You would like to address Mrs. Farley's pain using a multi-modal and inter-professional approach with the help of health care providers from different fields.
You discuss her possible diagnoses and treatment options with her.
Temporomandibular Disorder (TMD) Pathophysiology, Diagnosis, and Management
First, let's start by reviewing some terms.
Myofascial Pain
Dull aching regional pain referred from or emanating around active muscle trigger points
Arthralgia
Pain felt in a joint.
Trigeminal Neuralgia
Disorder of the sensory divisions of cranial nerve V, characterized by recurrent paroxysms of sharp, stabbing pains in the distribution of one or more branches of the nerve, often precipitated by stimulation of specific trigger points.
Tension-type Headache
Dull, aching, pressing, usually bilateral headache of mild to moderate intensity.
Migraine
Periodic, recurrent, intense throbbing headache, frequently unilateral that can be accompanied by phonophobia, photophobia, and nausea and vomiting.
Chronic Pain
Pain that persists when other aspects of disorder or disease have resolved, and typically lasts more than 3-6 months or beyond the normal time for healing of an acute injury or pain.
Nociceptive Pain
Pain from tissue damage and the subsequent release of chemicals.
Neuralgia
Paroxysmal or constant pain, typically with sharp, stabbing, itching, or burning characteristics, in the distribution of a specific nerve or nerves.
Neuropathic Pain
Pain caused by a dysfunction in the peripheral or central nervous system.
Acute Pain
Unpleasant sensation with a duration limited to the normal healing time or the time necessary for neutralization of the initiating or causal factors.
TMD Epidemiology & Diagnosis
What is TMD?
A collection of musculoskeletal disorders of the head and neck involving the muscles of mastication and jaw joints. Included are headaches, neck and ear pain influenced by jaw function.
Reference
- Stegenga B. Nomenclature and classification of temporomandibular joint disorders. J Oral Rehabil. 2010 Oct;37(10):760-5. doi:10.1111/j.1365-2842.2010.02146.x. PubMed PMID: 20887277.
- Wacyl Mesnay (2012). Current role of orthodontists in treating temporomandibular disorders. Journal of Dentofacial Anomalies and Orthodontics, 15, 205 doi:10.1051/odfen/2012105 Link to this article: http://www.jdaojournal.org/10.1051/odfen/2012105
- Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008 Dec 18;359(25):2693-705. doi: 10.1056/NEJMra0802472. Review. PubMed PMID 19092154.
- Vázquez-Delgado E, Cascos-Romero J, Gay-Escoda C. Myofascial pain associated to trigger points: a literature review. Part 2: differential diagnosis and treatment. Med Oral Patol Oral Cir Bucal. 2010 Jul 1;15(4):e639-43. Review. PubMed PMID: 20173729.
Whom Does TMD Affect?
Epidemiologic studies have shown that 40-70% of the population exhibit signs and symptoms of TMD, while 30-45% of the population experience jaw joint sounds. Approximately 7% of these persons will have symptoms severe enough to require treatment. The most common TMD patients are women of childbearing age, although a recent study found chronic TMD in older women with TMJ osteoarthritis.
Reference
Slade GD, Bair E, By K, Mulkey F, Baraian C, Rothwell R, Reynolds M, Miller V, Gonzalez Y, Gordon S, Ribeiro-Dasilva M, Lim PF, Greenspan JD, Dubner R, Fillingim RB, Diatchenko L, Maixner W, Dampier D, Knott C, Ohrbach R. Study methods, recruitment, sociodemographic findings, and demographic representativeness in the OPPERA study. J Pain. 2011 Nov;12(11 Suppl):T12-26.
doi: 10.1016/j.jpain.2011.08.001. PubMed PMID: 22074749; PubMed Central PMCID: PMC3666856.
Questions to Ask to Determine if Your Patient has TMD
- Do you have pain in or around the ears, temples, or cheeks?
- Do you have frequent headaches and/or neck aches?
- Have you had a recent injury to your head, neck, or jaw?
- Have you previously been treated for a TMD problem?
- Do your jaws regularly feel stiff, tight, or tired?
- Do you have difficulty or pain when opening your jaw?
- Does your jaw get stuck or locked?
- Do you have difficulty or pain when chewing, talking, or using your jaws?
- Are you aware of noises in your jaw joints?
- Have you ever been treated for a jaw pain problem?
Ask the patient these questions to assess their pain and/or limited range of motion (ROM) with jaw function. If the patient is pain-free and does not have limited ROM, consider other orofacial pain disorders such as neuralgia, tooth pain, headache, etc.
Etiology of TMD
Why do some people with signs and symptoms of TMD have pain and limited jaw opening while others do not? As with any pain patient, the answer is multifactorial and can include (but is not limited to) TMJ disc displacement, parafunctional habits, uncomfortable occlusion (bite), peripheral and/or central sensitization.
Reference
- Lim PF, Maixner W, Khan AA. Temporomandibular disorder and comorbid pain conditions. J Am Dent Assoc. 2011 Dec;142(12):1365-7. PubMed PMID: 22130437.
- Fricton JR. Clinical care for myofascial pain. Dent Clin North Am. 1991 Jan;35(1):1-28. Review. PubMed PMID: 1997346.
- Cairns BE. Pathophysiology of TMD pain--basic mechanisms and their implications for pharmacotherapy. J Oral Rehabil. 2010 May;37(6):391-410. doi:10.1111/j.1365-2842.2010.02074.x. Epub 2010 Mar 10. Review. PubMed PMID:20337865.
Distinguishing TMJ from a Masticatory Muscle Problem
Ask the patient to point to the location of their pain. Then, duplicate their pain with palpation. If preauricular pain occurs with vertical and lateral ROM, the source of pain is likely coming from the TMJ. TMJ arthralgia is usually sharp during jaw movement. Muscle pain is usually dull, aching, can be constant, and with somewhat limited ROM.

