Child Bearing Related Breast Pain
- Pain during pregnancy
- Pain during lactation
- Sore Nipples
- Ineffective attachment
- Short frenulum
Pain During Pregnancy
- Discomfort and pain can be caused by oversupply of milk and persistent breast engorgement
- Pregnancy-induced gigantomastia (Rare)
- Excessive engorgement
- Breast enlargement is likely hormonal
- Can result in tissue necrosis and infection
- Thought to be related to breast tissue hypersensitivity to hormonal influences
Reference
Berens PD, 2015
Pain During Lactation
- Pressure during breastfeeding is normal
- Pain during breastfeeding is not
- According to the CDC, exclusive breastfeeding rates drop 59.8% by 6 months postpartum
- Main cause of decline is painful nipples and persistent nipple pain
- Breastfeeding can lead to nipple problems such as the development of microscopic lesions
- Lesions occur on the nipples and the areola
- May appear as wounds, fissures, eroded skin, erythema, edema, white or yellow blisters, dark spots, and ecchymosis
- Breastfeeding can lead to nipple problems such as the development of microscopic lesions
- Main cause of decline is painful nipples and persistent nipple pain
Reference
CDC , 2011; Shanazi M, et al., 2015; Kent JC, et al. , 2015; Dennis CL, Jackson K, & Watson J, 2014
Reasons Women Reported Weaning
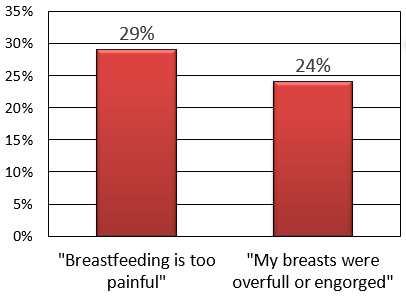
Sharon Seeks Help from Dr. Spatz
Reasons for Lactation Pain
Mothers reporting:
- Sore, cracked, or bleeding nipples
- Baby having trouble latching
- Breastfeeding as “too painful”
Are less likely to meet breastfeeding goals.
Pain is Not Normal
Sore Nipples
Most commonly due to nipple trauma (Traumatic Nipples):
- Multiple causes related to improper breastfeeding technique or poor attachment (see Sore Nipple Etiologies)
- For most women, the greatest nipple pain intensity seems to happen between 3-7 days postpartum
- Persistent nipple pain can cause psychological distress. It can interfere with:
- Sleep
- Activities
- Mood
- Mother/child bonding
- May lead to deprivation of breast milk
Reference
Shanazi M, et al., 2015; Kent JC, et al. , 2015
Additional Information on Treatments for Sore Nipples
From the Breast Feeding Centre of Western Australia.
| Sore Nipples Treatments | Discussion |
|---|---|
| Correct Positioning and attachment |
|
| Improving Latch |
|
| Nipple Shields |
|
| Anhydrous Lanolin/Vitamin A Ointments |
|
| Frentomy for Ankyloglossia |
|
| Warm Compress |
|
| Antibiotics/Antifungal |
|
| Avoiding Irritants/Topical Corticosteroid Ointment |
|
| Warmth/ Avoidance of Vasoconstrictors/Prescriptions for Nifedipine |
|
Reference
Kent JC, et al., 2015; Berens PD, 2015
Topical Treatments for Sore Nipples
| Herbal Treatment | Discussion |
|---|---|
| Lanolin |
|
| Dexphanthenol |
|
| Peppermint |
|
Reference
Shanazi M, et al., 2015; Kent JC, et al., 2015
Treatment of Sore Nipples
Treatment for traumatic nipple pain has shown to be complicated because of the repeated sucking on the nipples by the infant
- Constant exposure of the nipple skin to the infant’s oral flora
- Microorganisms enter through the nipple fissures
- Cause infections
Reference
Shanazi M, et al., 2015
Pain Decrease by Treatment Type
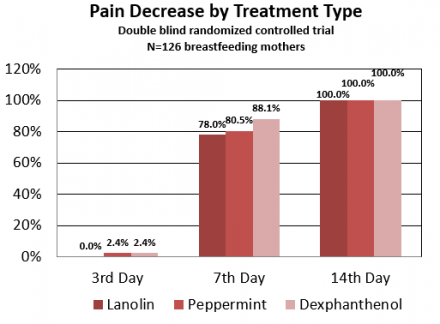
Pain Treatments
Dr. Spatz explains treatments for nipple pain.
