Surgical Team Unit Meeting
The surgical team discusses Mrs. Smith's refusal of an epidural for surgery.
After watching the video, you may wonder about the depth of knowledge needed about medications. Jenny addresses this subject:
Test Your Knowledge
How else could Jenny have described Carol so that she was more respectful?
Strategies to Reduce Medication Errors
- Strategies to implement
- Education programs
- Written information on medications available on all patient care units
- Detailed policies and procedures for prescribing
- Standardized concentration for all opioids
- Independent double-checks on initiation of therapy and with all setting changes
Reference
Moss J. Joint Commission Journal on Quality and Patient Safety. 2010;36(8):359-364
Surgical Unit Team Meeting: Erin
Erin will be the patient’s clinical nurse. She is prepared to report on Mrs. Smith’s comprehensive monitoring plan of care based on evidence-based practice guidelines.
Pain During Hospitalization Predicts Long-Term Pain at 6 Months
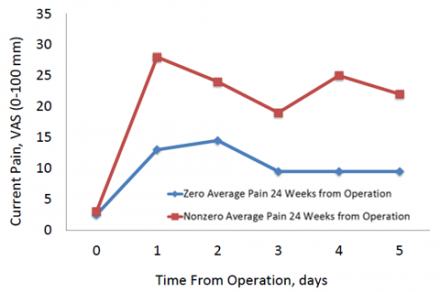
Reference
Ochroch EA, et al. Anesthesiology. 2002;97:1234-1244.
Multimodal Pain Therapy
Multimodal pain therapy decreases the chances of chronic pain.
Regional analgesic techniques can impact the pain experience for weeks to months following major surgery.
- Thoracotomy
- Prostatectomy

Pre-operative administration of gabapentin or pregabalin to help limit the development of central sensitization and:
- Lower postoperative pain intensity
- Lower the chances of developing chronic pain

Note: Gabapentin and pregabalin are not FDA approved for this purpose but are supported by strong clinical trial evidence. See Clarke, H et al. Anesthesia & Analgesia. 2012;115(2):428-442.
Postoperative Pain Predicts Chronic Post-Thoracotomy Pain (CPTP)
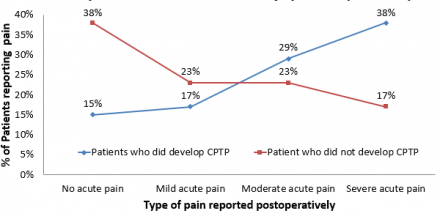
Reference
Pluijms WA, et al. Acta Anaesthesiologica Scandinavica. 2006;50:804-808.
Pain Therapy is the Responsibility of All Team Members

- Pre-operative screening and planning
- Pre-operative medication administration
- Pre-operative pain procedures
- Postoperative multimodal medication therapy
- Ongoing patient and family education
- Ongoing patient assessment
Pain Management Strategies
- Spinal opioids ± local anesthetics
- Epidural opioid and/or local anesthetics [Patient Controlled Epidural Analgesia (PCEA)]
- Intrathecal opioid administration
- Regional anesthetic techniques
- Systemic opioids
- Intravenous Patient- Controlled Analgesia (IV PCA or PCA)
- Non-opioid analgesics
- Acetaminophen and NSAIDs
- Adjuvant agents
- Gabapentin and pregabalin
Patient Controlled Epidural Anesthesia (PCEA): Basic Principles
- The catheter (of course) has to actually be where we want it for the technique to work
- Thoracic T6 – T9
- Upper Abdomen T7 – T10
- Lower Abdomen T9 – L1
- Hip / Knee L1 – L4
- Pain relief is better when both local anesthetics and opioids are used
- think before you use a local anesthetic alone
- Patients receiving PCEA do not always require an indwelling urinary catheter
Does Patient Controlled Epidural Anesthesia (PCEA) Improve Outcomes?

- Compared to systemic opioids, PCEA appears to lower risk of perioperative complications, thus possibly improving surgical outcomes
- PCEA may also have an impact on long-term survival following cancer surgery
Reference
Gottschalk A, et al. European Critical Care & Emergency Medicine. 2011;3:16-24.
Long-Term Survival and Epidural Analgesia

- Recent epidemiologic study evaluating survival in patients over age 66 who underwent colectomy for non-metastatic colorectal cancer
- 42,151 patients included in review
- There was a significant association between epidural use and improved survival (adjusted Cox model hazard ratio = 0.91, 95% CI 0.87-0.94)
Reference
Cummings KC, et al. Anesthesiology 2012;116:797-806.
Patient Controlled Epidural Analgesia: Medication-Related Adverse Events
- The risk of harm is real
- opioids can lead to sedation and respiratory depression / arrest
- the most common opioid used is fentanyl and it is important to know the concentration per ml, and dose per hour
- local Anesthetics can lead to hypotension and neurological dysfunction
- Don’t forget about the risk of epidural failure
Reference
American Society of Anesthesiologists Task Force on Neuraxial Opioids. Anesthesiology 2009;110:1–13.
Pain Following Major Thoracotomy (with PCEA)
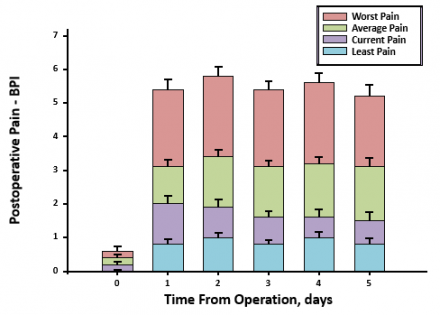
Reference
Ochroch EA, et al. Anesthesiology. 2002;97:1234-1244.

