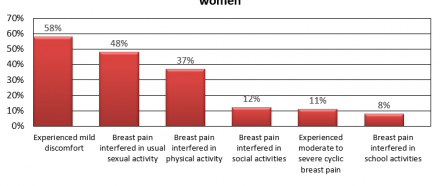
Cyclic Breast Pain
Cyclical Breast Pain may cause:
- Absence from school or work, sports, etc.
- Interrupt sleep
- Increase pain during sexual activity
Reference
Chase C, et al., 2011
American Women Experiencing Cyclic Breast Pain
Cyclic Breast Pain - Menopause
Prevalence of breast discomfort:
- 21% lower in late perimenopause compared with early perimenopause
- Breast tenderness shown as an adverse effect of menopausal hormone therapy
- Change in sex steroid levels may influence breast discomfort
- As evidenced by prevalent breast tenderness during premenopausal compared to the decline of prevalence in menopause
- However, prevalence and causes for breast pain in postmenopausal women is not well-understood
- ~40% of women experience cyclic mastalgia during premenopausal years
- Cyclic pain may worsen during perimenopause
- This may be due to hormones surging and dropping erratically
- Cyclic pain may continue into menopause
- especially for those using oral contraceptives or hormonal therapy
- Although cyclic pain is often resolved during menopause, women may still experience breast tenderness and pain
Reference
Breast pain, 2005; Rosolowich et al., 2006; Chase C, et al., 2011
Additional Information- Benefits of Lactation
Benefits for breastfeeding:
- Decreases childhood infection incidence
- Lower sudden infant death syndrome
- Lower post-neonatal mortality rates
- Reduced childhood obesity incidence
- Reduced childhood diabetes
- Reduced certain childhood cancers
- Can help to lower postpartum bleeding and reduce the risk of breast and ovarian cancer
Reference
Breastfeeding, 2015; Eidelman AL & Schanler RJ, 2012; Lessen R & Kavanagh K, 2015; Spatz DL & Lessen R, 2011; Steube A, 2016
U.S. Women Exclusively Breastfeeding
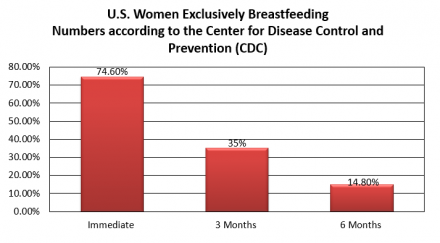
Reference
Dennis CL et al., 2014
Additional Information on Pain During Breastfeeding
Sore Nipples
| % of Breastfeeding Mothers | Description |
|---|---|
| 34%-96% | Nipple pain and trauma caused from breastfeeding |
| 29%-76% | Traumatic nipples (visible skin breakdown) |
| 80%-90% | Mild nipple pain (of breastfeeding women) |
| 26% | Nipple pain develop into nipple fissures |
Reference
Shanazi M, et al., 2015; Kent JC, et al., 2015
Traumatic Nipples and Sore Nipples
Due to Nipple Trauma (Traumatic Nipples):
- The greatest nipple pain intensity seems to happen between 3-7 days postpartum for most women
- Can cause psychological distress
- Can interfere with:
- Sleep
- Activities
- Mood
- Mother/child bonding
- May lead to deprivation of breast milk
- If traumatic nipples occur early can lead to cessation of breastfeeding
- Untreated nipple pain can develop into nipple fissures
- Nipple fissures increase the risk for bacterial infections
- Latch needs to be improved to reduce trauma and promote healing
- If sore nipples occur early can lead to cessation of breastfeeding
- Too little supply of milk can cause pain due to overlong nursing periods.
