
Harold’s car was broadsided on the driver side by a vehicle running a red light. Both front and side airbags deployed.
Harold's Initial Stats
- HR: 136
- BP: 82/40
- RR: 32
- Pulse-ox: 88
- Radial pulses were palpable but weak
- Harold was slipping in and out of consciousness, but was able to tell the EMT that he had pain in his left leg and left chest and was having difficulty breathing
Harold's Trauma
Harold is air lifted to the trauma center.
Harold's Health History
Past Medical History:
- Mild depression
- Opioid use disorder: Oxycodone
Hospitalizations:
- 4 week inpatient drug rehabilitation stay for opioid use disorder
Allergies:
- No known drug or food allergies
Family History:
- Family history of substance use disorder
Social History:
- + Tobacco: 2 packs per day for 20 years (40 pack years)
Past Medications:
- Ibuprofen PRN
- Buprenorphine/naloxone (Suboxone®)
Harold's Initial Triage
Harold tells the trauma care team he can't breathe. After they start a four-liter nasal cannula, they continue the initial survey.
Harold's Pain Assessment
While Harold complains of pain, he's able to move every portion of his body when asked by the trauma team.
Interprofessional Care
The Chaplain arrives to support Harold’s wife. She is understandably distraught and tells the chaplain that Harold is taking buprenorphine and naloxone (brand name Suboxone). She provides an account of Harold’s substance use disorder and expresses concerns about Harold receiving any opioids for his pain.
Trauma Critical Care Unit
Dr. Black is concerned wth Harold's breathing and wants to keep him in the Trauma Critical Care Unit overnight for observation.
The trauma team comprised of physicians, nurses and a pharmacist discuss Harold’s plan of care that includes frequent assessment of his pain, administration of multimodal analgesia, and frequent monitoring to evaluate his response to treatment and observe for an adverse events from analgesics. The team anticipates that he will be transferred to the general care trauma unit the next day.
Meet Harold
With Harold in the Critical Care Unit for observation, let's take time to learn more about him, in his own words.
Meet Janice
With Harold in the Critical Care Unit for observation, let's take time to learn more about his wife, Janice.
Harold's Substance Abuse
Harold's wife Janice tells us more about Harold's substance abuse.
Harold's Rehabilitation
Harold's wife Janice tells us more about his rehabilitation.
Does Harold Have Mild, Moderate, or Severe Opioid Use Disorder (OUD)?
Using the table below, see how many criteria for Opioid Use Disorder Harold displays. Click either "yes" or "no" depending on whether you believe Harold exhibits the criteria referenced.
The number of criteria a patient meets determines the severity of OUD:
- Mild OUD: 2-3 criteria
- Moderate OUD: 4-5 criteria
- Severe OUD: 6-7+ criteria
Harold meets the following criteria for Opioid Use Disorder:
Opioid taken in larger amounts or over a longer period than intended:
Harold told his doctor he needed more oxycodone to make him feel "good." Harold stated he needed more oxycodone to get him through the day.
Persistent desire or unsuccessful efforts to cut down or control opioid use :
Harold mentions he would "do anything to continue to have that high."
A lot of time spent obtaining, using, or recovering from the effects of the opioids:
Harold admitted having times when he felt "out of it," and would even doze off at work.
Craving or a strong desire to use opioids:
Harold said he would "do anything to continue to have that high," which increased his craving for opioids.
Recurrent opioid use resulting in a failure to fulfill major role obligations at work, school, or home:
As a result of misusing and abusing opioids, Harold was often feeling drowsy and "out of it," irritable and angry. He almost lost his job and his relationship with his wife.
Continued use despite persistent or recurring social or interpersonal problems caused or exacerbated by opioid use:
Harold and his wife argued frequently about his opioid misuse and abuse, but he still continued to misuse and abuse prescription opioids.
Continued use despite knowledge of having persistent or recurrent physical or psychological problems caused or worsened by opioid use.
Harold continued to hid and misuse opioids despite the constant arguments between him and his wife.
Tolerance as defined by either a need for markedly increased amounts to achieve intoxication or desired effect or by markedly diminished effect with continued use of the same amount (does not apply when used appropriately under medical supervision):
Harold needed to take more pills each day to continue to feel euphoric, and he was exhibiting signs of tolerance.
Harold does not meet the following criteria for Opioid Use Disorder:
Stopping or reducing important social, occupational, or recreational activities due to opioid use.
Recurrent use of opioids in physically hazardous situations.
Withdrawal manifesting as either characteristic syndrome or the substance is used to avoid withdrawal (does not apply when used appropriately under medical supervision).
