
General Principles
- Comprehensive assessment of pain
- Clear communication between all team members, including the patient/family
- Follow relevant pharmacologic principles
- Understand tolerance issues
- Investigate and clarify problematic behavior and difficulty progressing care
- Consider multidisciplinary consultation (mental health, addiction, pain, social work, spiritual care, etc.)
Reference
Laroche F, Rostaing S, Aubrun F, Perrot S. Pain management in heroin and cocaine users. Joint Bone Spine 2012;79(5). PMID:22405747 DOI:10.1016/j.jbspin.2012.01.007
Paschkis Z, Potter ML, CE: Acute pain management for inpatients with opioid use disorder. Am J Nurs 2015;115(9). PMID:26273927 DOI:10.1097/01.NAJ.0000471243.30951.92
Stromer W, Michaeli K, Sandner-Kiesling A. Perioperative pain therapy in opioid abuse, Eur J Anaesthesiol 2013;30(2). PMID: 23241915 DOI:10.1097/EJA.0b013e32835b822b
Interdisciplinary Team
Pain management in patients with the disease of addiction begins with an interdisciplinary team approach. The team can address the multiple needs and problems that can occur while managing such a patient. Verifying patient behaviors with other team members is helpful for assessing aberrancy.
Team discussion can be used to individualize treatment plans, establish limit-setting and help staff understand behaviors they may view as manipulative. Conflict with staff may be lessened if there is a general understanding of realistic goals.
Consistency and Communication
- Don’t make promises you can’t keep!
- Commit to care for patient’s pain
- Decide to use multiple therapies besides opioids
- Assure adequate dosing
- Empathize with clear limit setting (depersonalize)
- Adopt and convey non-judgmental attitude
- Gather a care conference (may be needed several times a day)
Understanding the Experience of Addiction
- Substance use may start as a choice, but addiction leads to loss of control
- Patients use substances to relieve distress and feel “normal”
- Affects all life roles and relationships, including medical encounters
- Patients may not be seeking treatment for addiction, complicating relationships with providers, who clearly see negative consequences.
- Can result in mutual mistrust
Reference
Merrill JO JGIM 2002 Mutual Mistrust
Screening for Substance Use
- Ask permission to discuss this sensitive topic
-
- “Can I ask you some questions about your substance use?”
- Be specific and detailed
-
- “What do you use? - cocaine, meth, heroin, pills?”
- How much and how often?
-
- “When did you last use?”
- Ask about withdrawal symptoms
-
- “What symptoms do you usually feel when in withdrawal?”
Reference
Kilbourne AM, Salloum I, Dausey D, Cornelius JR, Conigliaro J, Xu X, Pincus HA. Quality of care for substance use disorders in patients with serious mental illness. J Subst Abuse Treat. 2006;30(1):73-7. PMID: 16377454 DOI:10.1016/j.jsat.2005.10.003
Getting an Addiction History
- Establish rapport – listen to the story
- Use open ended questions in non-judgmental fashion
-
- A patient may feel shame, guilt and fear (fear of pain and withdrawal)
- Ask about past use – it is less threatening
- Assess past problems and treatment attempts
- Listen for and reflect concerns about bias, stigma, problems with medical care
- Listen for a “recovery story”
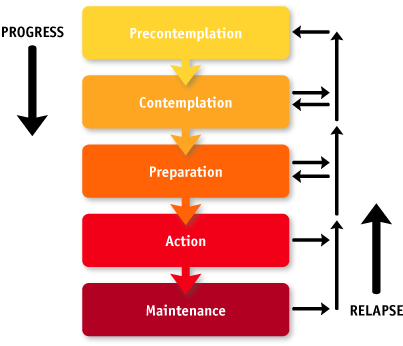
Access Stage of Readiness to Change
Reference
DiClemente, C. C. , & Prochaska, J. O. (1998). Toward a comprehensive, transtheoretical model of change: Stages of change and addictive behaviors. In W. R. Miller & N. Heather (Eds.), Treating addictive behaviors (2nd ed., pp. 3-24). New York: Plenum.