Reference
- Stegenga B. Nomenclature and classification of temporomandibular joint disorders. J Oral Rehabil. 2010 Oct;37(10):760-5. doi: 10.1111/j.1365-2842.2010.02146.x. PubMed PMID: 20887277.
- Fricton JR. Clinical care for myofascial pain. Dent Clin North Am. 1991 Jan;35(1):1-28. Review. PubMed PMID: 1997346.
- Manolopoulos L, Vlastarakos PV, Georgiou L, Giotakis I, Loizos A, Nikolopoulos TP. Myofascial pain syndromes in the maxillofacial area: a common but underdiagnosed cause of head and neck pain. Int J Oral Maxillofac Surg. 2008 Nov;37(11):975-84. doi: 10.1016/j.ijom.2008.04.023. Epub 2008 Jul 15. Review. PubMed PMID: 18632254.
TMD Pathophysiology
Peripheral Mechanism: What causes TMJ Disc Displacement?
Adhesions in the joint capsule affect disc mobility, which cause the ligaments holding the disc in place to become stretched.
Reference
Vos LM, Slater JJ, Leijsma MK, Stegenga B. Does hypoxia-reperfusion injury occur in osteoarthritis of the temporomandibular joint? J Orofac Pain. 2012 ;26(3):233-9. Review. PubMed PMID: 22838008
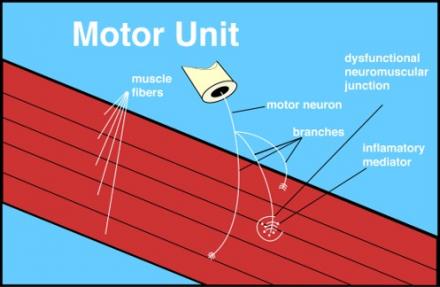
Pathophysiology of Myofascial Trigger Points
Myofascial trigger points are thought to be caused by a dysfunctional neuromuscular junction.
Reference
- Shah JP, Phillips TM, Danoff JV, Gerber LH. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J Appl Physiol. 2005 Nov;99(5):1977-84. Epub 2005 Jul 21. PubMed PMID: 16037403.
- Mense S. Nociception from skeletal muscle in relation to clinical muscle pain. Pain. 1993 Sep;54(3):241-89. Review. PubMed PMID: 8233542.
- Carlson CR, Okeson JP, Falace DA, Nitz AJ, Curran SL, Anderson D. Comparison of psychologic and physiologic functioning between patients with masticatory muscle pain and matched controls. J Orofac Pain. 1993 Winter;7(1):15-22. PubMed PMID: 8467294.
- Vázquez-Delgado E, Cascos-Romero J, Gay-Escoda C. Myofascial pain syndrome associated with trigger points: a literature review. (I): Epidemiology, clinical treatment and etiopathogeny. Med Oral Patol Oral Cir Bucal. 2009 Oct1;14(10):e494-8. Review. PubMed PMID: 19680218.
Do Pain Processing Problems Cause TMD?
TMD patients can have increased temporal summation and lower pain thresholds. Abnormal reactions to stress have been found in TMD patients.
Reference
- Zubieta JK, Heitag MM, Smith YR, et al. COMT val168met genotype affects mu-opioid neurotransmitter responses to a stressor. Science 2009;299:1240–3. Not on Pub Med?
- Martenson ME, Cetas JS, Heinricher MM. A possible neural basis for stress-induced hyperalgesia. Pain. 2009 Apr;142(3):236-44. doi: 10.1016/j.pain.2009.01.011. Epub 2009 Feb 15. PubMed PMID: 19232470; PubMed Central PMCID: PMC2676435.
- Maixner W, Fillingim R, Booker D, Sigurdsson A. Sensitivity of patients with painful temporomandibular disorders to experimentally evoked pain. Pain. 1995 Dec;63(3):341-51. PubMed PMID: 8719535.
- Diatchenko L, Slade GD, Nackley AG, Bhalang K, Sigurdsson A, Belfer I, Goldman D, Xu K, Shabalina SA, Shagin D, Max MB, Makarov SS, Maixner W. Genetic basis for individual variations in pain perception and the development of a chronic pain condition. Hum Mol Genet. 2005 Jan 1;14(1):135-43. Epub 2004 Nov 10. PubMed PMID: 15537663.
- Diatchenko L, Anderson AD, Slade GD, Fillingim RB, Shabalina SA, Higgins TJ, Sama S, Belfer I, Goldman D, Max MB, Weir BS, Maixner W. Three major haplotypes of the beta2 adrenergic receptor define psychological profile, blood pressure, and the risk for development of a common musculoskeletal pain disorder. Am J Med Genet B Neuropsychiatr Genet. 2006 Jul 5;141B(5):449-62. PubMed PMID: 16741943; PubMed Central PMCID: PMC2570772.
- Garrett PH, Sarlani E, Grace EG, Greenspan JD. Chronic temporomandibulardisorders are not necessarily associated with a compromised endogenous analgesic system. J Orofac Pain. 2013 Spring;27(2):142-50. doi: 10.11607/jop.943. PubMed
- PMID: 23630686.
- Sarlani E, Grace EG, Reynolds MA, Greenspan JD. Evidence for up-regulated central nociceptive processing in patients with masticatory myofascial pain. J Orofac Pain. 2004 Winter;18(1):41-55. PubMed PMID: 15029872.
Central Mechanism: Do Genetics Play a Role in TMD?
Genetic studies indicate that the genetic contribution to the development of TMD is a small part of the overall risk for these disorders; however, gender is the single biggest risk factor for TMD. Gender differences in pain thresholds, temporal summation, pain expectations, and somatic awareness can exist with chronic TMD.
