Luisa is referred to physical therapy as one of the non-pharmacological strategies to help her manage her acute neck pain.
At this event, we will look at outcome measures, subjective report, physical therapy interview with and without a medical interpreter, objective evaluation and examination, assessment, and physical therapy plan of care.
Physical Therapy – Outcome Measures
The first step of the physical therapy initial evaluation is completion of outcome measures. We will look at three main areas of information about pain and function which will include a body diagram for pain location, faces pain scale revised for pain intensity, and neck disability index for pain and function.
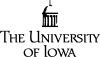
Body Diagram
The body diagram demonstrates pain in the upper back, posterior neck and base of the head.
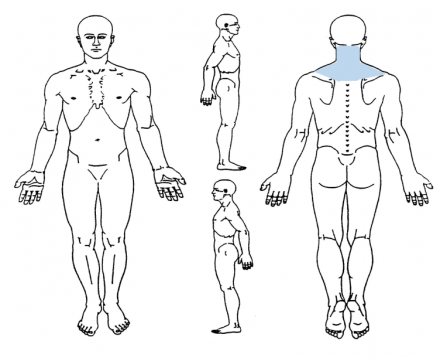
Faces Pain Scale
Luisa rates her pain for three areas: present pain 6 of 10, best 2 of 10 and worst 8 of 10.
Luisa's Pain
Luisa rates her pain for three areas: present pain 6 of 10, best 2 of 10 and worst 8 of 10.
Reference
Pain Manag Nurs. 2006 Sep; 7(3):117-25.Evaluatio of the Revised Faces Pain Scale, Verbal Descriptor Scale, Numeric Rating Scale, and Iowa Pain Thermometer in older minority adults. Used with permission from IASP. For clinical, educational, or research purposes, use of the FPS-R is free of charge, and permission for use is not needed, provided that the scale is not modified or altered in any way. https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1519&navItemNumber=577 (Access to multiple languages on download link)
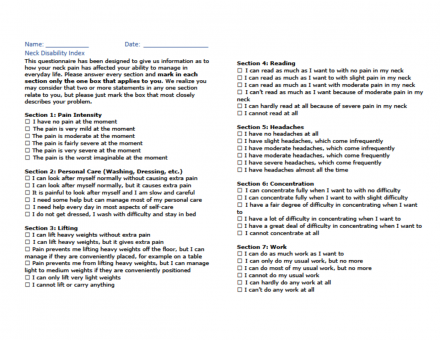
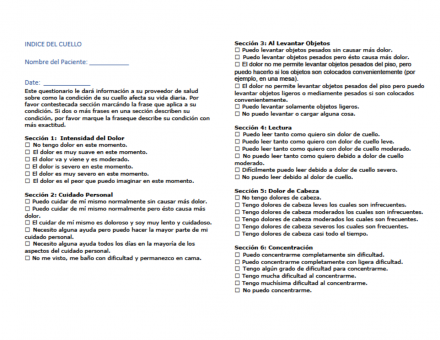
Neck Disability Index (NDI)
The Neck Disability Index (NDI) was developed by Vernon, H. & Mior, S. in 1991. This tool is used to determine the impact of pain and function.
Luisa’s NDI score is 34/50 or 68% disability at this initial physical therapy visit.
Physical Therapy Subjective Report
Luisa’s subjective report includes her background and subjective patient report.
Past Medical History
History of hypocholesteremia, hypertension, and osteoarthritis in neck, shoulders and back. Patient is a previous smoker and occasional drinker.
Living Environment
Patient lives in a one-story home with her husband and one daughter and 2 grandchildren.
Demographics
Patient is Hispanic, primarily Spanish speaking, high school education.
Social History
Patient is a homemaker. She participates in bowling once a week, plays cards and helps care for 2 grandchildren by driving them to/from school each day. Patient is left hand dominant.
Patient Complaint
Patient reports pain in her posterior neck after making tamales for two days to get ready for an event at church 3 weeks ago. She reports stiffness and pain are increased in the morning and difficulty turning her head during daily activities, especially driving and looking down; difficulty getting comfortable at night due to neck discomfort. She is normally involved in social activities of bowling and caring for her grandchildren and is not able to complete these at this time due to discomfort. Pain aggravated by neck and head motion, laying down on her side and driving. Pain relief noted with use of heat and laying on her back at home. Patient notes headache occasionally at the end of the day.
Patient notes she sleeps on her sides and has not been able sleep in that position for more than 2 hours due to neck pain. Patient denies any numbness or tingling in neck or upper quarter. She notes no previous injury to neck or upper back. Patient was referred to physical therapy by her primary physician. Patient notes she has been using intermittent Tylenol without a significant change in her pain.
Patient Goals
Return to driving, return to church activities, caring for grandchildren, playing cards, bowling and looking down to be able to read the newspaper.
Neck Disability Index
Spanish Version of the Neck Disability Index completed with a score of 68% disability.
Subjective
Patient is a 69-year-old female with primary complaint of neck pain which began 3 weeks ago after making tamales for two days.