Using Opioids for Acute Pain in Patients with OUD
- High doses of opioids might be necessary due to tolerance
- Respect tolerance but don’t let it drive dosing
-
- Opioid tolerant may need 2-3X usual doses
- Short-acting opioids are platform for acute pain
- A schedule may be beneficial for all involved
- Oral preferred; if parenteral is needed, consider using IV PCA
-
- Avoid prn RN boluses
- Can set lockouts to 90 minutes
- Disentangle from non-opioids
Reference
Carroll IR, Angst MS, Clark JD. Management of perioperative pain in patients chronically consuming opioids. Reg Anesth Pain Manag 2004;29(6):576-591. PMID:15635517
Richebe P, Beaulieu P. Perioperative pain management in the patient treated with opioids: continuing professional development, Can J Anesth 2009;56(12):969-81. PMID:19888637 DOI:10.1007/s12630-009-9202-y
Shah S, Kapoor S, Durkin B. Analgesic management of acute pain in the opioid-tolerant patient. Curr Opin Anaesthesiol 2015;28(4):398-402. PMID:26107026 DOI:10.1097/ACO.0000000000000218
Addiction Maintenance Therapy
- Methadone and buprenorphine are used in addiction maintenance programs to prevent craving
- Methadone maintenance therapy can only be provided by Opioid Treatment Programs certified by the federal government
- Buprenorphine is approved for in-office treatment of opioid dependence
Methadone maintenance programs, available since the 1960s, have been found to reduce heroin use and the crime, death and disease associated with abuse of the drug. Methadone reduces craving and suppresses withdrawal symptoms. When used to treat pain, it is usually dosed every 6-8 hours, whereas when used in addiction maintenance programs, it is dosed once a day. Outpatient maintenance treatment can only be provided by Opioid Treatment Programs (OTPs) certified by the Substance Abuse and Mental Health Services Administration and registered by the DEA. OTPs should also provide a comprehensive range of medical care, drug and health education and counseling.
Buprenorphine offers an alternative to methadone and is subject to fewer prescribing restrictions. This Schedule III drug was approved for in-office treatment of opioid dependence under the Federal Drug Addiction Treatment Act of 2002. Buprenorphine may be prescribed by any physician who has received training (available via the internet or as a oneday course) and receives an additional prescribing number from the DEA. Buprenorphine is available in sublingual tablets both alone and with naloxone.
Individuals in either treatment program are at risk for inadequate pain control, but for different reasons. Clinicians may fail to recognize that patients in OTPs may have developed significant tolerance and require “larger than expected” doses of opioid to control pain. The challenge with buprenorphine is that it acts as an antagonist at high doses and thus could block the analgesic effect of an opioid agonist such as morphine or hydromorphone.
Reference
Bonhomme J, Shim RS, Gooden R, Tyus D, Rust G. Opioid addiction and abuse in primary care practice: a comparison of methadone and buprenorphine as treatment options. J Natl Med Assoc 2012;104(7-8):342-350. PMID: 23092049 PMCID:PMC4039205
Methadone
- Patients who are admitted on methadone dispensed from addiction treatment centers should continue to receive the same daily dose while in the hospital
- Once daily methadone for addiction treatment will not treat acute pain
- Methadone has an unpredictable long half-life and should not be increased or added to treat acute pain
- Consult an addiction or pain specialist for advice and regulations
Reference
Noska A, Mohan A, Wakeman S, Rich J, Boutwell A. Managing opioid use disorder during and after acute hospitalization: a case-based review clarifying methadone regulation for acute care settings. J Addict Behav Ther Rehabil 2015;4(2):PMID: 26258153 PMCID: PMC4527170 DOI:10.4172/2324-9005.1000138
Shanahan C, Beers D, Alford DP, Brigandi E, Samet JH, A transitional opioid program to engage hospitalized drug users.J Gen Intern Med 2010;25(8):803-808. PMID:20237960 PMCID:PMC2896583 DOI:10.1007/s11606-010-1311-3
Buprenorphine
- Used for analgesia or office based maintenance therapy with special license
- Can be used for pain control. Variable analgesic effect
- Binds very tightly to m-receptor; high dose blocks effect of pure agonists
- Can precipitate opioid withdrawal due to partial agonist effect
- Limited respiratory depression risk, so safer than full agonists
- Less risk of prolonging the QT interval than methadone
Reference
Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med 2006;144(2):127-134. PMID:16418412 PMCID:PMC1892816
Bonhomme J, Shim RS, Gooden R, Tyus D, Rust G. Opioid addiction and abuse in primary care practice: a comparison of methadone and buprenorphine as treatment options. J Natl Med Assoc2012;104(7-8):342-350. PMID:23092049 PMCID:PMC4039205
Bryson EO The perioperative management of patients maintained on medications used to manage opioid addiction. Curr Opin Anesthesiol 2014;27:359-364. PMID: 24500338 DOI:10.1097/ACO.0000000000000052
Substance Use in Hospital
What should you do if a patient could be using while in the hospital?