Reference
- Oakley M, Vieira AR. The many faces of the genetics contribution to temporomandibular joint disorder. Orthod Craniofac Res. 2008 Aug;11(3):125-35. doi: 10.1111/j.1601-6343.2008.00426.x. Review. PubMed PMID: 18713149.
- Palmer SN, Giesecke NM, Body SC, Shernan SK, Fox AA, Collard CD. Pharmacogenetics of anesthetic and analgesic agents. Anesthesiology. 2005 Mar;102(3):663-71. Review. PubMed PMID: 15731608.
- Meloto CB, Serrano PO, Ribeiro-DaSilva MC, Rizzatti-Barbosa CM. Genomics and the new perspectives for temporomandibular disorders. Arch Oral Biol. 2011 Nov;56(11):1181-91. doi: 10.1016/j.archoralbio.2011.03.012. Epub 2011 May 4. Review. PubMed PMID: 21536254.
- Shaefer JR, Holland N, Whelan JS, Velly AM. Pain and temporomandibular disorders: a pharmaco-gender dilemma. Dent Clin North Am. 2013 Apr;57(2):233-62. doi: 10.1016/j.cden.2013.02.005. PubMed PMID: 23570804.
- LeResche L, Sherman JJ, Huggins K, Saunders K, Mancl LA, Lentz G, Dworkin SF. Musculoskeletal orofacial pain and other signs and symptoms of temporomandibular disorders during pregnancy: a prospective study. J Orofac Pain. 2005 Summer;19(3):193-201. PubMed PMID: 16106712.
Peripheral Mechanism
How Does One Assess the Role of Occlusion in TMD?
Ask the patient if her bite feels comfortable and if she can bite evenly on both sides. Have there been any recent changes in the bite (the way the teeth meet)? If so, these are indications that your patient may have an occlusal problem affecting TMD symptoms.
Reference
- Seligman DA, Pullinger AG. The role of functional occlusal relationships in temporomandibular disorders: a review. J Craniomandib Disord. 1991 Fall;5(4):265-79. Review. PubMed PMID: 1814969.
- Seligman DA, Pullinger AG. The role of intercuspal occlusal relationships in temporomandibular disorders: a review. J Craniomandib Disord. 1991 Spring;5(2):96-106. Review. PubMed PMID: 1812142.
What is the Role of Motor Vehicle Accidents (MVA) in TMD?
A patient who undergoes whiplash injury during an MVA oftentimes has multiple injuries that might mask the presence of a TMD injury. Should the TMD problem present within 2-3 months of the whiplash injury, one can consider the MVA to be a contributing factor to the TMD problem.
Reference
Marini I, Paduano S, Bartolucci ML, Bortolotti F, Bonetti GA. The prevalence of temporomandibular disorders in patients with late whiplash syndrome who experience orofacial pain: a case-control series study. J Am Dent Assoc. 2013 May;144(5):486-90. PubMed PMID: 23633696.
TMD Examination and Diagnosis
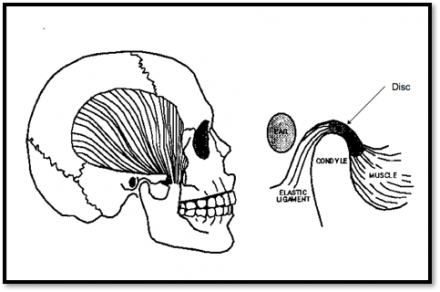
What is Unique About the TMJ?
The TMJ serves as the articulation between the temporal bone and mandibular condyle. The TMJ is a ginglymoarthrodial joint, allowing for both hinge (rotation) and slide (translation) movements of the mandible. The mandibular condyle, temporal bone, articular disc, joint capsule, and ligaments all comprise what we know as the TMJ. The biconcave articular disc, separating the TMJ into superior and inferior compartments, is a unique component of the TMJ. The TMJ’s articular surfaces are composed of dense fibrous cartilage (as opposed to the hyaline cartilage found in most joints), which allows the joint to withstand tensile and compressive forces involved with jaw function.
What makes the TMJ Different?
- Rotation & translation movements
- Bilateral articulation
- Compound joint (2 bones & disc)
- Lined with fibrous cartilage
- Can withstand tensile forces
TMJ Anatomy
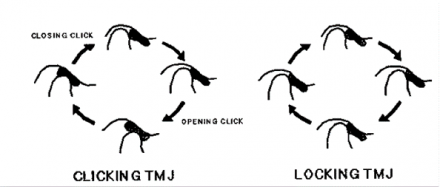
The ligaments that hold the TMJ articular disc in place can become stretched allowing the disc to become anteriorly displaced. This can lead to a ‘clicking jaw’ as the condyle returns to its position under the disc, termed “disc displacement with reduction.” Should the disc not return, the movement of the condyle is limited and termed “disc displacement without reduction.”
Muscle Anatomy
The muscular component of the TMJ is made up of one or more of the following muscle groups:
- Masticatory muscles
- Suprahyoid muscles
- Infrahyoid muscles
- Cervical and other neck muscles
What are the four muscles of mastication?
- Masseter
- Medial pterygoid
- Temporalis
- Lateral pterygoid
The 4 muscles of Mastication
The 4 muscles of mastication and what roles they play in the masticatory system.
| Muscle of Mastiction | Origin | Insertion | Main Action(s) |
|---|---|---|---|
| Masseter |
Superficial: Anterior 2/3 of the zygomatic arch Deep: Posterior 1/3 of the zygomatic arch |
Superficial: angle of the mandible Deep: Lateral ramus |
Elevate mandible |
| Medial Pterygoid | Medial side of lateral pterygoid plate | Angle of the mandible (medial side) |
|
| Temporalis | Inferior temporal line, temporal fossa and fascia | Coronoid process (extending onto the anterior mandibular ramus) |
|
| Lateral Pterygoid |
Superior: Greater wing of the sphenoid Infratemporal crest Inferior: Lateral surface of the lateral pterygoid plate |
Superior: Articular disc and TMJ capsule Inferior: Anterior condylar neck |
|
Table adapted from Norton, N.S., and Netter, F.H. Netter’s Head and Neck Anatomy for Dentistry. Philidelphia, PA: Saunders Elsevier, 2007. Print.