Harold Has Severe Opioid Use Disorder
Harold has 8 criteria for opioid use disorder. (Severe opioid use disorder is characterized as having 6-7+ criteria)
Harold's Emergency Pain Management
Pharmacotherapy
The following discusses appropriate pharmacotherapy for Harold's emergency pain management:
Opioids
Harold's emergent and critical care plan could include intravenous opioids, including fentanyl, morphine, or hydromorphone*.
*Opioid Adverse Effects:
- May produce a euphoric effect, while some patients may feel dysphoria
- Opioid use over time may induce physical dependence
- If stopped abruptly, the patient will experience withdrawal symptoms such as flu-like symptoms and pain
Acetaminophen
Harold should receive acetaminophen. Acetaminophen is a nonopioid analgesic that can be used as part of multimodal analgesia, and is not known to cause physical dependence.
Regional anesthesia
Harold could receive an ankle block to allow for early mobilization with assisted devices to prevent further injury. A block using bupivacaine could last approximately 18 hours. See below for more.
Codeine
Codeine is not the best choice for acute pain. It has variable metabolism, which creates unpredictable efficacy and is a weak synthetic opioid with little to no benefit to patients like Harold. Learn more about codeine.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Harold should receive NSAIDs. Because of his history with OUD, NSAIDs can be used as part of multimodal analgesia to reduce requirements for opioids.
Adjuvant drugs
Harold should receive adjuvant analgesics such as anti-convulsant medications as part of multimodal analgesia or antidepressants. Gabapentin is a commonly used anti-convulsant medicaton to treat pain. Alternatives include pregabalin, duloxetine, tricyclic anti-depressants (e.g., amitriptyline).
Tramadol
Harold should not receive tramadol. It is a weak mu opioid agonist for management of mild to moderate acute and chronic pain and should be avoided because of variable metabolism. It also has other serotonergic pathways. Because tramadol can lead to dependence, it should be avoided in patients with a history of substance use disorder.
Ankle Block
An ankle block is used to provide temporary relief from pain.

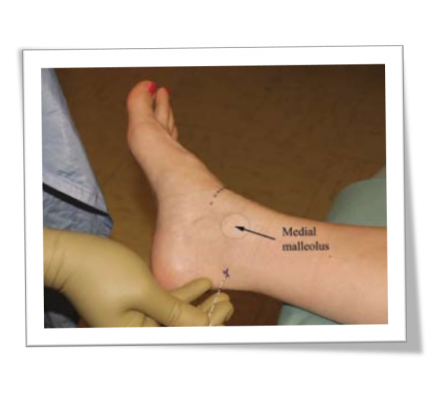
Images courtesy of Defense and Veterans Center for Integrative Pain Management (DVCIPM): Ankle Block. dvcipm.org. https://www.dvcipm.org/site/assets/files/1083/chapt22.pdf. Published 2018. Accessed July 26, 2018.
Reference:
Dever C. Treating acute pain in the opiate-dependent patient. J Trauma Nurs. 2017;24(5):292-299. CDC Guideline for Prescribing Opioids for Chronic Pain | Drug Overdose | CDC Injury Center. cdc.gov. https://www.cdc.gov/drugoverdose/prescribing/guideline.html. Published 2018. Accessed July 26, 2018. Sporer KA. Buprenorphine: A primer for emergency physicians. Ann Emerg Med. 2004;43(5):580-584. Ahmadi A, et al. Pain management in trauma: A review study. J Inj Violence Res. 2016;8(2)89-98. Chou R, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2)113-130.
Multimodal Analgesia
The schematic shows representation of multimodal analgesia and the actions of classes of analgesics on peripheral and central pain pathways.
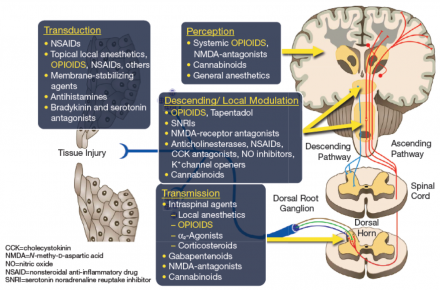
Transduction
NSAIDs, topical local anesthetics, opioids, others.
Transmission
Intraspinal agents, local anesthetics, opioids, gabapentinoids.
Descending/Local Modulation
Opioids, tramadol.
Perception
Systemic opioids, general anesthesia.
Reference:
Adapted from "Opioid Therapies and Cytochrome P450 Interactions," by Jeffrey Gudin, 2018, Journal of Pain and Symptom Management, figure 1. Adapted with permission.

