Fibromyalgia: Fact or Fiction?
Many people are unsure about what fibromyalgia is, and this next section will help you to describe fibromyalgia.
Test Your Knowledge
Question 1
Fibromyalgia is primarily a psychiatric diagnosis.
Question 2
Fibromyalgia is caused primarily by peripheral mechanisms.
Question 3
Fibromyalgia is diagnosed by physical exam and palpation of tender point sites.
Question 4
Fibromyalgia patients exhibit changes in neurotransmitter levels that cause decreased central nervous system pain processing.
Question 5
Patients with fibromyalgia often report heightened energy.
Question 6
Fibromyalgia is defined by pain in muscles of the neck and back.
Question 7
Patients with fibromyalgia have hyperalgesia and allodynia.
Question 8
There are no FDA-approved medications for fibromyalgia.
References
- Clauw DJ, Arnold LM, McCarberg BH; FibroCollaborative. The science of fibromyalgia. Mayo Clin Proc. 2011; 86(9):907-11. PMID: 21878603
- Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MB. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 2010; 62(5):600-10. PMID: 20461783
Fibromyalgia Background
- Fibromyalgia is a scientifically proven disease with well-studied treatment management strategies, contrary to the frequent misconception that it is “poorly understood”
- Men also have fibromyalgia; however, incidence in women is higher. Male : female ratio estimated at 1 : 2-3
- Most prominent symptom is chronic widespread pain
- Pain is characterized by allodynia and hyperalgesia
References
- Branco JC, Bannwarth B, Failde I, Abello Carbonell J, Blotman F, Spaeth M, Saraiva F, Nacci F, Thomas E, Caubère JP, Le Lay K, Taieb C, Matucci-Cerinic M. Prevalence of fibromyalgia: a survey in five European countries. Semin Arthritis Rheum 2010; 39(6):448-53. PMID: 19250656
- Arnold LM, Clauw DJ, McCarberg BH; FibroCollaborative. Improving the recognition and diagnosis of fibromyalgia. Mayo Clin Proc. 2011; 86(5):457-64. PMID: 21531887
- Arnold LM, Clauw DJ, Dunegan LJ, Turk DC; FibroCollaborative. A framework for fibromyalgia management for primary care providers. Mayo Clin Proc. 2012; 87(5):488-96. PMID: 22560527
Allodynia and Hyperalgesia
Allodynia is defined as pain due to a stimulus that does not normally cause pain (e.g., light touch or clothing rubbing over skin is painful in someone who has allodynia).
Hyperalgesia is defined as increased pain from a stimulus that does normally causes pain (e.g., extreme pain during placement of an intravenous line would be seen in someone with hyperalgesia; a person without hyperalgesia would feel discomfort and perhaps pain but not perceive it as extremely painful).
Fibromyalgia Pathophysiology
Postulated Pain Signaling Mechanism
Central nervous system neurochemical imbalances (peripheral impulses: e.g., muscle inflammation) lead to central amplification, hyper-excitability of pain perception, which lead to maintenance of pain, which cycles back to central nervous system neurochemical imbalances, starting the cycle over again.
Central Sensitization or Central Amplification
When discussing a patient with fibromyalgia and chronic pain, the term “central sensitization” or “central amplification” is often used to explain how the patient’s pain is maintained.
Central Sensitization and Fibromyalgia
Evidence suggests that ascending and descending pain pathways operate abnormally in fibromyalgia, resulting in central amplification of pain signals.
References
- Staud R, Robinson ME, Price DD. Temporal summation of second pain and its maintenance are useful for characterizing widespread central sensitization of fibromyalgia patients. J Pain. 2007; 8(11):893-901. PMID: 17681887
- Desmeules JA, Cedraschi C, Rapiti E, Baumgartner E, Finckh A, Cohen P, Dayer P, Vischer TL. Neurophysiologic evidence for a central sensitization in patients with fibromyalgia. Arthritis Rheum 2003;48:1420–9. PubMed: 12746916
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 Suppl):S2-15. Epub 2010/10/22. doi: 10.1016/j.pain.2010.09.030. PubMed PMID: 20961685
Central Amplification and Fibromyalgia
This can be thought of as if the patient’s pain perception “volume control setting” is turned up too high. A patient without chronic pain would interpret the same pain signal at a lower “volume” setting.
