Joyce Discusses Substance Use Disorder with Addiction Specialist
Signs and Symptoms of Opioid Withdrawal
- Tachycardia
- Hypertension
- Hyperthermia
- Insomnia
- Mydriasis
- Hyperreflexia
- Diaphoresis
- Piloerection
- Increased respiratory rate
- Lacrimation
- Yawning
- Muscle spasms
- Rhinorrhea
- Abdominal cramps
- Nausea/vomiting
- Diarrhea
- Anxiety
- Arthalgias/myalgias
How to Decide Level of Care For a Patient with Opioid Use Disorder
- Largely based on patient preference and psychosocial factors
- Some questions you may want to ask:
- Are you actively using or in withdrawal?
- Have you been enrolled in either inpatient or outpatient chemical dependency programs in the past?
- Do you have a safe place to live?
- Do you have transportation?
- Can consult the American Society of Addiction Medicine (ASAM) continuum
Levels of Care
- Detoxification
- Brief medically monitored setting for patients actively using, or in active withdrawal
- Outpatient Chemical Dependency treatment program
- Enrollment (usually 3-4 appointments)
- Intake
- Orientation
- Medical Screening
- Medical Therapy (if buprenorphine program)
- Requirements
- Regular attendance at group sessions (usually 3-5 per week)
- Inpatient Chemical Dependency treatment program (highest level of care)
- Typically 14-28 days
Medication Assisted Therapy (MAT)
- Naltrexone
- Available orally or Intramuscularly (IM)
- IM preferred when using for outpatient opioid use disorder treatment; lasts 30 days
- Requires 10 day confirmed “washout” period with no exposure to opioids
- Available orally or Intramuscularly (IM)
- Buprenorphine
- Sublingual tablets or strips
- Available alone, or in abuse deterrent preparations (naloxone containing)
- Naloxone is not bioavailable (doesn’t have any effect) when administered sublingually as prescribed. It is active only if injected intravenously.
- Can be prescribed in the hospital by any provider
- As of July 2019, requires an DEA x-waiver to be prescribed for outpatient treatment of opioid use disorder.
- Can be prescribed in the outpatient setting off-label for pain control by a provider without an x-waiver.
- Methadone
- Requires daily administration at an outpatient methadone program
- Cannot be prescribed for outpatient treatment of opioid use disorder
- Requires screening laboratory tests and EKG
- MAT is most effective when paired with regular chemical dependency counseling and psychotherapy
Starting Buprenorphine
- Starting buprenorphine is called a “buprenorphine induction”
- Buprenorphine is a partial opioid agonist with high affinity
- Could precipitate acute withdrawal if administered in a patient actively using, or recently took a long acting opioid (e.g., methadone, oxymorphone)
- Safe induction is performed in mild to moderate opioid withdrawal
- A helpful clinical decision tool is the Clinical Opioid Withdrawal Score
- Available at MDCALC1
- Induction can be done in the emergency department
Clinical Diagnosis of Uncomplicated Opioid Withdrawal
Based on history and physical exam.
Image
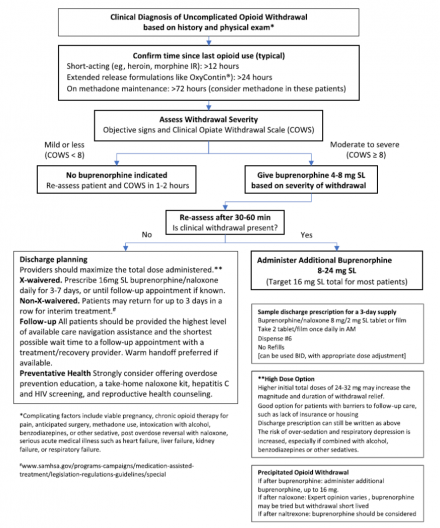
Reference
Herring AA, et al. Managing Opioid Withdrawal in the Emergency Department With Buprenorphine. Ann Emerg Med 2019; 73(5):481–487. doi:10.1016/j.annemergmed.2018.11.032.
Continuing Buprenorphine
- Continuing buprenorphine at discharge after an emergency department or the hospital induction is called “bridging,” or “a bridging prescription”
- Requires a DEA x-waiver
- If no x-waivered providers are available, same day or next day follow-up at an inpatient or outpatient treatment facility is necessary
- Patients discharged with interrupted or no access to buprenorphine or treatment otherwise will have a very high rate of relapse
- Ideally, the patient is “bridged” seamlessly to an inpatient or outpatient provider with a “warm handoff” (appointment with a provider or program who is expecting them)
Prescription Monitoring Program
- All prescription writing healthcare providers should have access prescription monitoring program
- Check a patient’s prescription record on the state prescription monitoring program prior to prescribing any opioid medication, including buprenorphine
- Depending on the state, you may need to perform an advanced search to check prescriptions provided to your patients in another state
- Identify patients at risk for polypharmacy
- Identify patients who have developed opioid use disorder
- The PMP provides useful information about a patient’s success or continued struggle with medication assisted therapy
Joyce Meets with the Pharmacist
Buprenorphine (BUP)/Naloxone Sublingual Film (Suboxone)
- Indications
- Pain
- Opioid use disorder (OUD)
- Pharmacokinetics
- Onset of action: 30-60 min
- Duration of analgesia: 6-8 hrs.
- Half-life: 24-42 hrs.
BUP Patient Counseling Pearls
- Take exactly as prescribed
- Unwrap film and place it under tongue
- Keep it in place ~10 minutes until it is dissolved
- Do not chew or swallow film
- Avoid eating or drinking for ~15 minutes before and after administration
- May notice some temporary numbness, tingling, and/or redness where the film is placed in the mouth
Prescribing information for buprenorphine sublingual film.
BUP Adverse Effects
- Orthostatic hypotension
- Dizziness
- Drowsiness
- Headache
- Glossodynia
- Oral hypoesthesia
- Inattention
- Diaphoresis
- Nausea/vomiting
- Constipation
- Pruritis
- Oral mucosal erythema
- Insomnia
Naloxone (Narcan®) Nasal Spray
- Indication
- Reversal of opioid overdose
- Commercially available as 4mg/0.1ml nasal spray (NS)
- Pharmacokinetics:
- Onset of action: 5-13 minutes
- Duration of action: 30-120 minutes
- Well tolerated medication with minimal adverse effects
- Not harmful to administer if unclear why patient is sedated
Signs and Symptoms of Opioid Overdose
- Unconsciousness
- Unresponsive to painful stimuli
- Miosis
- Slow/shallow respirations
- Respiratory rate < 8-10 breaths/min
- Cyanotic lips and/or nail beds
- Bradycardia
- Diaphoretic/clammy skin
Naloxone NS Patient Counseling
- Assess patient for signs and symptoms of opioid overdose
- Remove nasal spray from the package
- Insert tip of nasal spray into one of the patient’s nostrils and press plunger
- Move patient onto their side (in case of vomiting)
- Give another dose of naloxone if patient does not respond after 2-3 minutes
- Call for emergency medical services