Physical Therapy – Interview– Without Interpreter
Physical Therapy – Interview– With Interpreter
Physical Therapy – Objective and Assessment
System Review
Please review the system review below for Luisa.
Cardiopulmonary
HR 72, sPO2 98%, BP 124/72
Integument
No visible redness, warmth or scar in upper quarter
Musculoskeletal and Neurological
See ROM and Strength
Objective Information
Posture
Patient presents with moderate forward head and rounded shoulders with left greater than right. Patient with increased lumbar lordosis and increased thoracic kyphosis. Patient with limited head motion during subjective history and discussion.
Muscle Length and Flexibility
Patient with moderate tightness in bilateral pectoralis major and minor, left biceps musculature.
Sensation
WNL to light touch bilateral upper extremity dermatomes; patient denies numbness and tingling.
Palpation
Patient with marked muscle guarding in bilateral upper trapezius, anterior and middle scalene and sternocleidomastoid. Patient with moderate guarding in scapular musculature and posterior cervical musculature.
Physical Therapy – Objective
Cervical
Abbreviations: WNL = within normal limits; WFL = Within functional limits
| Motion and Strength | AROM | PROM | Muscle Test Grade | Comments |
|---|---|---|---|---|
| Flexion | 35 | 45 | 3 | In available ROM; pain at end range |
| Extension | 5 | 10 | 2+ | In available ROM; pain at end range |
| Lateral flexion - Right | 15 | 20 | 3 | In available ROM; pain at end range |
| Lateral flexion - Left | 10 | 15 | 3 | In available ROM; pain at end range |
| Rotation - Right | 25 | 35 | 3 | In available ROM; pain at end range |
| Rotation - Left | 15 | 20 | 3 | In available ROM; pain at end rang |
Upper Extremity Range of Motion
Abbreviations: WNL = within normal limits; WFL = Within functional limits
Shoulder
| Motion and Strength | AROM | PROM | Muscle Test Grade |
|---|---|---|---|
| Flexion - Right | WFL | WFL | 4+ |
| Flexion - Left | WFL | WFL | 5 |
| Extension - Right | WFL | WFL | 5 |
| Extension - Left | WFL | WFL | 5 |
| External Rotation - Right | WFL | WFL | 4+ |
| External Rotation - Left | WFL | WFL | 4 |
| Internal Rotation - Right | WFL | WFL | 4+ |
Elbow
| Motion and Strength | AROM | PROM | Muscle Test Grade |
|---|---|---|---|
| Flexion and Extension | WNL | WNL | 5 |
Wrist
| Motion and Strength | AROM | PROM | Muscle Test Grade |
|---|---|---|---|
| Flexion | WNL | WNL | 5 |
| Extension | WNL | WNL | 5 |
Grip
| Motion and Strength | AROM | PROM | Muscle Test Grade |
|---|---|---|---|
| Finger Flexion | WNL | WNL |
Right 90 Left 100 |
Assessment
Clinical Impression
Patient presents with subacute neck pain with mobility deficits. Patient presents with decreased active/passive range of motion and decreased strength in cervical musculature.
Patient with decreased flexibility and muscle length in muscles surrounding the shoulder in addition to changes in upper quarter posture. Patient with limited participation in sleeping, driving, bowling, playing cards, caring for grandchildren and flexion biased cervical motions.
Patient would benefit from skilled physical therapy in order to meet patient goals for reducing pain, improving active range of motion and functional activities.
Physical Therapy Plan of Care
Following the initial evaluation and examination, the physical therapist creates a plan of care with Luisa to assist her in managing her acute neck pain. This includes establishing goals, completing acute neck pain education, non-pharmacological strategies and a home exercise program.
Physical Therapy Goals
Short Term Goals: To be met in 3 weeks
- Patient will tolerate looking down up to 15 minutes in the cervical region.
- Patient resume normal sleeping patterns and social activities of playing cards, bowling and caring for grandchildren.
- Patient will complete driving without increased complaint of pain.
Long Term Goals: To be met in 6 weeks
- Patient will be able to resume mechanic activities for up to 4 hours without an increase in neck pain.
- Patient will be able to sleep 6-7 hours without awakening due to neck pain.
- Patient will return to bowling, playing cards, driving and caring for grandchildren without an increase in neck pain.