Fibromyalgia Brain Imaging
Patients with fibromyalgia have been compared to patients without chronic pain using functional magnetic resonance imaging (fMRI) of the brain. Pain processing is clearly different.
fMRI has shown that fibromyalgia is associated with aberrant processing of painful stimuli in the central nervous system (i.e., when compared to a non-pain patient, areas responsible for pain signaling light up more in a fibromyalgia brain when a painful stimulus is applied to a patient. Patients with fibromyalgia also perceive increased pain at lower thresholds of pressure when compared to patients without chronic pain.)
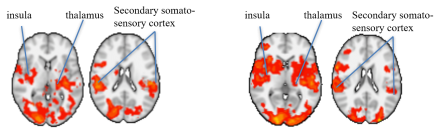
Images courtesy of Dr. Robert Edwards, Brigham and Women’s Hospital
Reference
Jorge LL, Amaro E Jr. Brain imaging in fibromyalgia. Curr Pain Headache Rep.2012 Oct;16(5):388-98 PMID: 22717698.
Diagnosing Fibromyalgia
Fibromyalgia is a “real” disease, and the brain processes pain differently in patients with fibromyalgia when compared to patients without the disease.
How do you diagnose it?
- Criteria for diagnosing fibromyalgia used to involve identifying at least 11 of 18 tender point sites on a patient during a physical exam.
- In 2010, the criteria were restructured by the American College of Rheumatology in order to develop simple and practical criteria suitable for use in primary and other specialty care.
- A diagnosis of fibromyalgia is made using symptom scales and a widespread pain index score – no physical exam is required.
Reference
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MS. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 2010; 62(5):600-10. PMID: 20461783
How Would You Diagnose Fibromyalgia in Mrs. Farley?
Diagnosis made by using the following indices:
- Widespread pain index (WPI) – patient indicates how many body areas are painful (19 areas of the body are listed)
- Symptom Severity (SS) scale (scale ratings of fatigue, waking unrefreshed, and cognitive symptoms)
- Patient does not have any other disorders that would explain the pain. (Click here to see a fibromyalgia disease differential.)
Reference
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MS. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 2010; 62(5):600-10. PMID: 20461783
Fibromyalgia Disease Differential
Other diseases to consider and exclude when diagnosing fibromyalgia:
- Hypothyroidism
- Polymyalgia rheumatica
- Autoimmune disorders (rheumatoid arthritis, systemic lupus erythematosus (SLE), ankylosing spondylitis)
- Sjogren's syndrome
- Neuropathies
- Myositis, myopathies (localized)
- Irritable bowel syndrome
- Tension and migraine headache
- Infectious processes
- Obstructive sleep apnea
Reference
Goldenberg DL. Diagnosis and differential diagnosis of fibromyalgia. Am J Med 2009; 122(12 Suppl):S14-21. PMID: 19962492
Fibromyalgia Diagnosis
In summary, a patient satisfies diagnostic criteria for fibromyalgia if the following 3 conditions are met:
- Widespread pain index (WPI) ≥ 7 and symptom severity (SS) scale score ≥ 5 or WPI 3-6 and SS scale score ≥ 9.
- Symptoms have been present at a similar level for at least 3 months.
- The patient does not have a disorder that would otherwise explain the pain.
