Diana is seen for pelvic pain but also complains of morning jaw pain and difficulty getting her teeth together at times.
She is referred for a dental evaluation of her jaw pain.
OPQRST
Questions you might want to ask Diana specifically about her jaw pain are:
O - When did the pain start? Is it getting better or worse?
P - What aggravates the symptoms? Makes them better? What do you do when you have the symptoms?
Q - Please describe your jaw pain.
R - Where is the jaw pain? Does it radiate anywhere?
S - How intense is the pain?
T - How often? How long does it last?
Diana's Dental History
Additional Questions to Ask Diana to Evaluate for the Presence of a Temporomandibular Disorder (TMD)
- Do you have pain in or around the ears, temples, or cheeks?
- Do you have frequent headaches and/or neck aches?
- Have you had a recent injury to your head, neck, or jaw?
- Have you previously been treated for a TMD problem?
- Do your jaws regularly feel stiff, tight, or tired?
- Do you have difficulty or pain when opening your jaw?
- Does your jaw get stuck or locked?
- Do you have difficulty or pain when chewing, talking, or using your jaw?
- Are you aware of noises in your jaw joints?
- Have you ever been treated for a jaw pain problem?
You may ask Diana these questions to assess her pain, range of motion (ROM), and jaw function. If the patient is pain-free and does not have limited ROM, consider other orofacial pain disorders such as neuralgia, tooth pain, headache, etc.
Diana's History of Present Illness
- Diana points to her right TMJ area as the location of her jaw pain. It seemed to start at the time of her orthodontic treatment 6 years ago. At the time, her orthodontist told her that her symptoms would lessen after her malocclusion was corrected. Unfortunately, her jaw dysfunction symptoms have persisted and in past year seem to be more common.
- She describes the symptoms as a dull, aching pain presenting 3-4 mornings a week. Her jaw feels tight every morning until it loosens up mid-morning. On the mornings that she has pain, her symptoms can present throughout the day.
- She states that on days her pelvic pain bothers her, her jaw pain “acts up” as well.
- 3-4 days a week the jaw pain presents as a dull, aching pain at a 3-5 of 10 that can worsen as the day progresses.
- Sometimes she takes Tylenol (acetaminophen, one 325 mg tablet) that can decrease her jaw pain a little.
- She used to have a loud click many mornings after awakening, but now she just hears a softer click or noise when opening or moving her jaw side to side.
- She states that she can’t seem to get her teeth to fit together as well as she used to. Her left-side, back teeth don’t contact very well.
- She has not had any specific treatment or evaluation for her jaw pain.
TMJ Exam
Diana’s provider examines her jaw function to evaluate her temporomandibular disorder (TMD).
TMD Differential Diagnosis
Temporomandibular Disorders
A subgroup of craniofacial pain disorders that encompass a group of musculoskeletal and neuromuscular conditions that involve:
- The temporomandibular joint
- The masticatory muscles
- Associated head and neck structures
Temporomandibular disorders also include:
- Masticatory muscle disorders
- TM Joint articular disorders
- Congenital and developmental disorders
- Chronic mandibular hypomobility
- Hypermobility (subluxation/dislocation
Reference
de Leeuw R, Klasser GD (ed.): Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management. The American Academy of Orofacial Pain, 5th Edition, Quintessence Publishing Co., Inc., 2013.
Temporomandibular Joint Articular Disorders
- Congenital or developmental
- Aplasia
- Hypoplasia
- Hyperplasia
- Joint Pain
- Arthralgia
- Arthritis
- Joint Disorders
- Disc-condyle Complex Disorders
- Other Hypomobility Disorders – Adhesions, Ankylosis
- Hypermobility Disorders – Subluxation, Dislocation
- Joint Diseases
- Degenerative Joint Diseases – Osteo-arthritis (painful)/arthrosis(non painful)
- Condylysis – Idiopathic Condylar Resorption (ICR)
- Osteonecrosis
- Systemic Arthritides – Rheumatoid Arthritis (RA), Ankylozing Spondylitis (AS) , Rieter’s Syndrome, etc.
