DNIC: Diffuse Noxious Inhibitory Control
- A phenomenon where a strong pain suppresses the perception of another pain that is less intense
- E.g., a minor headache is less likely to enter conscious awareness when a hammer hits your thumb
- DNIC is present in about 30% of people
- Some people are pain-neutral, other experience enhancement of pain with other pains
- DNIC attenuates with age
Detailed Overview of Nociceptive Processing
Is your patient on opioids prior to surgery?
Expect to use more afterwards...
…and they won’t work as well, either.
Reference
Preoperative opioid consumption increases morphine requirement after leg amputation. Roullet S, Nouette-Gaulain K, Biais M, Bernard N, Bénard A, Revel P, Capdevila X, Sztark F. Can J Anaesth. 2009 Dec;56(12):908-13.
Early Pain Experience May Enhance Later Pain Signaling
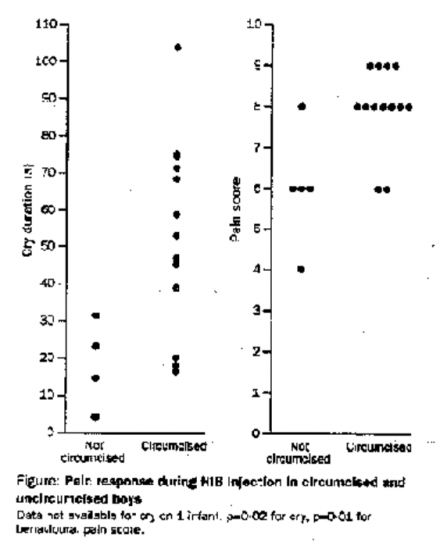
Reference
Effect of neonatal circumcision on pain response during subsequent routine vaccination. Taddio A, Katz J, Ilersich AL, Koren G. Lancet. 1997 Mar 1;349(9052):599-603
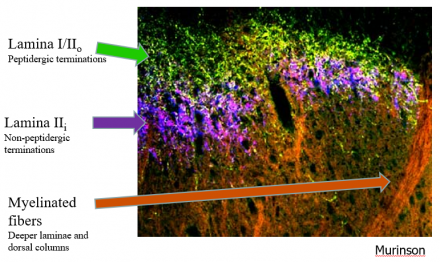
Wind Up
- A phenomenon in repetitive presentation of a stimulus results in increased pain perception
- Predominantly mediated by C- fibers
- Wind-up is relevant clinically when patients have small fiber neuropathy, dysfunction of small fibers makes them especially sensitive to repetitive stimuli, e.g. walking on gravel, hot sand, carpeting (chemotherapy induced neuropathy) and tight shoes.
Reference
Woolf CJ, Chong M-S. Anesth Analg 1993; 77:362-379.
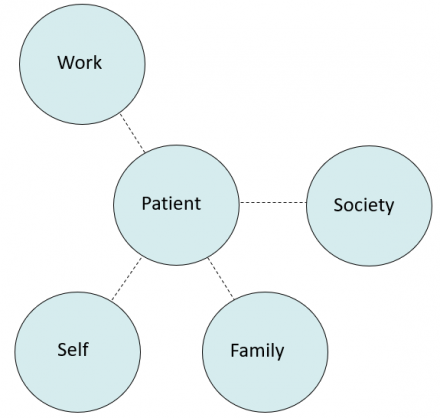
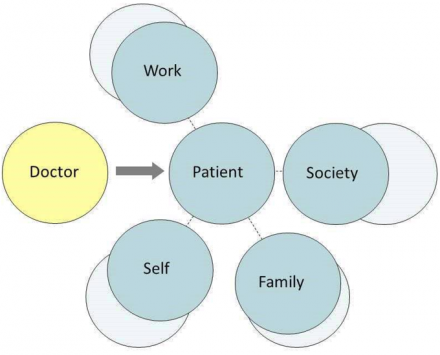
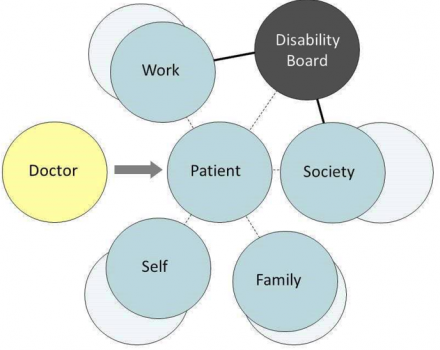
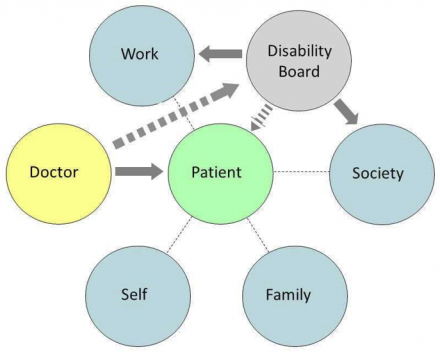
Pain and Function
Small group review material (please review before attending small groups).
