Components of CPP History
- Pain history/diary: quality, location, timing with cycle, contributing or relieving factors, body map,
- Medical/surgical history including medications used presently and in the past
- Ob/Gyn:
- Menstrual history
- Sexual history
- Obstetrical history
- GI symptoms
- Urinary symptoms: interstitial cystitis screening (example: pelvic Pain and urinary frequency / urgency Patient Symptom Scale (Parsons, 2004)
- Musculoskeletal issues: injuries, falls, accidents
- Quality of life/coping
- Psychological health: depression, anxiety, PTSD, and physical and sexual trauma
- Health habits: substance abuse, nutrition/exercise
- Review records: diagnostic tests, treatments including surgical findings
See International Pelvic Pain Society Website for history and PE forms: English, Spanish, French.
Assess Quality of Life
Assess impact on functioning and quality of life (scale of 1 to 5)
In the past month, how much has your pelvic pain kept you from doing your usual activities such as self-care, work or recreation?
How much has your pelvic pain interfered with your quality of life?
How much have the treatments you have received for your pelvic pain improved your quality of life?
How do you cope with your pain?
How does your partner, family etc. respond when you are in pain?
Psychological Health
- Elicit patient’s view of illness, fears and concerns
- Do you have any thoughts or concerns about what might be causing the pain?
- Screen for current or prior physical or sexual violence, including events in childhood.
Screen for depression
- During the past month, have you been bothered by little interest or pleasure in doing things?
- During the past month, have you been bothered by feeling down or hopeless?
- Assess sexual functioning.
- Desire, frequency, satisfaction, orgasm and discomfort.
CPP Diagnostic Tests
|
TEST |
RATIONALE |
|
Urinalysis and culture |
Rule out urinary tract infection |
|
Wet mount, STI screening |
Rule out genital tract infection |
|
ALT and creatinine |
Screen for liver or kidney disease/multiple medications |
|
TSH, CBC, FBS, Vitamin D OH 25 |
Screen for depressive or constitutional symptoms |
|
Pelvic sonogram |
Biannual exam is limited or abnormal |
|
CT and MRI |
Prior diagnostic studies are abnormal or inadequate |
|
Laparoscopy |
Persistent symptoms, infertility, large ovarian cysts, treatment of endometriosis or adhesions |
|
Cystoscopy |
Concern for interstitial cystitis or other bladder conditions |
|
FOBT x 3 or referral for colonoscopy |
GI symptoms, bleeding, rule out colon cancer |
Reference
Adapted from: Abercrombie PD, Learman LA. Providing Holistic Care for Women with Chronic Pelvic Pain. J Obstet Gyncecol Neonatal Nurs. 2012 Aug 3.
Physical Exam Goals
- Identify underlying pathology
- Reproduce pain
- Establish trust and minimize fear
Directed Exam for CPP
- General musculoskeletal exam
- Abdominal exam including testing for Carnett’s Sign
- Assess for myofascial trigger points
- Q-tip test for vulvodynia
- Examine pelvic floor muscles using single digit vaginal exam
Carnett’s Sign
- Differentiates pain originating from the abdominal wall versus peritoneal cavity (Suleiman et al., 2001)
- The patient raises her head and shoulders from the examination table while the provider palpates the tender area on the abdomen.
- Positive Carnett’s sign: pain remains unchanged or increases when the abdominal muscles are tensed.
Myofascial Trigger Points
- Trigger points are hyperirritable palpable nodules that are taut bands of muscle fibers (Tough et al., 2007)
- When palpated the pain usually radiates to another location
- Found in abdominal wall, buttocks, hips, perineum and pelvic floor locations
- Major contributor to CPP
See also:
Lavelle ED, Lavelle W, Smith HS. Myofascial trigger points. Anesthesiology Clin. 2007 Dec;25(4):841-51, vii-iii. 25, 841-51. PMID: 18054148.
Directed Exam for CPP, Continued
- External genitalia: vulvar / vestibular lesions and tenderness (Q tip test)
- Urethra and bladder: mass or tenderness, prolapse
- Vagina, cervix:
- Inspection (lesion, trauma, infection, prolapse)
- Single digit vaginal exam
- Wet mount / STI screening if clinical suspicion
- Uterus, adnexae – bimanual
- Size, shape, consistency, mobility, mass, tenderness
- Rectal or rectovaginal
- Lesion, rectocele, uterine retroflexion, uterosacral nodules
Q-tip test for vulvodynia
- Purpose: identify and map changes in sensation including allodynia
- Gently touch with a Q-tip
- Start at the thigh and work down to perineum bilaterally
- Include clitoris and perianal areas
- Proceed from labia majora to labia minora then the vestibule
- Record findings: location of changes in sensation and severity
Reference
Hartmann D. Chronic vulvar pain from a physical therapy perspective. Dermatol Ther. 2010 Sep-Oct; 23(5):505-13. doi: 10.1111/j.1529-8019.2010.01353.x. PMID: 20868404
Test Your Knowledge: What is Allodynia?
