Margaret is to be seen by the orofacial pain specialist.
Prior to the office visit, a medical history questionnaire is completed by the patient. The nurse practitioner reviews the patient’s answers to obtain other pertinent information that is best elicited using open-ended interviewing.
Nurse Practitioner Meets with Margaret and Her Mother
Nurse Practitioner Reviews Margaret's Answers to Pain Questionnaire
Nurse Practitioner Reviews Next Steps with Margaret and Her Mother
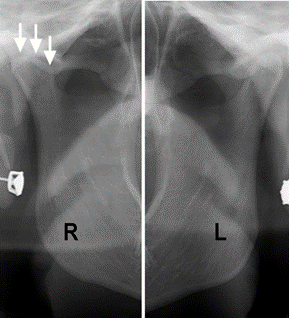
Based on the nurse practitioner’s evaluation, a panoramic x-ray is taken to evaluate the right and left condyles.
Panoramic Radiograph
17-year-old patient without temporomandibular joint involvement.

Yellow arrows indicate unerupted third molars (wisdom teeth)
Comparison of Left and Right Temporomandibular Joints
- A panoramic x-ray demonstrates that the right ascending ramus is shorter than the left
- There is flattening of the condyle on the right side (arrows)
- This suggests that the right condyle has osteoarthritic changes; the left condyle appears to be normal
Margaret Meets with Dr. Tallents
Margaret now sees Dr. Tallents, an orofacial pain specialist.
Review of the questionnaire and the interview with the nurse practitioner has documented:
- History of trauma, jaw and ear pain, joint noises, pain on jaw function and chewing, jaw locking, headache, and medications and other measures taken to alleviate the pain.
The clinical examination follows a template. The first part of the examination includes
measuring jaw mobility and evaluating symmetry.
Clinical Examination Template
Dr. Tallents Performs a Clinical Examination on Margaret
Findings include:
- Chin deviation to the right side and mandibular dental midline deviation of 4 mm to the right of the maxillary midline
- Vertical jaw opening 30 mm and right and left jaw movement is 8 mm and 3 mm, respectively
Examination now focuses on observation and palpation of the head and neck especially the muscles of mastication.
Findings include:
- Right sided jaw pain on manual palpation
- Pain in the right anterior and middle temporal muscle
- Crepitation sound on osculation in the right joint
- No evidence of tooth grinding because there is no wear on the maxillary and mandibular teeth
Dr. Tallents Palpates Areas of Margaret's Face for Sore Spots
Dr. Tallents’ advice at this time is to use conservative treatment (warm moist soaks, analgesics)
This treatment is often successful and the patient will not need any other intervention
Follow Up
The patient returns to the pain specialist one month later reporting minimal pain relief.
The recommendation now is to use a maxillary occlusal splint.


Dr. Tallents Meets With Margaret and Her Mother for a One Month Follow Up
- The benefit of using the maxillary occlusal splint is typically evaluated in 3-6 months
- In this case, the patient reports little improvement in headache/jaw joint pain
- Treatment options discussed at this time include surgery and alternative therapies such as acupuncture and chiropractic
Dr. Tallents Meets With Margaret and Her Mother for a Second Follow Up
Treatment Outcomes
- 80 % of patients will have improvement of pain using an occlusal splint
- 85 % of patients will have improvement of pain symptoms with surgical treatment