Physical Therapy Acute Neck Pain Education
- Acute pain usually comes on quickly and resolves in 6-8 weeks
- Posture and positioning for reading, sleeping, and activity modification to improve activity level/function and decrease discomfort
- Instruction in use of cold, heat and topical applications for pain reduction
- Review of TENS unit as a possible strategy
- Instruction in home exercise program and graded activity progression for pain reduction and improved upper quarter mobility and stability
Physical Therapy Neck Pain Clinical Practice Guideline
Based on Luisa’s presentation, the Neck Pain Clinical Practice Guideline (CPG) recommends the following:
Acute neck pain without radiculopathy or persistent headache summary:
- Most episodes of acute pain resolve within 8 weeks
- Some patients continue with ongoing symptoms or a recurrence of neck pain for more than a year
- Monitor for red flags: changes in bowel or bladder, numbness or tingling in the upper extremities
- Treatment Recommendations:
- Non-pharmacological strategies
- Pharmacological strategies
References
- Blanpied PR et al. Neck Pain: Revision 2017. Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability and Health From the Orthopaedic Section of the American Physical Therapy Association
- J Orthop Sports Phys Ther. 2017;47(7):A1-A83. doi:10.2519/jospt.2017.030
- Bier JD, Scholten-Peeters WGM, Staal JB, et al. Clinical practice guideline for physical therapy assessment and treatment in patients with nonspecific neck pain. Phys Ther. 2018;98:162–171.
Physical Therapy Non-Pharmacological Strategies
The physical therapist reviews non-pharmacological strategies for Luisa to try at home to help manage her acute neck pain.
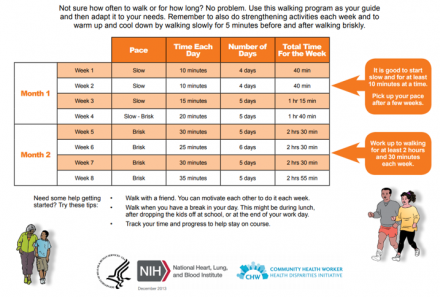
Home Exercise Program
The physical therapist reviews beginning a walking program for Luisa to try at home to help manage her acute neck pain.
- External Applications
- Topical pain relievers: mentholated or coolant gels
- Heat/Cold
- Activity
- Exercise
- Activity modifications
- Community of Faith
- Support
- Prayer
- Relaxation/Distraction
- Breathing
- Meditation
- Music
- Prayer
- Music
PT Interventions for Mrs. Sanchez
- Exercise
- Aerobic
- Stretching and Strengthening
- Use heat or cold
- Breathing
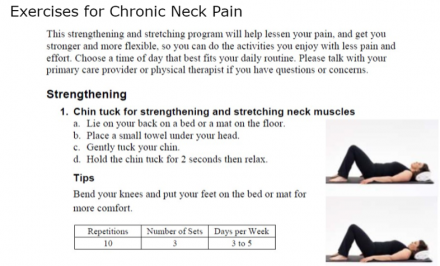
The physical therapist has Luisa begin an exercise program for stretching and strengthening of the neck and shoulders to help Luisa manage her acute neck pain.
Walking Program
Reference
Taylor D. Physical activity is medicine for older adults. Postgrad Med J. 2013;90(1059):26–32. doi:10.1136/postgradmedj-2012-131366
Exercises for Chronic Neck Pain
Efficacy of Physical Therapy Interventions
| Strategy | Strength | Evidence in Acute Neck Pain |
|---|---|---|
| Massage therapy | Weak | Short-term effect of massage therapy including massage and myofascial release in subacute and chronic neck pain |
| Aromatherapy | Inconclusive | Evidence in chronic neck pain in conjunction with other treatments but not acute neck pain |
| Physical therapy | Moderate | Moderate evidence for acute neck pain: may include manipulation or mobilization, exercise including endurance exercises, strengthening, range of motion and mobility, acute pain education |
| Topical applications | Moderate | Topical applications with menthol increases cutaneous blood flow; acts as a counter-irritant by sensitizing nociceptors and then desensitizing nociceptors |
| Exercise and activity | Strong | Strengthening, Flexibility and Aerobic Exercise have been shown to decrease acute pain. |
| Social support/Community of faith | Weak | Weak evidence for the role of social support/community of faith in acute pain |
| Relaxation | Weak | There is not specific evidence for relaxation in acute neck pain however there is evidence in procedural pain, labor pain, TMJ disorder, fibromyalgia |
| TENS | Weak | TENS has shown benefits in acute pain with acute neck pain showing inconclusive results |
| Music | Weak | |
| Reiki/Healing Touch | Moderate | Evidence in acute pain not specifically acute neck pain |
Interactive Activity PT Treatment with and without Medical Interpreter
Without Medical Interpreter
With Medical Interpreter
No Medical Interpreter VS Medical Interpreter
Without Medical Interpreter
- Caregiver was on the phone and distracted.
- Luisa was not engaged in the process.
- Therapist struggled to follow along; seemed to have difficulty knowing who to make eye contact with.
With Medical Interpreter
- Luisa was able to answer questions.
- Luisa and the physical therapist made eye contact, developed a rapport.
- Conversation was faster, easier to follow along.
Language Barriers
Without Medical Interpreter
- Luisa and caregiver had difficulty answering physical therapist’s questions.
- The physical therapist had to repeat herself with questions to help answer questions.
- Luisa and caregiver would talk at the same time.
- Conversation was awkward and many pauses.
With Medical Interpreter
- Luisa and the physical therapist made eye contact, developed a rapport.
- Luisa was able to tell her story.
- Luisa was able to describe her problem and goals.