- A low milk supply can result from nipple pain
- inhibition of milk ejection from pain and not removing milk properly when infant has ankloglossia or cleft palate
- A low milk supply can result from nipple pain
Reference
Shanazi M, et al., 2015; Kent JC, et al., 2015
Commonality of Attributed Nipple Pain
N = 264 cases
| Attributed Cause | n |
|---|---|
| Incorrect positioning and attachment | 238 |
| Ankyloglossia | 177 |
| Insufficient milk supply | 104 |
| Palatal anomaly | 117 |
| Flat or inverted nipples | 32 |
| Vasopasm | 14 |
| Mastitis | 32 |
| Confirmed infection | 69 |
| C. albicans | 7 |
| S. aureus | 56 |
| Other bacteria | 6 |
Reference
Kent JC, et al., 2015
Etiology for Nipple Pain
- Positioning of infant/ Poor attachment/ Pumping with incorrect shield size
- Flat or inverted nipples
- Infant sucking action
- Infant ankyloglossia
- Infant palatal
- Infant suction
- Milk blisters
- Infections
- Eczema/Psoriasis/Dermatitis
- Pregnancy
- Raynaud’s Phenomenon
- Lack of nipple exposure to light and air
- Frequency and duration of feedings
Reference
Kent JC, et al., 2015; Dennis CL, et al., 2014
Treatments for Sore Nipples
From the Breast Feeding Centre of Western Australia:
Correct Positioning and attachment
- Most common recommendation
- When corrected early, breastfeeding duration is prolonged and sore nipple prevalence is reduced
Improving Latch
- Infants between 4 days- 12 months old, this has been proven to resolve breast pain in 65% of cases
Nipple Shields
- Short-term remedy for premature infants
- Helps with mothers who have flat/inverted nipples.
- Helps decrease intense suction
- Should not be used too long
Anhydrous Lanolin/Vitamin A Ointments
Remedy for nipple pain caused by friction
Frentomy for Ankyloglossia
- Effective for pain relief and to increase milk transfer
- Points to consider: Infant with tongue tie may have already developed and learned usual tongue mechanics which means fixing the tongue tie may not immediately relieve pain in the mother’s nipple.
Warm Compress
- Helps with milk blisters
Antibiotics/Antifungal
- For breast pain caused by infection or Candida infection
Avoiding Irritants/Topical Corticosteroid Ointment
- Remedy for Dermatitis and Psoriasis of the nipple
- Points to consider: Topical steroids can be harmful for present trauma/fissures
- Can delay healing
Warmth/ Avoidance of Vasoconstrictors/Prescriptions for Nifedipine
- Remedy for Raynaud’s Phenomenon.
Herbal Treatment: Lanolin
- Gives moisture to nipples
- Penetrates skin to help facilitate absorption of medicines
- Can absorb up to 30% of water
- Use of Lanolin associated with an increase in the rate of infection
- Could be a result of hand hygiene when applying lanolin to the nipples
Herbal Treatment: Dexphanthenol
- Part of B complex vitamins
- Works a moisturizer to help keep skin hydrated by reducing water loss through the epidermis and can help to reduce nipple pain
Herbal Treatment: Peppermint
- Has been shown to decrease pain and increase healing in nipple trauma
- Can help to increase tissue flexibility and prevent fissures
- An effective treatment of traumatic nipples for patients interested in using herbal medications
References
Kent JC, et al. , 2015; Berens PD, 2015
Shanazi M, et al., 2015; Kent JC, et al., 2015
Treatment Considerations for Sore Nipples
- There is no sufficient evidence showing glycerin gel dressings, breast shells with lanolin, lanolin alone, or all-purpose nipple ointment (APNO) significantly improve maternal perceptions of nipple pain
- APNO has not been found to be superior to lanolin in treating nipple pain
- A separate study failed to find a difference in pain between groups at 1 week of treatment for women using either APNO or lanolin
- Not enough evidence to recommend a specific treatment for painful nipples
- Some studies suggest applying nothing or expressed breast milk for early breast discomfort may be just as or more beneficial in the short term than applying ointment such as lanolin
- Regardless of treatment, nipple pain in most women seemed to reduce to mild levels 7-10 days after giving birth
Reference
Dennis CL, et al., 2014; Dennis CL, et al., 2012; Berens PD, 2015
Pumping Breast Milk with a Nipple Shield That Is Too Small
Raynaud’s of the Nipple
Noticeable whiteness of nipple immediately after breastfeeding, then turning red or purple.