1. Patient’s functional domains before illness. People normally function in several roles including work-role, self-care, participation in family unit and social functioning.
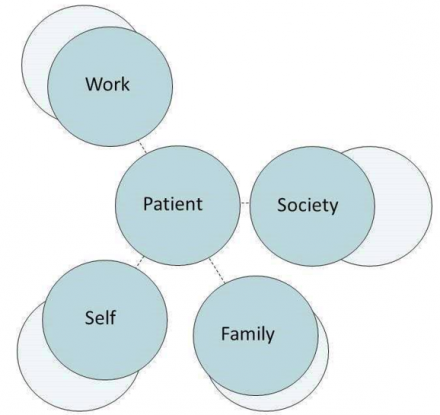
2. Patient's diminished function during illness. Function in various domains is diminished, note decreased distance in graph. Limitations (impairments) vary by domain.
3. Doctor - assesses patient. Physician incorporates history as well as physical exam and diagnostic test results. Evaluation should include assessment of function in various roles.
4. Disability board - reports to employer or government. Patient's sense of well-being is often strongly influenced by challenges and demands of the disability process.
5. Doctor works with disability board to okay work.
When an Employee is Unable to Work
When an employee becomes unable to work due to injury or illness, our expectation is that employee benefits and insurance will make up for lost wages due to time away from the job. Many patients will have sick leave that provides for a short work absence. Workers’ compensation provides benefits to employees with work-related injuries or illnesses. However, according to the National Safety Council, more than two thirds of disabling injuries happen off of the job [NSC]. Similarly, illnesses such as cancer, stroke and heart disease, may not eligible for worker’s compensation. Short-term and long-term disability insurance replaces income, usually at a rate of 50-70%, if a patient is unable to work due to non-occupational injury or illness. The Bureau of Labor and Statistics reported for 2009, that only 37% and 32% of civilian employees participate in short-term disability and long-term disability insurance programs, respectively [BLS].
Loss of Income
Therefore, the majority of patients with a non-occupational injury or illness resulting in large amounts of missed work face total loss of income.
Social Security Disability uses a stringent definition of disability in which only complete, long-term disability is considered. Disability must exist for a year before disability is determined.
Worker’s Compensation
Most state workers compensation agencies use a version of the ‘AMA Guides to the Evaluation of Permanent Impairment’ to define terms and assess the percentage of physical loss resulting from the illness or injury [College].
In the AMA guides 5th edition, an impairment is defined as “an alteration of an individual’s health status; a deviation from normal in a body part or organ system and its functioning [5th edition AMA guides].” For workers compensation, an impairment is directly weighted to the “normal”. Impairments are assigned ratings after reaching maximum medical improvement. The AMA guides 5th edition defines disability as “an alteration of an individual’s capacity to meet personal, social, or occupational demands because of an impairment [5th edition AMA guides].”
Social Security Administration
SSA definitions of impairment and disability are more stringent:
Medically Determinable Impairment – “a physical or mental impairment that results from anatomical, physiological, or psychological abnormalities which can be shown by medically acceptable clinical and laboratory diagnostic techniques. A physical or mental impairment must be established by medical evidence consisting of signs, symptoms, and laboratory findings-not only by the individual's statement of symptoms [SSA – 3].”