- Document and communicate aberrancies
- Move forward with prompt, clear, definitive response
- Hold opioids until intoxication signs have resolved and UDT obtained
- Change opioids to low diversion potential form (e.g. oral solution)
- Review and document
- Inform the patient of risk and consequences
- Advise others involved in patient’s care
- Ensure withdrawal symptoms have been adequately addressed
Care Coordination at Hospital Discharge
- Early discharge planning is crucial to identify transition plan, particularly for patients planning to engage with on-going addiction treatment
- It is illegal for inpatient provider to provide methadone for opioid use disorder (maintenance therapy) at discharge.
-
- An exception known as the "three-day rule"
-
- Title 21, Code of Federal Regulations, Part 1306.07(b)), allows a practitioner who is not separately registered as a narcotic treatment program, to administer (but not prescribe) narcotic drugs to a patient for the purpose of relieving acute withdrawal symptoms while arranging for the patient’s referral for treatment
- Not more than one day’s medication may be administered to a patient at one time
- This treatment may not be carried out for more than 72 hours
Reference
Noska A, Mohan A, Wakeman S, Rich J, Boutwell A. Managing opioid use disorder during and after acute hospitalization: a case-based review clarifying methadone regulation for acute care settings. J Addict Behav Ther Rehabil 2015;4(2):PMID: 26258153 PMCID:PMC4527170 DOI:10.4172/2324- 9005.1000138
Shanahan C, Beers D, Alford DP, Brigandi E, Samet JH, A transitional opioid program to engage hospitalized drug users.J Gen Intern Med 2010;25(8):803-808. PMID:20237960 PMCID:PMC2896583 DOI:10.1007/s11606-010-1311-3
Naloxone Prescription for Potential Outpatient Opioid Overdose
Persons at risk for opioid overdose should be given a prescription for naloxone when they leave the hospital. This may include persons:
- With a history of receiving emergency medical care for acute opioid poisoning or overdose
- A suspected history of substance abuse or nonmedical opioid use
- Receiving high-dose opioid prescriptions (e.g. >100 mg morphine equivalent)
- Who are opioid naïve and receiving a first prescription for methadone for pain
- Starting buprenorphine or methadone for addiction treatment
- On opioid prescriptions for pain in combination with:
-
- Smoking, COPD, emphysema, sleep apnea, or other respiratory illness
- Renal dysfunction, hepatic disease, or cardiac disease
- Known or suspected alcohol use
- Concurrent benzodiazepine or other sedative prescription
- Concurrent antidepressant prescription
- Who may have difficulty accessing emergency medical services
- Voluntary request by person or agency
For Patients Likely to Go Back to Using Heroin
- Patients who came to the hospital actively using will likely return to active use
- Methadone administered in hospital can be abruptly discontinued
- Provide no more than 3 days of opioids to treat acute pain at discharge; some with none
- Provide naloxone emergency overdose kit

