A New Pain
Mary returns to her doctor eight weeks after completing her radiation.
Based on what you have already learned about pain assessment, what other questions do you have for Mary to help determine the contributors of her pain now?
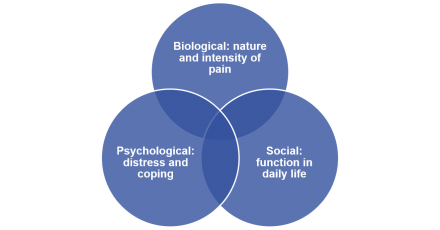
Biopsychosocial Syndrome
Cancer pain is a biopsychosocial syndrome. It is important to remember that pain has biological, social and psychological factors that all contribute to the overall experience of pain.
Following the Exam
Dr. Childers recommends seeing other members of the patient care team to help Mary cope with her pain.
Mary’s exam is consistent with myofascial pain and rotator cuff tendinitis. Her symptoms may have been exacerbated by testing and treatment, but not progression of cancer. One pitfall of managing pain in patients with cancer is the temptation to treat with opioids when new pain complaints arise. Many types of pain, such as those Mary is currently experiencing, are not optimally managed with opioids. Reassuring Mary that her pain is not related to her cancer is an important aspect of management. In addition, she should be encouraged to be active, and to avoid social isolation, an important contributor to morbidity in patients with non-cancer pain.
Follow-up: One Month
Mary presents one month later for a follow-up visit accompanied by her daughter. She has been going to physical therapy.
Patient Health Questionnaire (PHQ-4)
| Over the last 2 weeks, how often have you been bothered by the following problems? | Not at all | Several Days | More than half the days | Nearly every day |
|---|---|---|---|---|
| 1. Feeling nervous, anxious or on edge | 0 | 1 | 2 | 3 |
| 2. Not being able to stop or control worrying | 0 | 1 | 2 | 3 |
| 3. Little interest or pleasure in doing things | 0 | 1 | 2 | 3 |
| 4. Feeling down, depressed, or hopeless | 0 | 1 | 2 |
3 |
The Patient Health Questionnaire for Depression and Anxiety, or PHQ4, is one validated instrument to assess for distress in medical settings. This brief tool screens specifically for depression and anxiety. It is comprised of the Generalized Anxiety Disorder Scale, or GAD-2, a two-item screen for anxiety, and the PHQ2, a two-item screen for depression. GAD-2 items are represented by questions 1 and 2 shown here, and PHQ2 items by questions 3 and 4. A positive screen should prompt the clinician to take a more detailed history to determine whether treatment of depression or anxiety is indicated.
Reference
Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics 2009 Dec 31;50(6):613-621.
Mood Disorders
Nearly half of cancer patients have mood disorders.
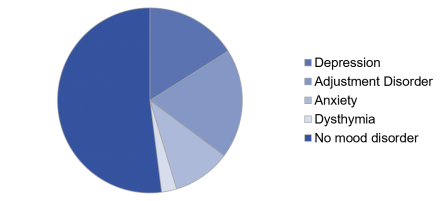
Mood disorders occur commonly in patients with cancer. Patients may perceive their depression or anxiety as a “natural” reaction to having cancer. In such cases, it is important for the clinician to educate the patient about the importance of treating these conditions, because it left untreated, they can negatively impact pain treatment outcomes, as well as overall cancer survival.
Thought Starter
What additional information is important for developing a pain management plan for Mary?
Not All Cancer Pain Should be Treated with Opioids
Because not all pain in a cancer patient is cancer pain, not all pain should be treated with opioids.
Not all pain in a cancer patient is related to the cancer or its treatment. As with Mary, myofascial pain within the shoulder was the underlying physical contributor to her pain symptoms. At the same time, a person’s psychological well-being can influence one’s pain experience particularly anxiety and depression. As a result, co-morbid psychological conditions require management to optimize pain related outcomes whether or not the pain itself is the result of cancer or a non-cancer condition.
Given the many dimensions of one’s pain experience, it is important to remember that not all pain in a cancer patient should be treated with an opioid. In fact, most etiologies of non-cancer pain respond better to other management strategies and should be integrated into the care plan prior to consideration of an opioid.