TMD Examination
3-Part Protocol
- Range of Motion
- Palpation
- Auscultation
Differential for Decreased Range of Motion (ROM)
- Myalgia (myofascial pain)
- Disc displacement
- Muscle spasm
- Myositis
- Contracture
- Cranial nerve deficit
Vertical ROM is measured between the end of the upper and lower anterior teeth.

TMJ Assessment: Patterns of Opening
Patterns of opening:
- Straight: normal pattern
- S-Deviation: DD with reduction
- Lateral Deviation: DD without reduction
- Jerky: Osteoarthritis
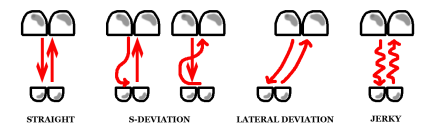
The TMJ begins to translate at about 20 mm of jaw opening. If there is a disc displacement (DD), the jaw opening will deviate to the affected side as the displaced disc prevents further forward advancement on the affected side, but the unaffected side continues its unrestricted advancement resulting in an S-shaped opening pattern. If the displaced disc reduces (DD with reduction) the mandible’s restricted side will start to move forward and will return to midline (see arrow). If the disc does not reduce, the mandible will remain displaced to the affected side (resulting in a lateral deviation) giving the diagnosis of DD without reduction. The “jerky” opening on the far right depicts a pattern consistent with a TMJ with arthritic changes in the joint, which is commonly associated with sounds of course crepitus.
Image from: Fricton JR, Kroening RJ, Hathaway KM: TMJ and Craniofacial Pain: Diagnosis and Management. St. Louis, 1988, Ishiyaku EuroAmerica Inc.pg 46 Figure 5.5 (out of print, permission granted by author)
TMD Exam: TMJ Arthralgia Diagnosis
To confirm diagnosis, the patient must have preauricular pain with at least two of these three maneuvers:
- Palpation
- ROM
- Joint Loading (upwards and/or distal pressure on the mandible)

TMD and Occlusion
Pullinger (1993) evaluated subjects for TMD symptoms and occlusal discrepancies finding the prevalence of TMD to be associated with the following occlusal discrepancies:
- Anterior open bite (space between the upper and lower teeth when biting)
- Overjet (horizontal) anterior-posteriorly > 6 - 7mm between anterior teeth (small lower jaw with “buck” front teeth)
- Centric relation (swallowing position) to normal biting position slide > 2 mm
- Unilateral lingual crossbite (malposition of tooth/teeth causing sideways shift from first tooth contact to normal biting position)
- 5 or more missing posterior teeth

This patient has no tooth contact on her left posterior teeth contributing to an unstable bite.

Reference
- Pullinger AG, Seligman DA. The degree to which attrition characterizes differentiated patient groups of temporomandibular disorders. J Orofac Pain. 1993 Spring;7(2):196-208. PubMed PMID: 8358366.
- Seligman DA, Pullinger AG. The role of functional occlusal relationships in temporomandibular disorders: a review. J Craniomandib Disord. 1991 Fall;5(4):265-79. Review. PubMed PMID: 1814969.
- Seligman DA, Pullinger AG. The role of intercuspal occlusal relationships in temporomandibular disorders: a review. J Craniomandib Disord. 1991 Spring;5(2):96-106. Review. PubMed PMID: 1812142.
Myofascial Pain Diagnosis
The most common TMD diagnosis.

Consider downloading the Apple application for iPhone and iPad “Muscle Trigger Points” written by Read Bodywork Medical.
Reference
Wright EF. Referred craniofacial pain patterns in patients with temporomandibular disorder. J Am Dent Assoc. 2000;131(9):1307-15. http://www.ncbi.nlm.nih.gov/pubmed/?term=10986831
Patterns in Muscle Pain
Classification
- Focal (localized) myalgia
- Regional craniocervical and masticatory myalgia (TMD) = Mrs. Farley’s type
- Widespread chronic muscle pain (such as with fibromyalgia)
Regional and widespread pain can have overlapping features; in some patients, they are considered to be on a continuum rather than existing as distinct entities with different etiologies.
Reference
Temporomandibular disorder and comorbid pain conditions. Lim PF, Maixner W, Khan AA.
J Am Dent Assoc. 2011 Dec;142(12):1365-7. No abstract available. PMID: 22130437 [PubMed - indexed for MEDLINE]
Temporomandibular Disorder: Summary of Terms
Joint
- Arthralgia: pre-auricular pain with at least 2 out of the following 3 maneuvers: palpation, ROM, and/or joint loading
- Disc Displacement Disorders: disorders involving an abnormal position of the intra-articular disc relative to the mandibular condyle and the temporal fossa
- Arthritis: inflammation of the joint, usually accompanied by pain
Muscle
- Myofascial Pain/Dysfunction: regional pain referred from or emanating around active myofascial trigger points
- Myositis: inflammation of muscle tissue
- Spasm: spasmodic continuous involuntary contraction of a muscle, typically causing acute pain
- Contracture: sustained increased resistance to passive muscle stretch due to reduced muscle length
Evaluation of Temporomandibular Disorders
Mrs. Farley revealed numerous signs and symptoms of a temporomandibular disorder.