- Neoplasm
- Synovial Chondromatosis (joint mice)
- Fractures
Reference
Kalaykova SI, Klitsie AT, Visscher CM, Naeije M, Lobbezoo F. A Retrospective Study on Possible Predictive Factors for Long-term Temporomandibular Joint Degeneration and Impaired Mobility in Juvenile Arthritis Patients.J Oral Facial Pain Headache. 2017 Spring;31(2):165-171. doi: 10.11607/ofph.1656. PMID:28437514
Diagnosing and Managing Arthritides in a TMD Patient
How to Test for Rheumatoid Disease (RA)
References for detailed protocol:
- Viller F1, Guillemin F, Briançon S, Moum T, Suurmeijer T, van den Heuvel W . Compliance with drug therapy in rheumatoid arthritis. A longitudinal European study. Joint Bone Spine. 2000;67(3):178-82.
- Schiffman E, Braun B, Lindgren B. Temporomandibular joint iontophoresis: a double blind randomized clinical trial. J Orofacial Pain 10:157-165, 1996. PMID:9133860
- Lobbezoo F, Drangsholt M, Peck C, et al. Topical review: New insights into the pathology and diagnosis of disorders of the temporomandibular joint. J Orofac Pain 18(3):181-190, 2004 PMID: 15508997
- Bakke M, Zak M, Jensen BL. Orofacial pain, jaw function, and temporomandibular disorders in women with a history of juvenile chronic arthritis or persistent juvenile chronic arthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. Oct;92(4):406-14, 2001 PMID: 11598575 DOI: 10.1067/moe.2001.115467
- Appelgren A, Appelgren B, Ericksson S, Kopp S, Lundeberg T, Nylander M, Therodorsson E. Neuropeptides in the arthritic TMJ and symptoms and signs from the stomatognathic system with special consideration to rheumatoid arthritis. J Orofacial Pain. 9:215-225, 1995. PMID: 1722347
- Westhoff G1, Zink A. Basic treatment of early rheumatoid arthritis. Abstaining from rheumatological care and preferring alternative medicine increase the risk of undertreatment. Z Rheumatol. 2007 Mar;66(2):121-4, 126-8 PMID: 17334734 DOI: 10.1007/s00393-007-0153-9
Epidemiology of RA Influencing TMJ Function
Studies shows that 30% of RA patient will develop symptomatic TMJs (arthralgia).
How Does RA Treatment Fit Into the Overall Patient’s Treatment Plan?
Treatment involves control of the systemic arthritide coupled with standard TMD therapy.
Masticatory Muscle Disorders
- Muscle Pain Limited to the Orofacial Region
- Myalgia
- Tendonitis
- Myositis
- Spasm
- Myofibrotic Contracture
- Hypertrophy
- Neoplasms
- Movement Disorders – dyskinesia/dystonia
- Masticatory Muscle Pain Due to Systemic/Central Disorders
Reference
de Leeuw R, Klasser GD (ed.): Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management. The American Academy of Orofacial Pain, 5th Edition, Quintessence Publishing Co., Inc., 2013.
TMD Examination
3-part protocol
- Range of Motion
- Palpation
- Auscultation
Differential for decreased range of motion (ROM)
- Myalgia (myofascial pain)
- Disc displacement
- Muscle spasm
- Myositis
- Contracture
- Cranial nerve deficit
Vertical ROM is measured between the ends of the upper and lower anterior teeth.

Reference
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications..J Oral Facial Pain Headache. 2014 Winter;28(1):6-27. doi: 10.11607/jop.1151.PMID: 24482784
Temporomandibular Joint (TMJ) Patterns of Jaw Opening

TMJ patterns of opening include:
- Normal function
- DD with reduction
- DD w/o reduction
- osteoarthritis
The TMJ begins to translate at about 20 mm of jaw opening. If there is a disc displacement (DD), the jaw opening will deviate to the affected side giving an S shape to the opening pattern. If the displaced disc reduces (DD with reduction) the mandible will go back to midline (see arrow). If the disc does not reduce, the mandible will remain displaced to the affected side giving the diagnosis of DD without reduction. The “jerky” opening on the far right depicts a pattern consistent with a TMJ with arthritic changes in the joint which commonly is associated with course crepitus.