Medication Options
Mary’s doctor discusses options for antidepressant therapy and they decide together to start duloxetine.
Community support services and referral to psychosocial oncology are discussed and Mary agrees to see psychosocial oncology.
Total Pain
Total pain contributes to suffering.
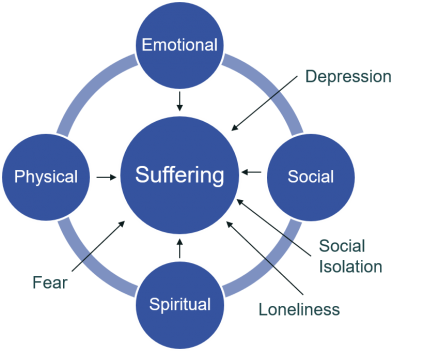
Total pain more accurately depicts the complex experience of suffering in patients with serious illness including cancer. Total pain expands on the biopsychosocial model to include additional dimensions of suffering.
Patients with serious illness often express distress in multiple areas, and each of these contributes to the overall pain experience.
Social
Social aspects of suffering often include the impact an illness has on a patient’s role in the family. The patient may be concerned about contributing to family stress both emotional and financial. They also may fear being a burden. Financial concerns can also arise with loss of income—for both the patient and the persons helping to care for the patient—along with the cost of the cancer treatment itself. Often the patient’s changed role in the family negatively affects their sense of identity.
The social aspects of suffering include:
- Effect of illness on family
- Worry about family stress
- Being a burden
- Loss of role
- Changes in identity
- Financial concerns
- Loss of income
- Costs of treatments
Spiritual
Spiritual aspects of suffering typically arise because of the existential threat that serious illness brings. This crisis of meaning is often expressed in questions about why the illness is happening. It is important to recognize these questions as having deeper meaning beyond the patient wanting concrete medical facts. Spiritual assistance may be a key part of helping patients cope. They may express anger at God, and may have stopped participating in their faith community at a time when it is most needed.
The spiritual aspects of suffering include:
- Asking, "Why me?"
- Anger at God
- Loss of meaning
- Loss of involvement in previous spiritual community
Psychological
Psychological distress as previously mentioned, may be caused by fear, adjustment disorders, as well as anxiety and depression. It can also manifest in substance use disorders and chemical coping. Patients may use analgesics and sedative medications in order to escape their distress rather than actively cope with it.
The psychological aspects of suffering include:
- Anxiety
- Depression
- Post-traumatic stress disorder
- Substance use disorders
Physical
Patients with cancer may have pain of different types, some related to their cancer or its treatment, and some not. Patients may also have pain from several of these sources at once.
The physical aspects of suffering include:
- Pain directly caused by cancer
- Pain caused by cancer treatment
- Chemotherapy induced peripheral neuropathy
- Post-surgical pain
- Chronic nonmalignant pain
Treatment Beyond Medications
- Individual and family therapy
- Financial and legal advisors
- Dignity therapy
- Bodywork (massage, yoga, etc.)
- Acupuncture
- Mindfulness training
- Spiritual care
Many of the contributors to total pain require specific expertise beyond that of a medical provider. This reminds us of the importance of an interdisciplinary team in the management of pain in a patient with serious illness, in this case pain in a patient with metastatic cancer. A subspecialty of psychiatry and psychology called psycho oncology is often engaged to work with cancer patients and their families. The existence of this subspecialty underscores the role that psychological issues play in cancer patients. Treatment approaches can include medications such as the duloxetine that Mary has been prescribed as well as talk therapy in private and group settings, couples and family therapy, cognitive behavioral therapy, and mindfulness based stress reduction.
Spiritual care is typically supported through hospital chaplaincy or pastoral care programs, and may include a specifically designed treatment for persons with serious illness called dignity therapy. There is a significant body of literature supporting the integration of psychological and spiritual care services into comprehensive cancer care. Integrative therapies such as yoga, acupuncture and massage are gaining popularity but the evidence base, while growing, is not definitive.
Follow-up: Three Months
Case Conclusion
Pain in a Patient with Metastatic Cancer
Wrap-up.