| Signs and Symptoms | Mrs. Farley's Problem List |
|---|---|
| Limited ROM | Yes, pain-free ROM is limited |
| Deviation on opening/closing | No |
| Pain with vertical ROM | Yes, in anterior temporalis, masseter and TMJ |
| Pain with lateral TOM | Yes, could be from muscle or joint |
| Pain while eating | Yes, in masseter |
| Tender muscles of mastication | Yes, duplicating jaw pain and headache (masseter, temporalis, medial pterygoid) |
| Tender TMJ | Yes, but not consistent with chief complaint (CC) |
TMD Treatment
Example TMD Multi-modal Treatment Plan for Mrs. Farley
| Treatment | Examples and Treatment Descriptions |
|---|---|
| Home exercise program | Exercises to increase ROM within pain tolerance |
| Physical therapy | Modalities to reduce pain, develop exercise regimen 2-3 x per week x 3-4 weeks. Ensure treatment compliance. |
| NSAIDS | To control acute myalgia symptoms; 600-800 mg ibuprofen TID, 10-day regimen for arthragia |
| Neuropathic medications (can also help with sleep) | Consider gabapentin, pregablin, amitriptyline 10-30 mg HS |
| Muscle relaxants | Cyclobenzaprine (Flexeril) 5-10 mg TID |
| Anxiolytics | Consider anti-anxiety medication if indicated |
| Occlusal appliance | Mandibular stabilization appliance providing even bite to control night-time parafuction and provide stable (even) occlusion bilaterally on posterior teeth. It can be worn during the day to assess the role of unstable occlusion in TMD symptoms |
| Injections; trigger point injections (TPIs), nerve blocks, Botox | If unresponsive to standard therapy and pain is localized to masticatory myofascial trigger points, consider TPI’s. If pain is more regional and/or neuropathic, consider nerve blocks. |
| Behavioral therapy (BT) | Cognitive BT relaxation training, mental health evaluation |
| Hypnosis, acupuncture, laser | Baad-Hansen 2013, Jung 2011, Petrucci 2011, Koh 2003 |
References
- List T, Axelsson S. Management of TMD: evidence from systematic reviews and meta-analyses. J Oral Rehabil. 2010 May;37(6):430-51. doi:10.1111/j.1365-2842.2010.02089.x. Epub 2010 Apr 20. Review. PubMed PMID:20438615.
- Sturdivant J, Fricton JR. Physical therapy for temporomandibular disorders and orofacial pain. Curr Opin Dent. 1991 Aug;1(4):485-96. Review. PubMed PMID:1802010.
- Mujakperuo HR, Watson M, Morrison R, Macfarlane TV. Pharmacologicalinterventions for pain in patients with temporomandibular disorders. Cochrane Database Syst Rev. 2010 Oct 6;(10):CD004715. doi: 10.1002/14651858.CD004715.pub2. Review. PubMed PMID: 20927737.
- Wynn RL. Over-the-counter ibuprofen and acetaminophen in combination are superior to each agent alone in treating postoperative pain. Gen Dent. 2012 May-Jun;60(3):176-8. PubMed PMID: 22623453.
- Wynn RL. Ketorolac nasal spray--a new formulation of this non-narcotic pain reliever. Gen Dent. 2012 Mar-Apr;60(2):90-2. Review. PubMed PMID: 22414499.
- Herman CR, Schiffman EL, Look JO, Rindal DB. The effectiveness of adding pharmacologic treatment with clonazepam or cyclobenzaprine to patient education and self-care for the treatment of jaw pain upon awakening: a randomized clinical trial. J Orofac Pain. 2002 Winter;16(1):64-70. PubMed PMID: 11889661.
- Gonzalez LA, Gatch MB, Forster MJ, Dillon GH. Abuse Potential of Soma: the GABA(A) Receptor as a Target. Mol Cell Pharmacol. 2009 Jan 1;1(4):180-186. PubMed PMID: 20419052; PubMed Central PMCID: PMC2858432.
- Arnold LM, Clauw DJ, Dunegan LJ, Turk DC; FibroCollaborative. A framework for fibromyalgia management for primary care providers. Mayo Clin Proc. 2012 May;87(5):488-96. doi: 10.1016/j.mayocp.2012.02.010. Review. PubMed PMID: 22560527; PubMed Central PMCID: PMC3498162.
- Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular joint disorders. Cochrane Database Syst Rev. 2003;(1):CD003812. Review. PubMed PMID: 12535488.
- Macedo CR, Silva AB, Machado MA, Saconato H, Prado GF. Occlusal splints for treating sleep bruxism (tooth grinding). Cochrane Database Syst Rev. 2007 Oct 17;(4):CD005514. Review. PubMed PMID: 17943862.
- Klasser GD, Greene CS, Lavigne GJ. Oral appliances and the management of sleep bruxism in adults: a century of clinical applications and search for mechanisms. Int J Prosthodont. 2010 Sep-Oct;23(5):453-62. Review. PubMed PMID: 20859563.
- Hong CZ. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am J Phys Med Rehabil. 1994 Jul-Aug;73(4):256-63. PubMed PMID: 8043247.
- Scicchitano J, Rounsefell B, Pilowsky I. Baseline correlates of the response to the treatment of chronic localized myofascial pain syndrome by injection of local anaesthetic. J Psychosom Res. 1996 Jan;40(1):75-85. PubMed PMID: 8730647.
- Annaswamy TM, De Luigi AJ, O'Neill BJ, Keole N, Berbrayer D. Emerging concepts in the treatment of myofascial pain: a review of medications, modalities, and needle-based interventions. PM R. 2011 Oct;3(10):940-61. doi: 10.1016/j.pmrj.2011.06.013. Review. PubMed PMID: 22024326.
