History of Present Illness

Mr. Monahan is a retired, community-dwelling, 81 year old Caucasian male who was a carpet installer for 50 years. He has a history of lower back pain, morbid obesity, hypertension, hypothyroid, occipital lobe stroke, bilateral knee arthroplasty, GERD and sleep apnea. You are seeing Mr. Monahan in his home, as a part of your pre-licensure course Interprofessional Care of the Community-Dwelling Older Adult. The team consists of a second-year Medical Student and a senior Nursing Student. Your assignment is to perform general health and tailored pain assessment, and develop for Mr. Monahan a home-based management plan of care.
Pain Assessment
What else would you like to know from Mr. Monahan?
- Health history
- Pain assessment
- Physical exam
- Review of diagnostic tests
- Usual daily activities
- Goals for pain treatment
Chief Complaint
“My back is killing me. You’ve got to do something.”
Past Medical History
- Hypertension
- Hypothyroidism
- GERD
- OSA
- Occipital lobe cerebral vascular accident
Past Surgical History
- Vasectomy
- Bilat total knee arthroplasty
Current Medications
- Tramadol 50 – 100 mg p.o. Q 12 hrs prn back pain
- Atenolol 25 mg p.o. Q a.m.
- Levothyroxine sodium 125 mcg p.o. Q a.m.
- Clopidogrel 75 mg p.o. Q a.m.
- Ibuprofen 600 mg ii p.o. prn knee pain
- Aspirin 650 mg p.o. prn “when I can’t get to sleep”
- Multi-Vitamin
Family History
Parents divorced in 1946. His father had a heart valve replacement in 1978 and died at 92. His mother died of pancreatic cancer at age 85. He has two sisters who are in good health.
Social History
Mr. Monahan has been married for 62 years. He and his wife live in the farm in which they raised their family. He has 5 children, 8 grandchildren, and 6 great grand children. His parents are deceased. He has a high school education. He was self-employed as a carpet installer and retired in 2009. Mr. Monahan’s friends are all deceased. Reports does not engage in much social activity “because my back hurts.” Will push through the pain when his children are home to visit.
Psychiatric History
Denies psychiatric history.
Substance Abuse History
Denies ETOH or recreational drug use. Does not smoke.
Review of Systems
CardioPul
Has HTN, denies palpitations, chest pain, shortness of breath, or cough. Has OSA and has CPAP unit that he uses intermittently. Reports numerous night time awakenings and difficulty getting back to sleep. Reports takes ASA ii p.o. hs prn for sleep. Feels tired during the day.
GI/GU
Reports constipation when takes tramadol. Takes 2-3 extra strength laxative tablets for this and then has diarrhea for 1-2 days. Denies blood in stool, steatorrhea, bloating. Had had testing for occult blood in the past year that was negative. Reports urinary frequency and urgency, and wears disposable, absorbent underwear when he travels. Has GERD; reports burning sensation in throat and bad taste in his mouth.
Neuro
Reports memory problems, “I just can’t remember things like I used to.” Does not get lost when driving with his wife.
HEENT
Wears glasses that have bifocal lenses “so I can read the paper,” reports decreased hearing acuity and does not wear hearing aids; denies tinnitus or ear pain. Reports summer allergies and sinus drainage; denies sore throat, difficulty chewing or swallowing. Denies changes in voice, hoarseness.
Allergies
NKA
Pain Measurement
What are some important questions to ask Mr. Monahan about his pain?
The pain alphabet will guide the questions you ask Mr. Monahan:
Q: Quality – Aching, burning, sharp, deep, freezing, dull, squeezing/pressure, stabbing
R: Region – Where is your pain?
S: Severity – 0(no pain) – 10(worst pain), pain severity?
T: Timing – Is the pain constant? Intermittent?
U: Usually associated with – Activities/symptoms that cause/co-occur with pain?
V: Very much relieved by – What do you do to help reduce your pain?
W: Worse with – What makes your pain worse (poor sleep, activity, etc.)
Mr. Monahan's Pain Assessment
Q: Quality
States “My back hurts every day. Sometimes my back pain is sharp and stabbing, other days it’s a dull and throbbing ache. I don’t know why it changes. My knees ache. It hurts to stand.”
R: Region
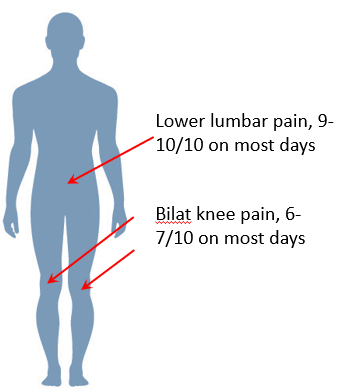
Mr. Monahan is able to point to knees and back as areas that are painful.
S: Severity
He is able to provide to you pain scores for each painful body site.
T: Timing
States “My knees ache all the time and the pain is worse first thing in the morning. I never know when my back will hurt. Some days I can plenty, other days I can only sit in my chair.”
U: Usually Associated With
“I get bound up by the Tramadol. When my back is bad, I can’t sleep.”
V: Very Much Relived By
“My doctor gave me these [shows bottle of tramadol], some days I’ll take just 1 pill, other days I take 2. I don’t take it every day. I take Motrin 2 or 3 pills, for my knees. I don’t know what else to do. Sometimes a heating pad helps.”
W: Worse With
“When I stand still for a long time, my back hurts. I can’t go shopping with Joan, because I can’t stand still. I have to mow my lawn over 2 days. The jarring on the lawn tractor really makes my back hurt a lot. I try to ride my exercise bike. Some days I can go 5 minutes.”