Lanolin Treatment
Dr. Spatz explains more about lanolin treatment for sore nipples.
Reference
Shanazi M, et al., 2015
Treatment of Lactation Pain
- Effective early lactation management is vital to avoid early weaning or breastfeeding cessation
- Early detection in intervention helps to prevent ongoing pain and psychological distress
- Herbal medicines have been used to help with pain
Medication Treatment
Dr. Spatz discusses medication treatment for lactation pain with Sharon.
Reference
Shanazi M, et al., 2015; Kent JC, et al., 2015
Ineffective Attachment
First, watch what effective attachment looks like.
Now, listen to Dr. Spatz describe the effects of ineffective attachment.
Dr. Spatz describes how a nipple shield can help address ineffective attachment.
Short Frenulum
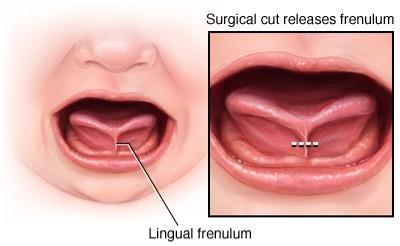
http://www.mayoclinic.org/
Dr. Spatz checks Sharon's baby for a short frenulum.
Mastitis
Mastitis is an inflammatory condition in the breast, often associated with lactation, occurring in women of all ages.
- Sometimes milk stasis is the cause of mastitis
- Sometimes associated with infection
- Onsite of mastitis is often sudden
- Mastitis commonly occurs during early postpartum period
Definition of Mastitis
Dr. Spatz tells Shanita about the definition of mastitis.
Mastitis Prevention
Dr. Spatz tells Shanita different ways to prevent mastitis.
Reference
Maldonado-Lobon JA, et al., 2015; Berens PD, 2015; Afshariani R, et al., 2014
Incidence of Mastitis
- 3%-33% of breastfeeding women will develop lactational mastitis.
- Can be associated with infection.

http://www.mayoclinic.org/diseases-conditions/mastitis/basics/definition/con-20026633
Most breast infections occur in breastfeeding women when bacteria enters the breast through cracks in the nipple. In severe infections, abscesses may occur.
Reference
Maldonado-Lobon JA, et al., 2015; Berens PD, 2015; Afshariani R, et al., 2014
Mastitis and Medical Reason for Early Weaning
- Mastitis and painful breastfeeding may be linked to mammary bacterial dysbiosis.
- Potential pathogens increase at the expense of the normal mammary microbiota
- Most organisms causing infections come from the infant’s oropharynx or nasal passage
- Potential pathogens increase at the expense of the normal mammary microbiota
- Mastitis is the main medical reason for early weaning
Reference
Maldonado-Lobon, J. A., et al., 2015; Berens, P. D. , 2015
Mastitis Risk Factors
- Factors that inhibit adequate drainage of the gland/plugged ducts
- Poor infant attachment
- Sore nipples
- Nipple trauma that allows for organisms to enter
- Mastitis with prior breastfeeding experiences
- Using breast pumps/manual pumps
- Nipple cracks
- Recent use of antifungal creams
Follow-up Visit for Mastitis
Shanita returns to Dr. Spatz with pain.
Reference
Maldonado-Lobon JA, et al., 2015; Berens PD, 2015
Complications of Mastitis
- Cessation of breastfeeding
- Breast tissue injury
- Breast abscess
- Recurrence
- Pain
- Illness
Reference
Afshariani R, et al., 2014
Treatment Considerations for Mastitis
- Pain and inflammation control is a vital component to treating mastitis
- Treatment should be started immediately
- Inflammation control is vital because painful breasts could prevent mother from removing milk effectively or feeding their baby
- This could lead to further complications of mastitis
Treatment of Mastitis
Dr. Spatz tells Shanita about treatment options for mastitis.
Antibiotics for Mastitis
Dr. Spatz goes over the use of antibiotics to treat mastitis with Shanita.
Reference
Afshariani R, et al., 2014