- Gerwin R. Botulinum toxin treatment of myofascial pain: a critical review of the literature. Curr Pain Headache Rep. 2012 Oct;16(5):413-22. doi: 10.1007/s11916-012-287-6. Review. PubMed PMID: 22777564.
- Soares A, Andriolo RB, Atallah AN, da Silva EM. Botulinum toxin for myofascial pain syndromes in adults. Cochrane Database Syst Rev. 2012 Apr 18;4:CD007533. doi: 10.1002/14651858.CD007533.pub2. Review. PubMed PMID: 22513950.
- Baad-Hansen L, Abrahamsen R, Zachariae R, List T, Svensson P. Somatosensory sensitivity in patients with persistent idiopathic orofacial pain is associated with pain relief from hypnosis and relaxation. Clin J Pain. 2013
- Jun;29(6):518-26. doi: 10.1097/AJP.0b013e318268e4e7. PubMed PMID: 23328326. Jung A, Shin BC, Lee MS, Sim H, Ernst E. Acupuncture for treating temporomandibular joint disorders: a systematic review and meta-analysis of randomized, sham-controlled trials. J Dent. 2011 May;39(5):341-50. doi: 10.1016/j.jdent.2011.02.006. Epub 2011 Feb 25. Review. PubMed PMID: 21354460.
- Petrucci A, Sgolastra F, Gatto R, Mattei A, Monaco A. Effectiveness of low-level laser therapy in temporomandibular disorders: a systematic review and meta-analysis. J Orofac Pain. 2011 Fall;25(4):298-307. Review. PubMed PMID:22247925.
- Koh HL, Teo HH, Ng HL. Pharmacists' patterns of use, knowledge, and attitudes toward complementary and alternative medicine. J Altern Complement Med. 2003 Feb;9(1):51-63. PubMed PMID: 12676035.
Standard TMD Therapy
Standard TMD therapy includes physical therapy (PT), appliance therapy, home exercise programs, behavioral therapy, control of parafunctional habits (such as bruxism and daytime clenching), and medication use (analgesics, sleep medications, muscle relaxants, anxiolytics) should be considered routine for initial TMD therapy.
References
- Fricton JR. Clinical care for myofascial pain. Dent Clin North Am. 1991 Jan;35(1):1-28. Review. PubMed PMID: 1997346
- List T, Axelsson S. Management of TMD: evidence from systematic reviews and meta-analyses. J Oral Rehabil. 2010 May;37(6):430-51. doi: 10.1111/j.1365-2842.2010.02089.x. Epub 2010 Apr 20. Review. PubMed PMID: 20438615.
- Cairns BE. Pathophysiology of TMD pain--basic mechanisms and their implications for pharmacotherapy. J Oral Rehabil. 2010 May;37(6):391-410. doi:10.1111/j.1365-2842.2010.02074.x. Epub 2010 Mar 10. Review. PubMed PMID: 20337865.
Medications Effective for TMD
Some examples include: Non-steroidal anti-inflammatory drugs (NSAIDs) or other analgesics for acute pain episodes; muscle relaxants for acute muscle pain; sleep medications can help control night-time parafunction; a 10-day regimen of anti-inflammatory medication or a Medrol (steroid) dose pack for TMJ arthralgia.
References
- Tchivileva IE, Lim PF, Smith SB, Slade GD, Diatchenko L, McLean SA, Maixner W. Effect of catechol-O-methyltransferase polymorphism on response to propranolol therapy in chronic musculoskeletal pain: a randomized, double-blind, placebo-controlled, crossover pilot study. Pharmacogenet Genomics. 2010 Apr;20(4):239-48. doi: 10.1097/FPC.0b013e328337f9ab. PubMed PMID: 20216107; PubMed Central PMCID: PMC2876724.
- Mujakperuo HR, Watson M, Morrison R, Macfarlane TV. Pharmacological interventions for pain in patients with temporomandibular disorders. Cochrane Database Syst Rev. 2010 Oct 6;(10):CD004715. doi: 10.1002/14651858.CD004715.pub2. Review. PubMed PMID: 20927737.
- Herman CR, Schiffman EL, Look JO, Rindal DB. The effectiveness of adding pharmacologic treatment with clonazepam or cyclobenzaprine to patient education and self-care for the treatment of jaw pain upon awakening: a randomized clinical trial. J Orofac Pain. 2002 Winter;16(1):64-70. PubMed PMID: 11889661.
- Annaswamy TM, De Luigi AJ, O'Neill BJ, Keole N, Berbrayer D. Emerging concepts in the treatment of myofascial pain: a review of medications, modalities, and needle-based interventions. PM R. 2011 Oct;3(10):940-61. doi:10.1016/j.pmrj.2011.06.013. Review. PubMed PMID: 22024326.
Goal of TMD Treatment
The goal of TMD treatment is to improve pain-free jaw ROM while giving the patient control of his/her TMD symptoms with the use of reversible therapies.
When are Occlusal Treatments Indicated?
Acute TMD symptoms after restorative dentistry can indicate the need for immediate adjustment of dental restorations. Appliance (night guard) therapy is a reversible way to stabilize the occlusion. Definitive occlusal treatments are done as a last resort, and then only if the patient is dependent on appliance wear to control TMD symptoms.
References
- Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular joint disorders. Cochrane Database Syst Rev. 2003;(1):CD003812. Review. PubMed PMID: 12535488.
- Macedo CR, Silva AB, Machado MA, Saconato H, Prado GF. Occlusal splints for treating sleep bruxism (tooth grinding). Cochrane Database Syst Rev. 2007 Oct 17;(4):CD005514. Review. PubMed PMID: 17943862.