Reference
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MS. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 2010; 62(5):600-10. PMID: 20461783
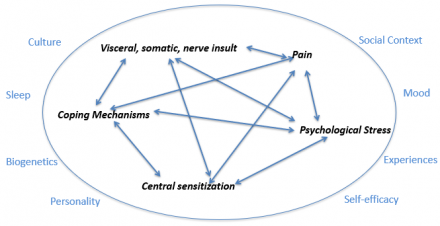
Co-existing Pain Problems and Central Nervous System Dysfunction
Many patients like Mrs. Farley have co-existing pain problems (such as TMD and fibromyalgia) and mood disorders. Explanations for this include the following:
- Central nervous system dysfunction affects general pain processing
- Increased pain signaling amplifies and perpetuates signaling in other pain disorders
References
- Pimentel MJ, Gui MS, Martins de Aquino LM, Rizzatti-Barbosa CM. Features of temporomandibular disorders in fibromyalgia syndrome. Cranio 2013; ;31(1):40-5. PMID: 23461261
- Plesh O, Adams SH, Gansky SA. Temporomandibular joint and muscle disorder-type pain and comorbid pains in a national US sample. J Orofac Pain 2011; 25(3):190-8. PMID: 21837286
Co-existing Systemic Disorders Overlapping with Fibromyalgia
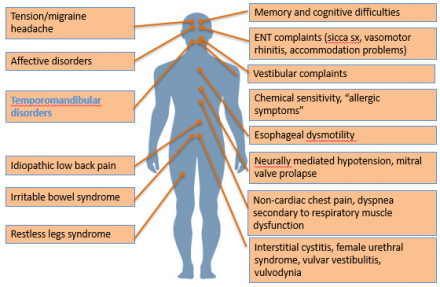
Diagram adapted from Clauw DJ. “Chapter 26: Fibromyalgia” in Bonica’s Management of Pain. 4th edition. Lippincott Williams & Wilkins. 2010
Facts About Gender Differences and Pain
There is epidemiologic evidence indicating that many pain disorders disproportionately affect women, such as TMD and fibromyalgia, but pain perception and experience are not unequivocally influenced by gender.
- Studies on gender differences and pain present conflicting results.
- Gender differences and pain experience are clearly complex issues.
- Gender is one of many patient-specific factors that may modulate pain perception.
- An Institute of Medicine Report (2011) stated that women appear to suffer more from pain, and women’s reports of pain are more likely to be dismissed.
- A systematic review (Racine et al., 2012) of laboratory research and biopsychosocial factors on pain and gender did not show a clear and consistent pattern of sex differences in human pain sensitivity.
- In contrast, another review (Mogil, 2012) of gender differences and pain asserts that “the evidence is actually overwhelmingly in support of the contention that women are more sensitive to pain, although the size and importance of this sex difference could be debated.”
- Some evidence suggests that pain treatment responses may differ for women when compared to men.
- A 2012 study on gender differences in pain severity, disability, depression, and widespread pressure pain sensitivity in patients with fibromyalgia concluded the following:
- Women with fibromyalgia show higher pain severity and lower pressure pain thresholds
- Men with fibromyalgia show longer duration of symptoms and disability
Gender is one of many patient-specific factors that
may modulate pain perception and treatment targets…
References
- Institute of Medicine Report (2011) “Relieving Pain in America.”
- Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choinière M. A systematic literature review of 10 years of research on sex/gender and experimental pain perception – part 1: are there really differences between women and men? Pain. 2012; 153(3):602-18. PMID: 22192712
- Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choinière M. A systematic literature review of 10 years of research on sex/gender and experimental pain perception – part 2: do biopsychosocial factors alter pain sensitivity differently in women and men? Pain. 2012; 153(3):619-35. PMID: 22236999
- Mogil JS. Sex differences in pain and pain inhibition: multiple explanations of a controversial phenomenon. Nat Rev Neurosci. 2012; 13(12):859-66. PMID: 23165262
- Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL 3rd. Sex, Gender, and Pain: A Review of Recent Clinical and Experimental Findings J Pain. 2009; 10(5):447-85. PMID: 19411059
- Castro-Sánchez AM, Matarán-Peñarrocha GA, López-Rodríguez MM, Lara-Palomo IC, Arendt-Nielsen L, Fernández-de-las-Peñas C. Gender differences in pain severity, disability, depression, and widespread pressure pain sensitivity in patients with fibromyalgia syndrome without comorbid conditions. Pain med 2012; 13(12):1639-47. PMID: 23171037
Psychological Factors and Pain
Test Your Knowledge
Question 1
Which statement is correct?