Disability – “the inability to engage in any substantial gainful activity (SGA) by reason of any medically determinable physical or mental impairment(s) which can be expected to result in death or which has lasted or can be expected to last for a continuous period of not less than 12 months [SSA – 3].” Under SSA guidelines, a medically determinable impairment requires observable signs and symptoms, not solely patient report of symptoms. The impairment must result in an inability to engage in work for at least one year.
Small Group Cases
The following material can be used by instructors for small group cases.
These are three cases of patients with pain. This discussion will be facilitated by
your group leaders. Your group leaders perspectives on impairment and disability will be colored by their specific disciplines: Psychiatry, Neurology, Anesthesiology, and Physical Medicine & Rehabilitation.
Case #1: Post‐Stroke Pain A
Mrs. S. is a 52 year‐old woman recovering from a mild hemorrhagic stroke suffered 4 months ago. Mrs. S. wishes to return to her full‐time child‐care provider position in a large center where she has worked for 9 years. For the 2 years prior to the stroke, Mrs. S. has cared for babies 3 months to 12 months of age in the infant care room, with a staff to child ratio of 1:3. In her time with the center, Mrs. S. has also worked as a provider and assistant teacher in both the 3 year‐old room and the 5‐year‐old room, but prefers working with the infants. Mrs. S. carries short‐term disability insurance and has been receiving her income at 50% for the past 3 months. Mrs. S. has been placed on a statin to control her cholesterol and advised to adopt a low‐fat, low‐cholesterol diet for both cholesterol and weight control. Although her ability to communicate and ambulate have been unaffected, the stroke has resulted in mild left‐sided weakness and left shoulder pain. One week after the stroke, Mrs. S. characterized her shoulder pain as a constant aching of an intensity of 5 out of 10, with additional bursts of sharp pain due to spasms having an intensity of 8 out of 10. Extensive physical therapy and use of prescribed exercises has resulted in improvements in left shoulder range‐of‐motion, strength and diminishment of pain. Mrs. S. describes her current pain as a constant left shoulder ache with an intensity of 3 out of 10, controlled with 25 mg amitripyline at bedtime, although at the time of the visit she notes a pain of 6 out of 10. Mrs. S. acknowledges that her shoulder is more painful when she increases her activity level or is fatigued.
Questions to Ask
What questions would you ask to determine this patient’s functioning in the areas of work, family, society and self? Examples are provided for this case, discuss what answers the patient is likely to provide to these questions.
Self
- Are there any activities from which you feel restricted at this point in your recovery due to pain or weakness?
- How is your energy level?
- How are you sleeping and eating?
- Are you taking your medications as prescribed?
- What are you doing for exercise, both prescribed arm exercises and in general?
- What are you doing for fun?
Family
- How supportive is your family at this point in your recovery?
- Have you been able to take over most the household tasks delegated to other family membersduri ng your recovery?
- Have any positive or negative changes in your family relationships resulted from your illness?
- Does your family have increased financial stress with your salary being reduced?
Society
- Have you felt connected to friends and your community during your recovery?
- How often do you interact with others on a weekly basis during errands, community activities, religious activities or recreational activities?
Work
- Are you motivated by a need to return to a full salary, or do you truly feel ready to tackle the challenge of returning to work?
- What job functions will be easy or difficult for you when you return to work?
- Do you miss the children you care for at work?
- Do you miss any of your coworkers?
The patient has requested you to fill out a release form for return‐to‐work in which return‐to-work restrictions, if any, are specified.
Decide what return‐to‐work restrictions you would place on this employee by considering the following list.
How often can the patient perform the following – never, seldom, occasional, frequent, constant or not restricted?
- sit, stand, walk, climb, twist, bend, kneel, crawl
- extremity control (left, right, both) – work above shoulders, keyboard, wrist flexion and
- extension, grasp, fine manipulation, operate foot controls, vibratory tasks
- lifting/pushing with arms (left, right, both) and back – number of pounds and duration
Mrs. S. has a strong desire to return to work with infants. Your impression is that her left arm weakness may impair her ability to safely carry out her job related tasks. How would you respond to this patient’s request to return to work in her original position?
