Differential Diagnosis for Oral and Facial Pain
Consider the following typical conditions that can cause oral and facial pain as you develop your differential diagnosis.
- Dental issues
- Temporomandibular disorders (TMD)
- Cutaneous and Mucogingival Pains
- Neuropathic pain
- Neurovascular pain (Headache)
- Intracranial, Head, Neck and Oral neoplasm
- Vascular Pains
- Visceral Pains
- Infection
- Other conditions: Lyme Disease, Eagle syndrome, Post-stroke pain, etc.
This is not an all inclusive list. The entire list of conditions causing oral and facial pain exceeds the scope of this training module
A thorough understanding of sources of oral and facial is paramount, and the clinician should be very cautious not to dismiss the pain as psychological in nature.
Dental Causes
Consider the following typical conditions that can cause oral and facial pain as you develop your differential diagnosis.
- Odontogenic Sources of Pain
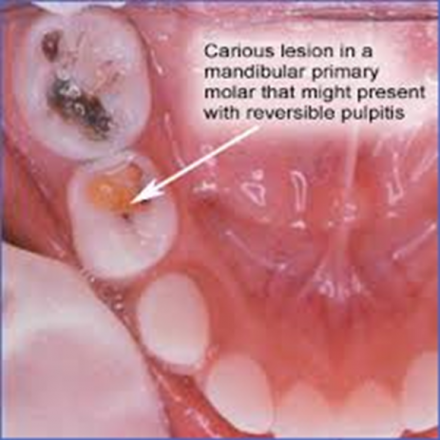
- Pulpal
- Pulpitis, Dentin hypersensitivity, Cracked tooth syndrome
- Features: Pain is localized; pain can be aggravated by mechanical or chemical irritants (heat, cold, acids, palpation and percussion); Site and source of pain are the same
- Periodontal
*image: https://en.wikipedia.org/wiki/Pericoronitis#/media/File:48_clinical_per…
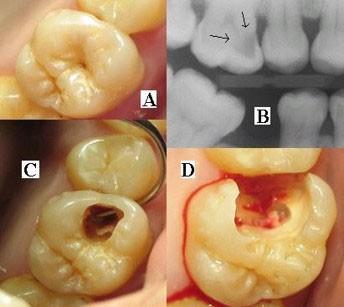
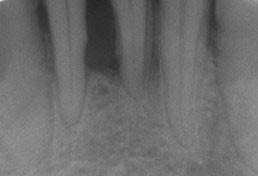
Periapical periodontitis and periapical abscess
Features: Pain is localized; pain can be aggavated by percussion; site and source of pain are the same. May be present with oral or facial swelling. Verified by dental exam and dental x-ray.
- Pericoronitis and pericoronal abscess
* image: https://upload.wikimedia.org/wikipedia/commons/d/d2/ToothMontage3.jpg
Features: Visible tissue inflammation near erupting 3rd molars. Pain is localized; pain can be aggravated by palpation; site and source of pain are the same.
*image: https://upload.wikimedia.org/wikipedia/commons/4/48/Paro1.JPG
Temporomandibular Oral and Facial Pain
Temporomandibular disorder (TMD)
Consists of muscular pain, TM joint pain, or both
Second most common source of orofacila pain
Features: must be aggravated by jaw function, functional testing, or palpation of associated structures. May require diagnostic imaging and/or bloodwork.
Cutanous and Mucogingival Pain
Oral ulceration (e.g. aphthous stomatitis, erosive oral lichen planus, etc.)
Features: Pain is localized; visible oral tissue changes or trauma are present

*image: https://en.wikipedia.org/wiki/Aphthous_stomatitis#/media/File:Aphtha2.jpg
Neuropathic Oral/Facial Pain
Episodic/paroxysmal
Features: brief lancinating pain lasting a few seconds. Touching an oral or facial trigger zone may precipitate attacks.
Consider
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Nervus intermedius neuralgia
Continuous
Features: continuous pain. Most often burning quality.
Consider
- Burning mouth syndrome
- Persistent idiopathic facial pain (old terminology atypical facial pain, persistent dentoalveolar pain)
- Complex regional pain syndrome
- Post-herpetic neuralgia
- Post traumatic trigeminal pain
- Anesthesia Dolorosa
Neurovascular Oral and Facial Pain
Neurovascular pain is traditionally thought of as headaches (HA) and the terminology reflects that. But neurovascular pain can also present in the facial region.
- Migraine
- Features: Unilateral severe pain. Nausea and/or vomiting. Photophobia, phonophobia and/or osmophobia. Alleviated by sleep. May present in head, maxilla, mandible, tooth.
- Tension-type Headache
- Features: Bilateral mild to moderate pain. Pressing/tightening quality. No nausea, no vomiting.
- Cluster headache and other Trigeminal Autonomic Cephalgias
- Features: Severe pain with autonomic features
- Other primary headaches (includes hemicrania continua, new daily-persistent HA, primary stabbing headache, primary cough HA, primary exertional HA, etc.)
Intracranial, Head, Neck and Oral Neoplasm
Time is a critical factor in diagnosis

*image: https://en.wikipedia.org/wiki/Oral_cancer#/media/File:ZungenCa2a.jpg
Vascular Oral and Facial Pain
Vascular Pain
- Ischemic cerebrovascular disease
- Intracranial hemorrhage
- Vascular malformation
- Temporal Arteritis
Features
- Unilateral or bilateral pain in temporal region; throbbing, burning or lancinating quality; medical emergency due to rapid loss of vision; requires ESR blood study; confirmed by biopsy. Systemic symptoms and/or neurological deficits associated with jaw claudication; sometimes allodynia of scalp
- Carotydinia
Additional Possibilities
- Visceral Oral/Facial Pains
- Glandular pain
- Ocular pain
- Auricular pain
- Sinusitis
- Infection
- Cardinal signs and symptoms of infection (dolor, rubor, etc.) and/or radiographic features (dental abscess, intrabony lesion, etc.)
- Other*
- Lyme disease
- Eagle syndrome (Features: Very rare. Usually unilateral, neuralgic pain. Elongation/calcification of stylohyoid ligament visible on radiograph)
- Post-stroke pain
*This is not an all-inclusive list. The entire list of conditions causing oral and facial pain exceeds the scope of this training module
Summary
There are many reasons for oral and facial pain, but a thorough assessment and examination of a patient should result in a limited list of differential diagnoses as demonstrated in this visit. Treatment of pain should address both the mechanisms of pain and the underlying pathology that prompted the patient’s pain.
Assessment and examination of patients with oral and facial pain will be demonstrated in the neurophysiology visit of this module. Treatments will be explained in both the neurophysiology and genetic visits.
A comprehensive understanding of sources of oral and facial is paramount, and the clinician must avoid dismissing the pain as psychological in nature. During the remainder of this visit, you will learn about the development of pain theories and the basis for our current understanding of pain.