Single Digit Vaginal Exam: Palpation of Pelvic Floor Muscles
Palpation may elicit: tension, spasm, tenderness and trigger points
- Layer one (First knuckle of first finger)
- Bulbocavernosus, ischiocavernosus, superfiscial transverse perineal and external anal sphincter muscle
- Layer two (second knuckle of first finger)
- Urethra muscles superiorly and deep transverse perineal muscles inferiorly
- Layer three (beyond second knuckle of first finger)
- Levator ani, coccygeous, piriformis and laterally obturator internus
Positive findings confirm a diagnosis of pelvic floor muscle dysfunction
Reference
Pastore EA, Katzman WB. al (2012). Recognizing Myofascial Pelvic Pain in the Female Patient with Chronic Pelvic Pain. J Obstet Gynecol Neonatal Nurs. Aug 3. doi: 10.1111/j.1552-6909.2012.01404.x. [Epub ahead of print] PMID: 22862153
Case Summary: Ms. Rhodes Physical Exam Findings
Affect: flat and anxious
Abdomen: diffuse pain throughout, positive Carnett’s sign suggestive of myofascial pain, no masses or organomegaly
Q-tip test of vulva: positive allodynia at the vestibule, exquisitely tender
Single digit vaginal exam: burning pain at introitus, tenderness and tightness of obturator internus, levator ani and piriformis muscles on exam. Anterior palpation of vagina replicates bladder pain. Posterior palpation reveals hard stool in rectum.
Patient states the exam reproduces her pain and she has acute exacerbation of pain after exam.
Common Diagnoses
- Gynecologic: endometriosis, vulvodynia
- Gastrointestinal: IBS
- Urinary tract: Interstitial cystitis
- Musculoskeletal/neurological: myofascial pain, pelvic floor muscle dysfunction
- Psychological: anxiety, depression, sexual dysfunction
The focus will be on issues managed by women’s health specialists
Endometriosis
Symptoms
- Severe dysmenorrhea
- Deep dyspareunia
- Chronic pelvic pain
- Ovulation pain
- Cyclical or premenstrual symptoms (bowel, bladder etc.) with or without abnormal bleeding
- Infertility
- Chronic fatigue
Physical Exam
- Pelvic tenderness
- Fixed retroverted uterus
- Tender utero-sacral ligaments
- Enlarged ovaries
- Deeply infiltrating nodules (best found during menses)
- Visible vaginal or cervical lesions
Diagnosis
- Ovarian suppression: OC’s, progestins
- Diagnostic laparoscopy (gold standard)
- Family history
- Cyclic pain
Treatment
- Ovarian suppression: OC’s, progestogens, danazol, GnRH agonists
- Surgery: Lysis of lesions and/or adhesions, remove endometriomas, LUNA/presacral neurectomy, Hysterectomy with BSO
- Anti-prostaglandins: NSAIDS
- Anti-inflammatory diet, herbs and supplements
Test Your Knowledge: Dyspareunia
What is dyspareunia?
Vulvodynia
Incidence
3-5% of reproductive age women
Risk Factors
- Vulvovaginal infection
- OC use
- Physical, emotional or sexual trauma
Comorbid disorders
- IC
- IBS
- Fibromyalgia / Chronic Fatigue Syndrome
- Psychosocial and sexual impairment
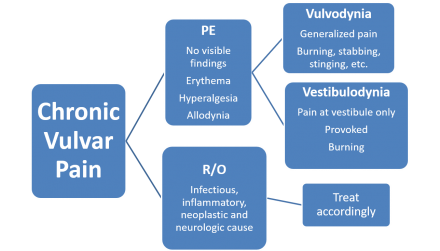
Diagnosis of Vulvodynia
Vulvodynia Treatments
- Multidisciplinary approach
- Patient education
- Topical agents: local anesthetic
- Oral pain medications: TCA’s, gabapentin, pregabalin
- Vestibulectomy
- Pelvic floor therapy, biofeedback
- Acupuncture
- Intralesional injections
- Supportive therapy: sexual, psychological
- Diet modification
Reference
Nunns D, Mandal D, Byrne M, McLelland J, Rani R, Cullimore J, Bansal D, Brackenbury F, Kirtschig G, Wier M; British Society for the Study of Vulval Disease (BSSVD) Guideline Group. Guidelines for the management of vulvodynia. Br J Dermatol. 2010 Jun;162(6):1180-5. doi: 10.1111/j.1365-2133.2010.09684.x. Epub 2010 Mar 16. PMID: 20331460
Myofascial Pain
Inciting Pain Event: may involve uterus, ovary, bowel, bladder, muscles and/or nerves
Subsequently:
- Inciting Event Resolves (naturally or with treatment)
- Local Muscle tension leading to secondary Muscle "Adaptations" (Lower back, buttocks, hips, pelvic floor) that cycles back to another inciting painful event