Reference
Image from: Fricton JR, Kroening RJ, Hathaway KM: TMJ and Craniofacial Pain: Diagnosis and Management. St. Louis, 1988, Ishiyaku EuroAmerica Inc.pg 46 Figure 5.5 (out of print, permission granted by author)
TMD Exam: TMJ Arthralgia Diagnosis
To confirm diagnosis, the patient must have preauricular pain with at least two of these three maneuvers:
- Palpation
- ROM
- Joint Loading (upwards and/or distal pressure on the mandible)

References
- Stegenga B, Lambert G, De Bont, Boering HG. Osteoarthrosis as the cause of craniomandibular pain and dysfunction: a unifying concept. J Oral Maxillofac Surg. 47: 249-256,1989.
- Schiffman E, Ohrbach R, Truelove E, Look J, Anderson, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMDConsortium Network* and Orofacial Pain Special Interest Group†.J Oral Facial Pain Headache. 2014 Winter;28(1):6-27. doi: 10.11607/jop.1151.PMID: 24482784
Myofascial Pain Diagnosis
The most common TMD diagnosis.
- Dull aching pain
- Somewhat limited ROM
- Trigger point (TP)
- Hypersensitive area
- Referred pain from the TP
- Ability to passively stretch the jaw further open
Consider downloading the Apple application for iPhone and iPad “Muscle Trigger Points” written by Read Bodywork Medical.
Reference
Wright EF. Referred craniofacial pain patterns in patients with temporomandibular disorder. J Am Dent Assoc. 2000;131(9):1307-15. http://www.ncbi.nlm.nih.gov/pubmed/?term=10986831
Diana’s Occlusal Exam
Diana's Occlusion Frontal View

Occlusal Contacts with the Use of Articulator Paper
The blue marks on the teeth indicate occlusal contacts via the use of articulator paper.

Shimstock Measurement
Measurement of occlusal contacts with the use of shimstock which is thinner than the patient can proprioceptively discern between her/his teeth (see small blue arrow) note open posterior bite on the patient ‘s left.

Mandibular Occlusal Appliance
Diana’s mandibular occlusal appliance which provides even contact on her posterior teeth bilaterally. She can wear this during the day to determine how a stable occlusion affects her symptoms.

Summary of Diana’s TMD/ Jaw Function Examination
- When asked to point to where her symptoms are, she points to just beneath her right TMJ.
- When asked to open as far as she can without any pain or tightness, she opens to 2 finger tips (approximately 30 mm).
- When asked to open as far as she can with pain or discomfort, she opened to 3 finger tips+ (+ 40 mm) and pointed to her right TMJ as the location of her discomfort.
- When moving her jaw laterally, she could move her mandible well to the right but was limited in her ability to move her jaw to the left.
- She had a mild discomfort in her right TMJ area with lateral jaw movement; when she was asked to move her jaw side-to-side on two tongue blades, she did not notice this discomfort.
Significance of Diana’s lateral ROM of her jaw findings:
- Her limited ROM to the left indicates decreased translation of the right condyle, possibly related to a anteriorly –medially displaced articular disc on the right side.
- The right TMJ exhibits arthralgia from capsulitis. When the patient moves side-to-side on a tongue blade, the increase in space in the joint does not allow compression of the inflamed tissues. Would a similar test relieve pain of a rt lateral pterygoid problem?
Summary of Diana’s Head and Neck Exam

- The patient’s head and neck palpation examination revealed two positive findings (exam was otherwise negative):
- Palpation of the right deep masseter area was positive. It was a familiar pain that referred to her ear and felt like her jaw and ear pain, duplicating her Chief Complaint (CC) of dull, aching jaw pain.
- Palpation of the right splenius capitis referred pain to her vertex. This was familiar pain to her, but the referral to her head was not familiar pain for her.
Summary of Diana’s Jaw Function Tests
- Diana's jaw clench test was negative. Biting on a unilateral tongue blade placed over her left molar teeth brought on right TMJ jaw pain. This pain was relieved when she bit on tongue blades placed over both her right and left molar teeth.
The jaw clench test indicates whether a patient’s symptoms can be associated with night and/or daytime parafunction. If this duplicates the patient’s symptoms, one can predict that parafunction is an etiologic factor for the patient’s symptoms. If the clenching symptoms dissipate when clenching on tongue blades placed bilaterally over the patient’s posterior teeth (not allowing the muscles to completely contract), night-time appliance therapy and/or diurnal habit control should limit parafunction and decrease symptoms.