- Klasser GD, Greene CS, Lavigne GJ. Oral appliances and the management of sleep bruxism in adults: a century of clinical applications and search for mechanisms. Int J Prosthodont. 2010 Sep-Oct;23(5):453-62. Review. PubMed PMID: 20859563.
When is Physical Therapy (PT) and Behavioral Therapy (BT) Indicated?
Initially, the patient’s response to a home regimen designed to promote an increase in pain-free ROM via exercises and control of parafunctional habits is assessed. In cases with persistent pain (e.g. pain score > 5/10), PT and BT are indicated. PT and BT should be included in all complex TMD cases.
References
- De Laat A, Stappaerts K, Papy S. Counseling and physical therapy as treatment for myofascial pain of the masticatory system. J Orofac Pain. 2003 Winter;17(1):42-9. PubMed PMID: 12756930.
- Carlson CR, Bertrand PM, Ehrlich AD, Maxwell AW, Burton RG. Physical self-regulation training for the management of temporomandibular disorders. J Orofac Pain. 2001 Winter;15(1):47-55. PubMed PMID: 11889647.
What Success Can One Expect From TMD Treatment?
Evidence indicates that 80% of patients with TMD will respond to standard TMD therapy. For the 20% who do not respond, ensure the following:
- the correct diagnosis has been made
- the patient is complying with the treatment plan
- all contributing factors are being addressed
References
- Ohrbach R, Fillingim RB, Mulkey F, Gonzalez Y, Gordon S, Gremillion H, Lim PF, Ribeiro-Dasilva M, Greenspan JD, Knott C, Maixner W, Slade G. Clinical findings and pain symptoms as potential risk factors for chronic TMD: descriptive data and empirically identified domains from the OPPERA case-control study. J Pain. 2011 Nov;12(11 Suppl):T27-45. doi: 10.1016/j.jpain.2011.09.001. PubMed PMID: 22074750; PubMed Central PMCID: PMC3443556.
- Fricton JR. Clinical care for myofascial pain. Dent Clin North Am. 1991 Jan;35(1):1-28. Review. PubMed PMID: 1997346.
- Rammelsberg P, LeResche L, Dworkin S, Mancl L. Longitudinal outcome of temporomandibular disorders: a 5-year epidemiologic study of muscle disorders defined by research diagnostic criteria for temporomandibular disorders. J Orofac Pain. 2003 Winter;17(1):9-20. PubMed PMID: 12756926.
Mrs. Farley's Symptom Classification
| Mrs. Farley's Symptoms | Myofascial | Arthragia | Neuropathic |
|---|---|---|---|
| Limited ROM (33mm w/out pain increase; 43mm w/ pain increase; 6mm bilaterally) | Yes, ROM can be increased via passive stretching | Preauricular arthralgia pain occurs in lateral and vertical ROM | |
| Deep, aching, and throbbing pain (relatively constant) right side | Yes, but pain should be aggravated only with jaw function | Constant pain can be of neuropathic nature | |
| Occasional sharp, shooting pain from masseter muscle | Can occur with increase in muscle pain severity | Typically sharp, shooting pain occurs preauricularly during jaw function | Spontaneous muscle or TMJ pain is consistent with neuropathic pain |
| Jaw pain worse in morning upon waking | Typical of pain aggravated by night-time parafunction | Typical of pain from night-time parafunction | |
| Widespread body pain worse at the end of day | Yes | ||
| Pain wakes her up at night | Unusual | Unusual | Consider tumor |
| Temporal headache after jaw function | Yes, a typical presentation | Can be related to arthralgia |
|
Special Considerations for Management of the Chronic TMD Patient
How do you distinguish between a simple (responds to standard treatment) and a complex TMD patient (one who requires inter-disciplinary care)?
- Complex patients present with one or more of the following characteristics: greater than 5 out of 10 pain of longer than a 3-month duration, multiple diagnoses, poor sleep, history of mental health problems, and/or severe parafunctional habits.
What are some comorbidities that are associated with TMD?
- Chronic headaches, irritable bowel syndrome (IBS), and fibromyalgia (FM) can be associated with TMD. When these are present, one should consider a pain processing problem, i.e., neuropathic pain.
References
- Lim PF, Maixner W, Khan AA. Temporomandibular disorder and comorbid pain conditions. J Am Dent Assoc. 2011 Dec;142(12):1365-7. PubMed PMID: 22130437.
- John MT, Miglioretti DL, LeResche L, Von Korff M, Critchlow CW. Widespread pain as a risk factor for dysfunctional temporomandibular disorder pain. Pain. 2003 Apr;102(3):257-63. PubMed PMID: 12670667.
- Yunus MB. Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes. Semin Arthritis Rheum. 2007 Jun;36(6):339-56. Epub 2007 Mar 13. Review. PubMed PMID: 17350675.
- Velly AM, Fricton J. The impact of comorbid conditions on treatment of temporomandibular disorders. J Am Dent Assoc. 2011 Feb;142(2):170-2. PubMed PMID: 21282683.
- King CD, Wong F, Currie T, Mauderli AP, Fillingim RB, Riley JL 3rd. Deficiency in endogenous modulation of prolonged heat pain in patients with Irritable Bowel Syndrome and Temporomandibular Disorder. Pain. 2009 Jun;143(3):172-8. doi: 10.1016/j.pain.2008.12.027. Epub 2009 Mar 10. PubMed PMID: 19278784; PubMed Central PMCID: PMC3629692.
- Schiffman E, Ohrbach R, List T, Anderson G, Jensen R, John MT, Nixdorf D, Goulet JP, Kang W, Truelove E, Clavel A, Fricton J, Look J. Diagnostic criteria for headache attributed to temporomandibular disorders. Cephalalgia. 2012 Jul;32(9):683-92. doi: 10.1177/0333102412446312. PubMed PMID: 22767961.