Treatment Option
Use of Nifedipine
- 10 mgs three times per day
- Or sustained released capsule of 30 mgs per day
Reference
Wu M, Chason R, Wong M, 2012
Yeast and Cracking
Yeast

Cracking

Plugged Ducts/Engorgement
- Engorgement, plugged ducts, and mastitis are common causes of pain and may lead to cessation of breastfeeding
- Cessation can be permanent or temporary
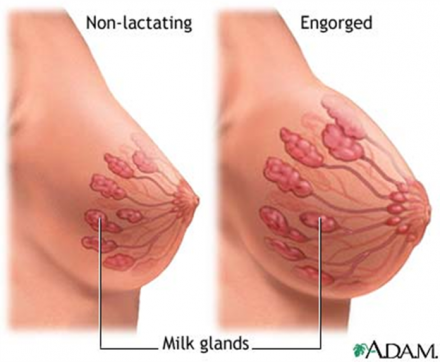
Engorgement can happen:
- When milk first "comes in" to the breasts, during the first few days after birth.
- When a regular breast-feeding routine is interrupted and the mother cannot nurse or pump as much as usual.
- If the baby suddenly stops breast-feeding.
- When the baby's breast-feeding suddenly drops, either when the baby is starting or increasing solid foods or when the baby is ill with a poor appetite.
Engorged breasts:
- Are swollen, firm, and painful. If severely engorged, they are very swollen, hard, shiny, warm, and slightly lumpy to the touch.
- May have flattened-out nipples. The dark areola may be very hard. This makes it difficult for the baby to latch on.
- Can cause a slight fever of around 100F.
- Can cause slightly swollen and tender lymph nodes in the armpits.
Data from the Infant Feeding Practices Survey in 2008 showed that 36.6% of women reported feeling their breasts were overly full within the 1st 2 weeks of postpartum breastfeeding.
Reference
Witt AM, et al., 2016; Berens PD, 2015
Treatment for Plugged Ducts/Engorgement
- Therapeutic Breast Massage in Lactation (TBML)
- Can help to empty the breast, which can help to reduce pain and resolve symptoms
- Provides immediate significant pain relief
- Reduces engorgement severity, provides immediate size reduction, and sometimes can provide complete resolution for plugged ducts
- Mother’s reported they were able to use TBML technique on their own after learning and receiving this treatment at a medical office
- This provides evidence that TBML can be taught and used outside of medical offices
- Cabbage Leaves
- Some studies have shown this treatment reduces pain, but there has been no statistical evidence to show these interventions improved symptoms better than routine care
- Cold Pack
- Some studies have shown this treatment reduces pain, but there has been no statistical evidence to show these interventions improved symptoms better than routine care
- Manual Expression
- Pumping Before
- Reverse Pressure Softening of the Areola
Reference
Witt AM, et al., 2016; Berens PD, 2015
Alternative Pain Treatment for Plugged Ducts/Engorgement
- Oxytocin
- Breast ultrasound
Reference
Berens PD, 2015
Proper Attachment and Latch
- Frequent Nursing: Breastfeed on demand.
- Application of Warmth: For only a few minutes at a time, apply warmth to the breasts by standing in a warm shower, applying warm washcloths, or by dipping the breasts in a bowl of warm water and allow some milk to flow out. Shower water should not spray directly on the engorged breasts. Application of warmth should not be done for longer than a few minutes because it may worsen swelling and inflammation caused by the engorgement.

Breast Massage
Before nursing, gently massage the breast toward the nipple and allow some milk to flow out to soften the nipple for easier latch. During nursing, gently compress and massage the breast to stimulate the letdown of milk.