A unilateral tongue blade clench test discerns between a joint-based or muscle-based etiology. This test unloads the ipsilateral joint while contracting the ipsilateral muscles. Accordingly, if the patient experiences same-side pain, one should consider a muscle problem; if the test elicits an contra-lateral TMJ pain, one should consider contra-lateral TMJ arthralgia.
- When asked to bite down on a piece of shimstock and resist it from being pulled from between her teeth, she was only able to hold the shimstock between her teeth when it was placed over her right molars and 2nd bicuspid teeth. What is the significance of these findings?
Shimstock “holding” indicates a definitive occlusal contact between opposing teeth. Diana only has contact on one side of her occlusion indicating occlusal instability. This finding is most likely related to the osteoarthritis in her Rt TMJ causing thinning of the superior surface of her right condyle, which promotes a clock-wise rotation of the mandible seating the condyle, and creating a hyper-occlusion on the right and posterior open bite on the left, i.e., occlusal instability.
- Diana had a positive rotational stretch test and a positive 2- finger stretch test with the discomfort /tightness again just beneath her right TMJ. After placing an ice pack over her right area of complaint and stretching her jaw open, this jaw-opening tightness dissipated. What is the significance of these findings?
The cold pack decreases nociception to lessen the discomfort from increasing painful ROM. The rotational stretch stretches the deep masseter muscle and unloads the TMJ, while the finger
stretch stretches the superficial masseter, medial pterygoid, and temporalis muscles. A positive stretch test indicates that the exercise should be part of the patient’s PT regimen and should
lead to increased pain-free ROM of the jaw.
Diana's Imaging
A panograph (screening image) was taken showing moderate-to-severe osseous changes to the right TMJ condyle with flattening of the anterior superior surface of condylar head. The articular eminence was intact and WNL.
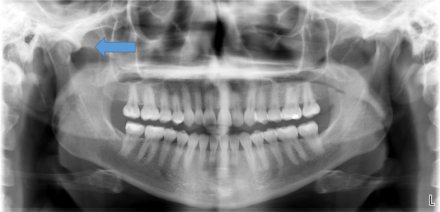
Due to the osseous changes observed in the “screening” panograph in her right TMJ, a CT scan was ordered as a more definitive evaluation and to provide a baseline exam should she continue to have occlusal (bite) changes and/or jaw function problems.
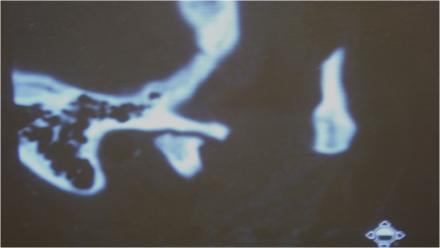
A panograph is the standard of care as a screening radiograph for a TMD or orofacial pain consult. If it reveals osseous changes to the joint, a CT scan should be taken as a baseline from which to assess future changes to the joint. Soft tissue changes to the joint and articular disc position is best documented with an MRI. Effusions, a sign of inflammation, is best evaluated with a T2 weighted MRI.
References for Imaging
- Shaefer J, Jackson D, Schiffman E, Anderson Q (2001). Pressure-pain thresholds and MRI effusions in TMJ arthralgia. J Dent Res, 80(10): 1935-1938.
- Stenks M, Bleys R, Witkamp T (1994) Temporomandibular joint structures: a comparison between anatomic and magnetic resonance findings in a coronal and an angulated coronal plane. J of Orofac Pain 8:4, 335-348, 1994
- Shaefer JR, Riley CJ, Keith D J of Dental Research Analysis of Criteria for MRI Diagnosis of TMJ Disc Displacement and Arthralgia, International Journal of Dentistry, 2012, Article ID 283163, 8 pages, 2012. doi:10.1155/2012/283163.
- DaSilva A, Shaefer J, Keith D. The Temporomandibular Joint: Clinical and Surgical Aspects.Neuroimag Clin N Am 13 (2003) 573-582
Diana's Jaw Pain Assessment and Treatment Plan
- Diagnoses of right TMJ degenerative joint disease (DJD), right deep masseter myofascial pain, and occlusal instability were made.