- List T, John MT, Ohrbach R, Schiffman EL, Truelove EL, Anderson GC. Influence of temple headache frequency on physical functioning and emotional functioning in subjects with temporomandibular disorder pain. J Orofac Pain. 2012 Spring;26(2):83-90. PubMed PMID: 22558607.
Contributing Factors and How they Affect Treatment
Different types of contributing factors (anatomical, behavioral, social, emotional, environmental, and cognitive) interact in human systems theory and impact patients’ pain perception.
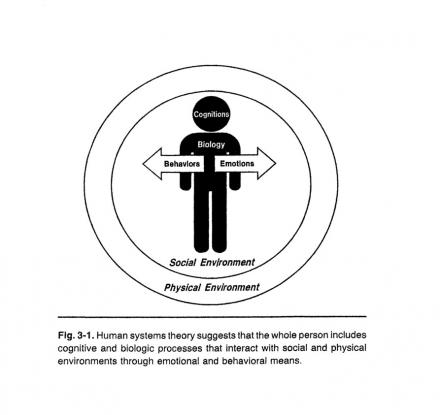
Image from: Fricton JR, Kroening RJ, Hathaway KM: TMJ and Craniofacial Pain: Diagnosis and Management. St. Louis, 1988, Ishiyaku EuroAmerica Inc.pg ? Figure 3.1 (out of print, permission granted by author)
Bruxism
What is bruxism? How do you determine if a patient does it?
- Bruxism refers to night-time grinding but can occur during the day. Tooth wear (especially on posterior teeth), hyperkeratosis on the intraoral mucosa along the occlusal line, tongue ridging, and morning symptoms can be predictors. The best predictor is patient self-report of grinding or clenching at night. 80% of parafanction at night involves clenching (compared to 20% grinding).
Reference
Klasser GD, Greene CS, Lavigne GJ. Oral appliances and the management of sleep bruxism in adults: a century of clinical applications and search for mechanisms. Int J Prosthodont. 2010 Sep-Oct;23(5):453-62. Review. PubMed PMID: 20859563
Poor Sleep
How is poor sleep a factor in fibromyalgia compared to TMD?
- As in any musculoskeletal problem, restful sleep is critical to promote healing in TMD. Ask if the problem is falling or staying asleep, provide sleep hygiene instructions, and consider medications to encourage restful sleep.
References
- Haack M, Mullington JM. Sustained sleep restriction reduces emotional and physical well-being. Pain. 2005 Dec 15;119(1-3):56-64. Epub 2005 Nov 16. PubMed PMID: 16297554.
- Davies KA, Macfarlane GJ, Nicholl BI, Dickens C, Morriss R, Ray D, McBeth J. Restorative sleep predicts the resolution of chronic widespread pain: results from the EPIFUND study. Rheumatology (Oxford). 2008 Dec;47(12):1809-13. doi: 10.1093/rheumatology/ken389. Epub 2008 Oct 7. PubMed PMID: 18842606; PubMed Central PMCID: PMC2582170.
- Pimentel MJ, Gui MS, Martins de Aquino LM, Rizzatti-Barbosa CM. Features of temporomandibular disorders in fibromyalgia syndrome. Cranio. 2013 Jan;31(1):40-5. PubMed PMID: 23461261.
Is TMD a Psychological Diagnosis?
For both simple and complex TMD patients, the presence of psychosocial factors must be assessed and controlled.
References
- Yoshihara T, Shigeta K, Hasegawa H, Ishitani N, Masumoto Y, Yamasaki Y. Neuroendocrine responses to psychological stress in patients with myofascial pain. J Orofac Pain. 2005 Summer;19(3):202-8. PubMed PMID: 16106713.
- Korszun A, Young EA, Singer K, Carlson NE, Brown MB, Crofford L. Basal circadian cortisol secretion in women with temporomandibular disorders. J Dent Res. 2002 Apr;81(4):279-83. PubMed PMID: 12097314.
Characteristics of Neuropathic Pain
- Spontaneous
- Allodynia
- Hyperalgesia
References
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011 Mar;152(3 Suppl):S2-15. doi: 10. 20961685; PubMed Central PMCID: PMC3268359. 1016/j.pain.2010.09.030. Epub 2010 Oct 18. Review. PubMed PMID:
- Hughes JP, Chessell I, Malamut R, Perkins M, Bačkonja M, Baron R, Farrar JT, Field MJ, Gereau RW, Gilron I, McMahon SB, Porreca F, Rappaport BA, Rice F, Richman LK, Segerdahl M, Seminowicz DA, Watkins LR, Waxman SG, Wiech K, Woolf C. Understanding chronic inflammatory and neuropathic pain. Ann N Y Acad Sci. 2012 May;1255:30-44. doi: 10.1111/j.1749-6632.2012.06561.x. PubMed PMID68: 225640.
Mrs. Farley’s TMD Diagnosis Summary
Why rule out arthralgia?
- Mrs. Farley has adequate lateral range of motion, and although there are positive findings to TMJ palpation, her symptoms (familiar pain) are best reproduced with muscle palpation.
Why rule out contraction and spasm?
- Due to Mrs. Farley’s moderate pain level and ability to stretch muscle to increase range of motion.
Why is the myofascial pain diagnosis supported?
- Mrs. Farley has a moderate pain level aggravated with function; her headache pain was duplicated with trigger point palpation, i.e., referred pain during muscle palpation causing familiar pain - a key characteristic of myofascial pain.
Does Mrs. Farley have neuropathic pain?
- With her co-morbidity of fibromyalgia, yes. Also her constant moderate-to-severe pain, nocturnal symptoms, and spontaneous pain have neuropathic qualities. However, she can still benefit from treatments tailored to her TMD diagnosis.

