More information on orofacial pain, temporomandibular disorders, trigeminal neuralgia, and persistent idiopathic facial pain.
Pain Classification
Simple
- Anatomic location: where pain is felt
- Subjective complaint: important to guide the diagnostic process
Complex
- Advanced knowledge of pain behavior
- Heterotopic pain: when the site of the pain is not in the same location as the source of the pain
- Central excitatory effects: diagnostic differentiation between true primary pain and symptoms that occur as secondary effects from that pain
Involves physical conditions and psychological comorbidities
Pain
Physical Conditions
Orofacial structures
- Cutaneous and mucogingival tissues
- Pharynx, nose and paranasal sinuses
- Dental
- Musculoskeletal structures of the mouth and face
- Visceral structures of the mouth and face
- Neural structures of the mouth and face
Psychological Comorbidities
Produce or influence the pain experience
- Anxiety disorders
- Mood disorders
- Somatic symptom and related disorders
- Psychological factors related to health condition(s)
Orofacial pain
Orofacial pain (OFP)
- Acute and chronic conditions
- Approximately 25% of general population
Chronic orofacial pain
- Painful regional syndromes with a chronic, unremitting pattern
- Approximately 10% of OFP cases
Differential Diagnosis of Chronic Orofacial Pain
Musculoskeletal pain
- Temporomandibular disorders (TMD)
Neuropathic pain
- Trigeminal Neuralgia
- Persistent Idiopathic Facial Pain
Neurovascular pain*
- Most common types are Trigeminal Autonomic Cephalgias
- Migraine
*Basis of pain is representative of both neurological and vascular elements
Differential Diagnosis of Orofacial Pain
- Intracranial pain
- Headaches
- Neuropathic pain
- Intraoral pain
- Temporomandibular disorders
- Cervical pain
- Pain related to anatomically associated structures
- Referred pain
- Psychiatric and mental illness
Reference
Sarlani E, et al. AACN Clinical Issues 2005, Kumar A, et al. Dent Clin North Am 2013
Intracranial Pain
- Tumors (benign or malignant)
- Aneurysm
- Intracranial bleeding (hemorrhage or hematoma)
- Intracranial swelling or edema
- Abscess or infection
Reference
Kumar A, et al. Dent Clin North Am 2013
Neuropathic Pain
Episodic
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
Continuous
- Post-herpetic neuralgia
- Pain resulting from trauma (aberrant healing of nerve tissue or development of neuromas)
- Burning mouth syndrome
- Atypical odontalgia
- Persistent idiopathic facial pain / atypical facial pain
Reference
De Rossi SS. Dent Clin North Am 2013, Hupp W, et al. Dent Clin North Am 2013, Kumar A, et al. Dent Clin North Am 2013
Intraoral Pain
Dentition
- Dentin sensitivity, caries, pulpal disease
Periodontium
- Gingivitis, acute or chronic periodontal disease, sensitivity related to recession or alveolar bone pathology
Other soft and hard tissues
- Caused by mucosal diseases, neoplasms, or pain related to parafunction or trauma
Reference
Napenas JJ. Dent Clin North Am 2013, Kumar A, et al. Dent Clin North Am 2013
Temporomandibular Disorders
Temporomandibular disorders, or TMDs, are a common source of orofacial pain in the general population. Literature suggests that 75% of the general population will develop one sign of TMD, most notably TMJ clicking. Literature also suggests that 33% of the population will develop one symptom associated with TMD, most notably pain. It is important to rule out other etiologies for orofacial pain that may mimic TMD signs and symptoms. It is important to rule out dental etiology as a source of orofacial pain, including dental decay, especially those teeth involving the pulp and/or nerve tissue, and gum or periodontal abscesses that may cause referred pain to the TMD structures.