- A self-care regimen to include jaw range of motion exercises was explained to the patient.
- A non-steroidal anti-inflammatory drug (NSAID) regimen and muscle relaxant regimen were prescribed. She is also taking a trial of suppressive hormonal therapy for her pelvic pain.
- An occlusal appliance was ordered.
- She was also given deep breathing exercises to help reduce acute pain.
Jaw Range of Motion and Stretch Exercises
Watch the video to see how Diana should complete her range of motion and stretch exercises.
Ice Pack therapy and Stretch Exercises
Watch the video to see how Diana should complete her ice pack therapy to help complete her stretch exercises.
Goal of TMD Treatment
The goal of TMD treatment is to improve pain-free jaw ROM while giving the patient control of her TMD symptoms with the use of reversible therapies.
What is Standard TMD therapy?
Physical therapy (PT), appliance therapy, home exercise programs, behavioral therapy, control of parafunctional habits (such as bruxism and daytime clenching), and medication use (analgesics, sleep medications, muscle relaxants, anxiolytics) should be considered routine for initial TMD therapy.
References
- Fricton JR. Clinical care for myofascial pain. Dent Clin North Am. 1991 Jan;35(1):1-28. Review. PubMed PMID: 1997346
- List T, Axelsson S. Management of TMD: evidence from systematic reviews and meta-analyses. J Oral Rehabil. 2010 May;37(6):430-51. doi: 10.1111/j.1365-2842.2010.02089.x. Epub 2010 Apr 20. Review. PubMed PMID:20438615.
- Cairns BE. Pathophysiology of TMD pain--basic mechanisms and their implications for pharmacotherapy. J Oral Rehabil. 2010 May;37(6):391-410. doi:10.1111/j.1365-2842.2010.02074.x. Epub 2010 Mar 10. Review. PubMed PMID:20337865.
- Nitzan D. Intraarticular pressure in the functioning Human temporomandibular Joint and its alteration by uniform elevation of the occlusal plane. J Oral Maxillofac Surg 52:671-679, 1994.
- Okesan J, The effects of hard and soft splints on nocturnal bruxism. J Am Dent Assoc. 114:788, 1987.
- Okeson, J.P., Kemper, J.T., Moody, P.M. A study of the use of occlusion splints in the treatment of acute and chronic patients with craniomandibular disorders. Journal of Prosthetic Dentistry. 48(6): 708-712, 1982.
Example TMD Multi-modal Treatment Plan
| Treatment | Examples and Treatment Descriptions |
|---|---|
| Home exercise program | Exercises to increase ROM within pain tolerance |
| Physical therapy | Modalities to reduce pain, develop exercise regimen 2-3 x per week. Ensure treatment compliance |
| NSAIDS | To control acute myalgia symptoms; 600-800 mg ibuprofen TID, 10-day regimen for arthralgia |
| Neuropathic medications (can also help with sleep) | Consider gabapentin, pregabalin, amitriptyline 10-30 mg HS |
| Muscle relaxants | Cyclobenzaprine (Flexeril) 5-10 mg TID |
| Anxiolytics | Consider anti-anxiety medication, if indicated |
| Occlusal appliance | Mandibular stabilization appliance providing even bit to control night-time parafunction and provide stable (even) occlusion bilaterally on posterior teeth. It can be worn during the day to assess the role of unstable occlusion in TMD symptoms |
| Injections; trigger point injections (TPIs), nerve blocks, Botox | If unresponsive to standard therapy and pain is localized to masticatory myofascial trigger points, consider TPIs. If pain is more regional and/or neuropathic, consider nerve blocks |
| Behavioral therapy | Cognitive behavioral therapy, relaxation training, mental health evaluation |
| Hypnosis, acupuncture, laser |
Medications Effective for TMD
Some examples include:
- non-steroidal anti-inflammatory drugs (NSAIDs) or other analgesics for acute pain episodes;
- muscle relaxants for acute muscle pain;
- sleep medications can help control night-time parafunction;
- a 10-day regimen of anti-inflammatory medication (NSAIDs) or a Medrol (steroid) dose pack for TMJ arthralgia
References
- Tchivileva IE, Lim PF, Smith SB, Slade GD, Diatchenko L, McLean SA, Maixner W. Effect of catechol-O-methyltransferase polymorphism on response to propranolol therapy in chronic musculoskeletal pain: a randomized, double-blind, placebo-controlled, crossover pilot study. Pharmacogenet Genomics. 2010 Apr;20(4):239-48. doi: 10.1097/FPC.0b013e328337f9ab. PubMed PMID: 20216107; PubMed Central PMCID: PMC2876724.
