11-point Numerical Rating Scale (NRS)
There are several different scales that can be used to assess for pain severity.
The most common is the 11-point Numerical Rating Scale (NRS), which uses the range 0-10. The benefits of the NRS are its simplicity and validity. Possible drawbacks include response variability and moderate correlation with functional status.

Opioid Risk Tool
Link opens a PDF version of the Opioid Risk Tool.
Numeric Risk Tool
Link opens a PDF version of the Numeric Risk Tool.
Quick DASH
Link opens a PDF version of the QuickDASH.
Functional Pain Scale (FPS)
Instructions:
Ask the patient if pain is present. If the patient has pain, ask him or her to rate the pain subjectively as either "tolerable" or "intolerable."
Finally, find out if the pain interferes with function.If the patient rates the pain as "tolerable," establish whether the pain interferes with any activity. If the pain is "intolerable," determine whether the pain is so intense as to prevent passive activities. See the chart below for guidelines.
- 0 No pain
- 1 Tolerable (and does not prevent any activities
- 2 Tolerable (but does prevent some activities
- 3 Intolerable (but can use telephone, watch TV, or read)
- 4 Intolerable (but cannot use telephone, watch TV, or read)
- 5 Intolerable (and unable to verbally communicate because of pain)
Scoring:
The patient's subjective rating of pain and the objective determination of the pain's interference with activities will produce a corresponding score on a scale of 0-5.
A lower score equates to less severe pain and less interference with functional abilities, if any. Ideally, all patients should reach a 0 to 2 level, preferably 0 to 1.
It should be made clear to the respondent that limitations in function only apply if limitations are due to the pain being evaluated.
Source:
Gloth FM III, Scheve AA, Stober CV, Chow S, Prosser J. The Functional Pain Scale: reliability, validity, and responsiveness in an elderly population. J Am Med Dir Assoc. 2001;2(3):110-114.
OPQRST
When assessing pain, it is important to ask certain questions in order to get a full understanding of the patient’s pain history. There are different methods you can use to remember the important questions to ask. One option is the pneumonic “OPQRST.”
O – Onset: When did the pain start? What was happening at that time?
P – Palliative and Provocative factors: What makes the pain better? Worse? (Include specific activities, positions or treatments.)
Q – Quality: Describe the pain. Is it burning, sharp, shooting, aching, throbbing, etc.?
R – Region and Radiation: Where is the pain? Does it spread to other areas?
S – Severity: How bad is the pain? (There are several scales to use, which will be discussed in the following slide)
T – Timing: When does the pain occur? Has it changed since onset? If so, how?
Reference:
Powell RA, Downing J, Ddungu H, Mwangi-Powell FN. Pain Management and Assessment. In: Andrea Kopf NBP, editor. Guide to Pain Management in Low-Resource Settings. Seattle: IASP: International Association for the Study of Pain; 2010. p. 67-79 http://www.iasp-pain.org/AM/Template.cfm?Section=Home&TEMPLATE=/CM/HTML….
Screening
Ask, "Are you experiencing any discomfort right now?"
If No: document “zero” pain and reassess periodically
If Yes: ask about its nature (verbal description) pattern (over time) and location
Try to quantify the intensity of the pain, show the patient the rating tools we use and determine which one is easiest and most meaningful for them.
Try to quantify the intensity of the pain, show the patient the rating tools we use and determine which one is easiest andmost meaningful for them.
Starting with the Numeric Risk Tool (remember, this is an eleven point scale of 0-10, not 1-10), ask the patient if they would recognize:
- if the discomfort were completely gone ("a rating of 0")
- or the worst they or anybody else could possibly experience ("10")
Have the patient rate the intensity of their pain/discomfort "right now" verbally with a number of by pointing to the number that represents their pain intensity.
Once the patient understands this scale, follow-up questions may be tried without the visual aid:
- "On a scale of 0 to 10, how much pain (or discomfort) are you experiencing now?"
If the Numeric Risk Tool is not easy and meaningful, use the Verbal Descriptor Scale:
- Determine if discomfort is "none" (chart 0) or the worst possible (chart 10).