www.breasthealthproject.com
Treatment Considerations of Plugged Ducts/Engorgement
- Receive consultation from an experienced lactation expert
- Extreme engorgement can lead to improper infant latch which can lead to pain
- Symptoms tend to improve over time regardless of the remedy or routine care
- Studies show that further scientific investigation on painful engorgement is necessary
Reference
Zhao C, et al., 2014; Berens PD, 2015
Additional Information on Treatment Considerations of Lactation Pain
Important considerations:
- important to specifically measure mothers thoughts on breastfeeding
- Example: Edinburg Postpartum Depression Scale (EDPS) to identify mother’s frustration and possible related depression
- Women with pain had a much higher likelihood of having a score on the EDPS consistent with depression (38%) compared to those without pain (14%)
Likelihood of Experiencing Depression From Breast Pain Based on Edinburgh Postnatal Depression Scale (EDPS)
| Pain | Likelihood of having score consistent with depression based on EDPS |
|---|---|
| High pain | 38% |
| Reduced pain | 16% |
| Without pain | 14% |
Reference
Berens PD, 2015
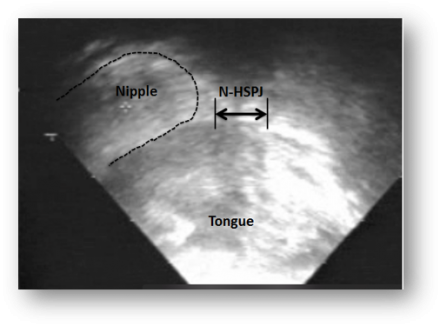
Additional Information on Short Frenulum
Patients and methods:
Twenty-four mother-infant dyads (infant age: 33 +/- 28 days) that were experiencing persistent breastfeeding difficulties despite receiving professional advice were recruited. Submental ultrasound scans (Acuson XP10) of the oral cavity were performed both before and >or=7 days after frenulotomy. Milk transfer, pain, and LATCH (latch, audible swallowing, type of nipple, comfort, and hold) scores were recorded before and after frenulotomy. Infant milk intake was measured by using the test-weigh method.
Pre-Frenotomy
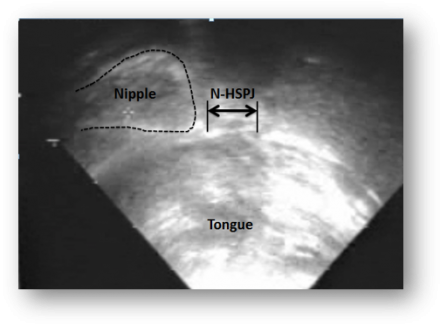
Post-Frenotomy
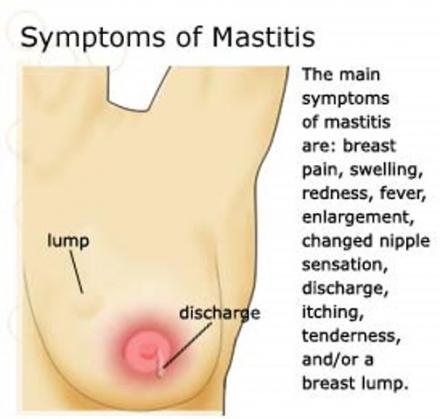
Additional Information on Mastitis
Symptoms of mastitis:
- Breast pain
- Swelling
- Redness
- Fever
- Enlargement
- Changed nipple sensation
- Discharge
- Itching
- Tenderness
- And/or a breast lump
Treatment of Mastitis
- Breast Drain
- Early mastitis may be managed by draining the breast
- Make sure affected breast is appropriately drained
- Infected breast should remain drained to manage infection (if there is an infection)
- Antibiotics
- Early infection may resolve itself through breast drainage, but if not, antibiotics should be considered
- If high fever is present or symptoms do not resolve in 12-24 hours then antibiotics are recommended
- Dicloxicillin or cephalosporin are used because the most commonly found organisms are streptococcus and staphylococcus
- Typically taken for 10-14 days
- Frequent breastfeeding and rest
- Components of management
- Feedings should take place on affected breast to allow for a drained breast, unless pain prohibits
- If pain prohibits feeding on affected breast, start with other breast and move to affected breast once pain has decreased
- If feeding is terminated or pain prohibits any type of breastfeeding, pumping should take place on affected breast to drain breast
- Bed rest and increase fluids can help
- Pain Medication
- Ibuprofen can be considered for pain
- Ibuprofen may aid in reducing inflammation in breast
- Prevention of Recurrence
- Investigate risk predisposing factors such as nipple trauma, poor breast drainage, breast mass
- If none of these are relative, it is important to look into hygiene and care of pump as possible risk factors
- Milk Culture
- May be requested for recurrent episodes of mastitis
- mastitis that does not relieve in 48 hours of antibiotic therapy.