- Mujakperuo HR, Watson M, Morrison R, Macfarlane TV. Pharmacological interventions for pain in patients with temporomandibular disorders. Cochrane Database Syst Rev. 2010 Oct 6;(10):CD004715. doi: 10.1002/14651858.CD004715.pub2. Review. PubMed PMID: 20927737.
- Herman CR, Schiffman EL, Look JO, Rindal DB. The effectiveness of adding pharmacologic treatment with clonazepam or cyclobenzaprine to patient education and self-care for the treatment of jaw pain upon awakening: a randomized clinical trial. J Orofac Pain. 2002 Winter;16(1):64-70. PubMed PMID: 11889661.
- Annaswamy TM, De Luigi AJ, O'Neill BJ, Keole N, Berbrayer D. Emerging concepts in the treatment of myofascial pain: a review of medications, modalities, and needle-based interventions. PM R. 2011 Oct;3(10):940-61. doi:10.1016/j.pmrj.2011.06.013. Review. PubMed PMID: 22024326.
When Physical Therapy (PT) and Behavioral Therapy is Indicated for TMD
Initially, the patient’s response to a home regimen designed to promote an increase in pain-free ROM via exercises and control of parafunctional habits is assessed. In cases with persistent pain (e.g., pain score > 5/10) and/or significant neck pain influencing the jaw pain, PT and behavioral therapy (e.g., cognitive behavioral techniques, stress reduction, etc.) are indicated. PT and behavioral therapy should be included in all complex TMD cases (severe pain, chronic pain with functional limitations, significant co-morbidities).
References
- De Laat A, Stappaerts K, Papy S. Counseling and physical therapy as treatment for myofascial pain of the masticatory system. J Orofac Pain. 2003 Winter;17(1):42-9. PubMed PMID: 12756930.
- Carlson CR, Bertrand PM, Ehrlich AD, Maxwell AW, Burton RG. Physical self-regulation training for the management of temporomandibular disorders. J Orofac Pain. 2001 Winter;15(1):47-55. PubMed PMID: 11889647.
- Truelove E, Huggins KH, Manel L, Dworkin SF. The efficacy of traditional, low-cost and nonsplint therapies for tempormandibualr disorder: randomized controlled trail. JADA (137) 1099-1107, 2006
- Turk D, Zaki H, Rudy R. Effects of intraoral appliance and biofeedback /stress management alone and in combination in treating pain and depression in patients with temporomandibular disorders.JPD. 70:158-164,1993.
Success to Expect from TMD Treatment
Evidence indicates that 80% of patients with TMD will respond to standard TMD therapy. For the 20% who do not respond, ensure the following:
- the correct diagnosis has been made
- the patient is complying with the treatment plan
- all contributing factors are being addressed
References
- Ohrbach R, Fillingim RB, Mulkey F, Gonzalez Y, Gordon S, Gremillion H, Lim PF, Ribeiro-Dasilva M, Greenspan JD, Knott C, Maixner W, Slade G. Clinical findings and pain symptoms as potential risk factors for chronic TMD: descriptive data and empirically identified domains from the OPPERA case-control study. J Pain. 2011 Nov;12(11 Suppl):T27-45. doi: 10.1016/j.jpain.2011.09.001. PubMed PMID: 22074750; PubMed Central PMCID: PMC3443556.
- Fricton JR. Clinical care for myofascial pain. Dent Clin North Am. 1991 Jan;35(1):1-28. Review. PubMed PMID: 1997346.
- Rammelsberg P, LeResche L, Dworkin S, Mancl L. Longitudinal outcome of temporomandibular disorders: a 5-year epidemiologic study of muscle disorders defined by research diagnostic criteria for temporomandibular disorders. J Orofac Pain. 2003 Winter;17(1):9-20. PubMed PMID: 12756926.