- Ask if the discomfort or pain is mild, moderate, severe, or extreme.
-
- Record 2 (for mild), 4 (for moderate), 6 (for severe), or 8 (for extreme) accordingly.
- If the patient reports it's between two words, select the odd number between them (e.g. the score of a report of pain between mild and moderate = 3)
If that isn't easy and meaningful, use the Functional Pain Scale.
Determine if it is tolerable ("less than or equal to 5") or intolerable ("greater than or equal to 5").
- Tolerable pain that does not interfere with activities = 2
- Tolerable pain that interferes with physically demanding activities = 4
- Intolerable pain that interferes with physically demanding activities = 5
- Intolerable pain that interferes with active but not passive activities = 6
- Intolerable pain that interferes with passive acitivities (e.g. reading) = 8
- Pain so severe the patient can't do any active or passive activities (e.g. can't even talk about pain without writhing/screaming) = 10
Reassess using the 4-A's determining safety and efficacy of therapy:
- Analgesia: To what extent did the treatment reduce the pain and make it more tolerable? This can be evaluated using one of the pain intensity scales above, the percent that pain intensity is reduced by (e.g., 30%, 50%, etc.) or adjectives (good, excellent effect) the patient uses.
- Activity: To what extent did the patient's activity and rest patterns improve as a result of the treatment? Does pain interfere less with usual and prescribed therapeutic (e.g. physical therapy) activity? Does pain interfere less with sleep? Does the treatment affect safety?
- Adverse effects: What side effects, toxicity, technology-related complications are experienced?
- Aberrant behaviors: Has the medication affected medication-focuxed behaviors or personality?
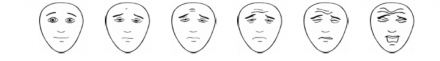
The Faces Pain Scale can also be used for any patient, but is especially useful with children or non-verbal patients. This is a well-studied and validated scale.
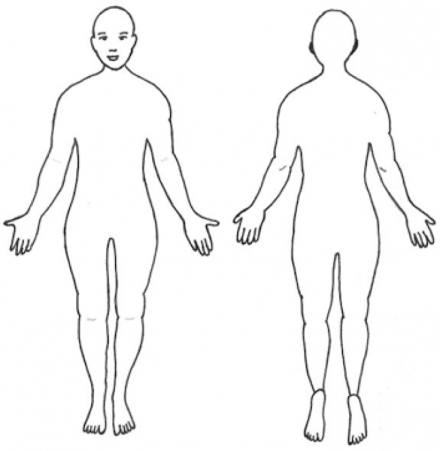
A body diagram can allow patients to pinpoint their pain site(s) to help guide your examination.
Additionally, observing patients when they move or during the exam is a useful addition to these scales, and is essential with young children and non-verbal adults.
Physical manifestations associated with acute pain, opioid withdrawal and opioid overmedication should be distinguished.
The table below matches the signs and symptoms to their corresponding condition(s) so you can see the similarities and differences for each condition.
| Signs/Symptoms | Acute Pain | Opioid Withdrawal | Opioid Overmedication |
|---|---|---|---|
| Tachycardia (fast heart rate) | Yes | Yes | No |
| Hypertension (high blood pressure) | Yes | Yes | No |
| Disphoresis (sweating) | Yes | Yes | No |
| Vasoconstriction (cold hands/feet) | Yes | Yes | No |
| Mydriasis (dilated pupils) | Yes | Yes | No |
| Tremors (shaking) | No | Yes | No |
| Dysphoria/anxiety (emotional state characterized by depression, anxiety, unease) | No | Yes | No |
| Flu-like symptoms (runny nose, congestion, malaise, etc.) | No | Yes | No |
| Depression (low mood) | No | Yes | No |
| Diarrhea/vomiting | No | Yes | No |
| Respiratory Depression (low respiratory rate) | No | No | Yes |
| Bradycardia (low heart rate) | No | No | Yes |
| Miosis (constricted pupils) | No | No | Yes |
| Vasodilation (warm extremities) | No | No | Yes |
| Myclonic jerks (sudden muscle contractions/twitches) | No | No | Yes |