Neuropathic pain, most commonly described as electric shock-like pain, may mimic TMD symptoms. However, it is most associated with trigeminal neuralgia. In addition, patients may also describe chronic burning pain, which may be associated with the condition persistent idiopathic facial pain, or atypical odontalgia. Oral mucosal disease can be a source of orofacial pain and patients can develop oral ulcers secondary to trauma, to infection, immune-mediated disorders, and/or potentially cancerous lesions.
Finally, odologic complaints, such as ear disorder and/or sinus complaints, may also represent signs and symptoms that are similar to temporomandibular disorders. It is important to consider referral to the appropriate healthcare provider for further evaluation and management to rule out these other etiologies that may mimic TMD.
TMD Facts and Figures
- TMD in the adult U.S. population
- 40% -75% have at least 1 sign
- Ex: jaw clicking but no pain or disturbance to quality of life
- 33% have at least 1 symptom
- Ex: pain in the TMJ area
- 40% -75% have at least 1 sign
- Only 5 – 10% with TMD will require active treatment
- May require multimodal therapy and interdisciplinary care
- Most common between 20 – 50 years of age
- Female > Male
- Some experts consider being female as a risk factor for TMD
Signs and Symptoms Associated With TMDs
- Facial / jaw / mouth pain
- Earache / ear pain
- Throat pain
- Headache / head pain
- Neck pain
- Shoulder pain
*Patients often have been evaluated by multiple health care providers without evidence of site-specific pathology
TMD Evaluation
- TMD - Focused History
- Onset of symptoms
- History of trauma
- Type / quality of pain
- Timing of pain
- Pain with jaw function / types of food
- History of click / pop / crunch sounds
- History of parafunctional habit (clenching / grinding)
- History of jaw locking
- Comorbid conditions
- Evaluations / diagnoses / treatments to date
Comorbid Conditions Which May Impact TMDs
- Centrally Acting
- Fibromyalgia
- Widespread pain
- Headache
- Anxiety
- Depression
- Sleep disturbance
- Peripherally Acting
- Parafunctional habit
- Postural tension
- Trauma
Comorbid Conditions and TMDs
- Increased risk of progressing from acute to chronic TMD
- Delayed or incomplete recovery with standard TMD treatments
- May affect central pain mechanisms / regulation
- May act peripherally to cause direct muscle / TMJ injury
- Should be addressed and integrated into treatment plan
TMD Clinical Examination
- Consider Cranial Nerve Examination
- Mandibular range of motion
- Inter-incisal opening
- Lateral and protrusive movements
- Mandibular deviation
- Auscultation of the TMJ
- Listening for joint noises
- Palpation of the TMJ
- Feeling if joint area is tender/sore
- Palpation of the muscles of mastication
- Feeling if muscles are tender/sore
TMD Clinical Exam
TMJ Articular Disc Disorders
Malpositioning of the articular disc relative to the condyle and articular eminence
With reduction
- The disc resumes its normal position on top of the condyle on opening without restricted mouth opening
Without reduction
- The disc remains mal-positioned on opening attempts, resulting in restricted mouth opening in acute cases
- “TMJ closed lock”
Subluxation (hypermobility)
- An overextension of the disc–condyle complex on opening beyond the articular eminence with ability to return to a normal jaw position
- “Jaw overextension”
Joint dislocation
- A dislocation of the entire disc–condyle complex beyond the articular eminence combined with inability to return to a normal jaw position
- “TMJ open lock”
Etiologies for TMJ Articular Disc Disorders
- Trauma
- Macrotrauma
- Direct injury
- Dental procedures
- Macrotrauma
- Microtrauma