Question 2
Patients who have chronic pain with low psychopathology have been found to have a _____ % greater reduction in pain with intravenous morphine when compared to patients with high psychopathology.
Question 3
Chronic pain patients with a major mood disorder tend to have:
References
- Arola HM, Nicholls E, Mallen C, Thomas E. Self-reported pain interference and symptoms of anxiety and depression in community-dwelling older adults: can a temporal relationship be dtermined? Eur J Pain 2010; 14:966-971.
- Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med 2003; 163(20):2433-45. PMID: 14609780
- Dworkin SF, Von Korff M, LeResche L. Multiple pains and psychiatric disturbance. An epidemiologic investigation. Arch Gen Psychiatry 1990; 47(3):239-44. PMID: 2306165
- Wasan AD, Davar G, Jamison R. The association between negative affect and opioid analgesia in patients with discogenic low back pain. Pain 2005; 117(3):450-61. PMID: 16154274.
Depression, Catastrophizing, and Pain
- “Psychogenic” pain (“pain in your head”) is a concept that has fortunately been abandoned.
- However, it is important to recognize that negative emotional processes such as anxiety, depression, and catastrophizing can increase levels of pain perceived by patients and lead to increased disability and morbidity.
- Research has shown that patients with depression and pain do not respond as well to pain medications such as morphine – patients without depression showed a 40% greater reduction in pain versus patients with co-morbid depression (Wasan et al).
Pain Catastrophizing Scale available FREE access at http://sullivan-painresearch.mcgill.ca/pcs.php
Catastrophizing comprises a specific set of pain-related cognitive and emotional processes reflecting patients’ degree of helplessness when in pain, their tendency to ruminate about and magnify pain, and their propensity to magnify the threat value of pain.
Catastrophizing and depression are common in fibromyalgia and other pain disorders and are risk factors for adverse pain-related outcomes such as physical disability, increased severity of pain, enhanced pain sensitivity, and other morbidities.
Recognizing anxiety, depression, and catastrophizing in a patient with chronic pain, like Mrs. Farley, is important in order to address pain treatment targets and individualized management strategies.
References
- Edwards RR, Cahalan C, Mensing G, Smith M, Haythornthwaite JA. Pain, catastrophizing, and depression in the rheumatic diseases. Nat Rev Rheumatol 2011; 7(4):216-24. PMID: 21283147
- Wasan AD, Davar G, Jamison R. The association between negative affect and opioid analgesia in patients with discogenic low back pain. Pain 2005; 117(3):450-61. PMID: 16154274.
Psychosocial and Psychological Factors and Pain
Click here link Psychosocial and Psychological Factors and Pain
Pain is a subjective experience involving the body, mind, spirit, and social interactions.
- Potential factors contributing to pain and distress at the level of the body
- Ongoing inflammation, muscle spasm, deconditioning, nerve sensitization
- Suboptimal diet, sleep, exercise patterns
- Suboptimal medication utilization pattern
- Potential factors contributing to pain and distress at level of the mind
- Anxiety, depressed mood, high levels of daily stress
- Maladaptive coping (illness behaviors), fear - avoidance patterns
- Self-doubts ability to manage pain, fulfill role expectations, and cope with pain
- Potential factors contributing to pain and distress at social and spiritual level
- Socially isolated, relationship/role conflict, suffering without meaning
- Overly dependent on unhelpful healthcare and family supports in place
- Lost connections with social supports, energy imbalance, unexplored losses
Healthcare providers need to gain additional insight about what Mrs. Farley values most and derives energy from.
Patient's Pain Experience is Complex
All of these factors need to be considered within the biopsychosocial context of the individual.