- Instance with premature or ill infant
- Infants in the NICU
- Infant on immunosuppression
- Exclusively pumping mothers who would not have had infant at breast for source of infection
- When choosing antibiotics that may be less likely to treat suspected organisms due to an allergy
- High rate of resistance in the community or recent hospitalization
- Infant
- If mother suffers from nipple trauma or fissures, consider observing latch, feeding, positioning, and observe infant’s tongue for tongue tie
- Imaging
- Not usually used for mastitis
- However, if antibiotics fail or if there is a breast mass, ultrasound may be used to evaluate for breast abscess
- Mammography may be used during acute infection
- However, may be misleading due to inflammatory changes
- Treat the infection. Pursue mammography after resolving infection, if one
Reference
Adapted from Berens PD, 2015
Additional Information on Benign Disease Related
Infectious Inflammation
- Staphylococcus
- Most common etiological agent of mastitis
- Staphylococcus aureus
- Related to acute mastitis cases
- More commonly found than Candida when fissures on nipples are present
- Related to acute mastitis cases
- Staphylococcus epidermidis
- Can cause nipple pain, breast engorgement
- But is usually misdiagnosed as “noninfectious” or “mammary candidiasis”
- Can cause nipple pain, breast engorgement
- Total bacteria and Staphylococcus loads have been correlated with pain perception in women’s breast
- Decreasing breastmilk microbiota directly relates to pain symptoms
Reference
Maldonado-Lobon JA, et al., 2015
Additional Information on Postmastectomy Pain Syndrome (PMPS)
Treatment Related Risk Factors
- More extensive surgery in the axilla
- Radiation therapy
- Tumor localization in the upper lateral quarter
- Radiotherapy
- Tumor diameter
- Tumor grade
- Estrogen and progesterone receptor status
- Amount of removed sentinel node
- Amount of removed lymph node
- Lymphedema
- Preoperative neoadjuvant Chemotherapy
- Postoperative chemotherapy
- Postoperative hormone therapy
- Adjuvant treatment
- Surgery type
- Analgesic treatment
Reference
Andersen KG,et a., 2015; Beyaz SG,et al., 2016; Caviggioli, F, et al., 2016
Etiology of Chronic Pain
- Chemotherapy agents can play, as role as: Taxanes, platinum agents, and vinca alkaloids are neurotoxic
- Endocrine therapy may prompt musculoskeletal pain and arthralgia
- Infections, seroma, and hematoma may aid in the development of persistent pain altering physiological scarring
Reference
Caviggioli F, et al., 2016
Areas of Pain and Discomfort Among Breast Cancer Survivors
N = 147
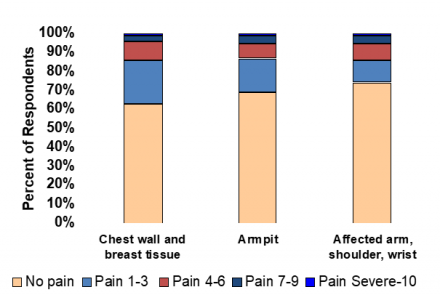
Reference
Bosompra K, et al., 2002
Frozen Shoulder
- Temporary loss of range of motion in the shoulder
- Typically occurs when the shoulder has been immobilized for a long period of time (i.e. surgery)
- A shoulder becomes frozen when: the shoulder is immobile, the capsule surrounding the glenohumeral joint (the main ball and socket of the shoulder) thickens and contracts causing it to stiffen
- The shoulder may remain immobile to avoid pain.
- The less the shoulder is moved the more likely it is that the capsule will contract and stiffen
Typical Candidates for Frozen Shoulder
- Typically occurs when individuals who undergo surgery and do not receive exercise therapy following their procedure
Treatment for Frozen Shoulder
- Visit expert or clinical for physical exam
- May receive x-ray/MRI to rule out other possible conditions
- Anti-inflammatory medications may be prescribed
- Most important treatment is physical therapy to stretch the joint capsule
Reference
How to release a frozen shoulder, 2004