- Application of prolonged forces on TMD complex
- Indirect trauma
- Whiplash injuries
TMJ Arthritic Disorders
- Osteoarthritis
- AKA “Degenerative Joint Disease”
- Non- to Low-inflammatory arthritic disorder
- Active bony changes
- Etiology
- Mechanical overloading of the articular surfaces leads to degeneration of articular cartilage
- History
- Unilateral joint pain aggravated by jaw movement
Exam
- Limited opening (typically <35mm)
- Crepitus (crunching sound)
- Pain on palpation of the joint
Imaging
- Changes to mandibular condyle
- Shape change / remodeling of bone
- Possible bone spurring
- Bone surface irregularities not normally observed
Rheumatoid arthritis
- Persistent inflammation in the joint leads to destruction of articular surfaces and bone
- Autoimmune disorder
- Similar clinical symptoms to TMJ osteoarthritis
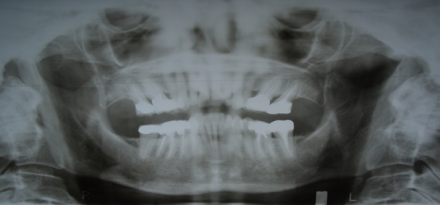
TMJ Imaging Considerations
- Plain film imaging
- Panoramic radiograph
- Advanced imaging
- Computed tomography (CT)
- Cone-beam CT (CBCT)
- Medical CT
- Magnetic resonance imaging (MRI)
- Computed tomography (CT)
Management of TMDs
- Pharmacotherapy
- Physical therapy
- Appliance therapy
- Trigger point injections
- Complementary and alternative medicine
- Invasive procedures
Trigeminal Neuralgia (TGN)
- General prevalence
- 0.01% to 0.3%
- Gender distribution
- Females > Males (2:1)
- Age of onset
- > 40 years of age
- Peak incidence
- 50 to 60 years of age
Classic TGN Signs and Symptoms
- Excruciating pain
- “Electric–like”
- Trigger areas
- Extra-oral
- Intraoral
- Short duration
- Latency
- Multiple episodes
- Refractory Period
- Unilateral
- Condition typically affects one side of the face
- Branches of the trigeminal nerve commonly affected
- Maxillary (V2)
- Mandibular (V3)
Clinical Evaluation of Suspected TGN
- Patient-reported symptoms
- Cranial nerve examination
- Physical exam findings
- Dental imaging
- Rule out odontogenic and / or local pathology
- Advanced imaging of CNS
- Rule out vascular compression of TGN nerve root
- Rule out CNS tumor
Medical Management of TGN
- Carbamazepine
- Oxcarbazepine
- Lamotrigine
- Baclofen
- Phenytoin
- Gabapentin
- Pregabalin
Surgical Management of TGN
- Peripheral Procedures
- Neurectomy
- Cryotherapy
- Injections
- Alcohol
- Glycerol
- Risk of neuropathic pain
- Central Procedures
- Microvascular decompression
- Gamma knife surgery
- Percutaneous trigeminal rhizolysis
Persistent Idiopathic Facial Pain (PIFP)
Also referred to as Atypical Odontalgia; Atypical facial pain
- General prevalence
- 0.03% to 1.0%
- Gender distribution
- Females > Males
- Age of Onset
- 40 to 60 years of age
PIFP Signs and Symptoms
- Persistent nature
- Poorly localized
- Does not follow nerve distribution
- Quality of pain
- Burning
- Aggravated by stress
- Onset may be associated with trauma
- Dental interventions unsuccessful
- Absence of clinical neurologic deficit / identification of local pathology
Clinical Evaluation of Suspected PIFP
- Patient-reported symptoms
- Cranial nerve examination
- Physical exam findings
- Local anesthetic nerve block
- Dental imaging
- Rule out odontogenic and / or local pathology
- Advanced imaging of CNS (if indicated)
- Rule out CNS pathology
Management of PIFP
- Patient reassurance
- Behavioral medicine
- Pharmacologic agents
- Tricyclic antidepressants
- Amitriptyline, Nortriptyline
- Anticonvulsants
- Gabapentin, Pregabalin
- Serotonin-Norepinephrine Re-uptake Inhibitors
- Duloxetine
- Analgesics, topical lidocaine
- Tricyclic antidepressants
Conclusions
- Orofacial pain disorders are often complex
- Range of symptoms
- Profound impact on quality of life
- Requires comprehensive evaluation
- Evidence-based approach to management
- Evolving process
- Multidisciplinary care