Case #2: Painful Crushed Foot
Ms. B. is a 27 year‐old paralegal who suffered a left lower‐limb trauma 9 months ago. A car slid on ice in her law firm’s parking lot pinning her left foot against a parking space barrier and knocking her backward awkwardly, badly fracturing her left tibia. Ms. B.’s orthopedic trauma surgeon released her to return to work 6 months following the trauma, to allow for multiple surgeries and extensive physical rehabilitation. Her surgeon regards her orthopedic outcome as excellent overall, functionally and cosmetically. Ms. B.’s physical therapist ascribes the patient’s excellent functional recovery to her intense determination and overall excellent physical health. The physical therapist did note Ms. B.’s expectation to continue rock climbing and hiking in the future may be unrealistic
due to her neuropathic injuries and pain. Ms. B. is also under the care of a neurologist for
persistent neuropathic foot pain due to injury to her peroneal nerve . Her neurologist prescribed gabapentin and increased the dosage to 900 mg bid one month ago.
Ms. B. has returned to her primary care physician’s office with complaints of persistent left foot pain which has increased to a baseline intensity of 6/10 in severity with flares of breakthrough pain with an intensity of 9/10. The patient states that the pain has gotten progressively worse during the three months she has returned to work. She reports that the intensity of the pain makes her unable to maintain the concentration required to work full days and she is leaving the office earlier each day. Up till this point, Ms. B. has refused referrals for cognitive behavioral therapy or psychological support. Ms. B. also has resisted the use of opioids during the very painful physical rehabilitation. Ms. B.’s demeanor is sad and stressed. She has requested a medical excuse absence note for her employer and wants you to fill out long‐term disability forms because she can’t handle
the pain and stress of working.
Questions and Topics for Discussion
Before beginning the disability discussion with Ms. B., how could expressing empathy for her increased pain, empathy for the difficulty of her recovery and sincere admiration for her determination to return to functionality steer the office visit in a more positive direction?
What questions would you ask to more fully understand the change in pain intensity?
What would you ask the patient to find out the extent of accommodations her employer has in place for her?
Case #3: Sickle Cell Vaso‐Occlusive Crisis Resulting in Missed Final Exams
Mr. D. is a 18‐year old African‐American male pre‐med college student with a diagnosis of sickle cell disease (SCD), Hb genotype SS. The patient has come to Student Health Services to obtain a medical waiver to allow him to postpone taking final exams, which begin today for the university, until next week. His first exam is scheduled for Monday (today) at 11:00 am. The patient hands you medical records for an emergency room visit last Thursday for a severely painful vaso‐occlusive crisis which resulted in hospitalization. The patient received intravenous morphine using a PCApump.
His pain was sufficiently resolved to be released after 36 hours with a dihydrocodeine
prescription. The patient states that although his pain is well‐controlled at this time, he has been unable to study since the pain became unbearable last Wednesday. Mr. D believes that a waiver to begin taking exams next Monday will give him sufficient time to prepare. As you read over the medical report, you note that the patient was dehydrated on admission and also tested positive for cannabis.
What questions would you ask this patient about his pain and pain management to determine if a one‐week delay in final exams is reasonable?
Consider what difference the physical appearance of the patient would make in the believability of his pain crisis narrative.
- Mr. D. is neatly attired and arrives at the 9:00 am opening time of the clinic on Monday.
- Mr. D. is attired as if he is heading to the gym and arrived at 11:00 am on Monday.
Consider what difference the demeanor of the patient would make in the believability of his pain crisis narrative.
- Patient is upbeat and self‐assured about his eventual performance on his final exams.
- Patient is stressed and unhappy to be taking his exams late. He would prefer not to explain his medical situation to each professor and is worried that his make‐up exams might be increased in difficulty.
Mr. D. has never come to the student health services clinic during previous VOCs. He reports that since he lives off‐campus, he doesn’t want to come on campus in pain to get to the clinic after a pain crisis starts getting worse. Given the ER report that he was dehydrated and tested positive for cannabis, what types of questions would you ask about his self‐management of milder VOCs?
Reference
Zempsky WT. Treatment of sickle cell pain; fostering trust and justice. JAMA. 2009; 302(22):2479‐2480.
Neuropathic Pain: Clinical Correlation
Instructors can use this section to build out a patient-specific clinical correlation.
Our Patient
This section should include a presentation of a patient with acute pain. There should be a relevant link to the anatomy section which follows.
Neuropathic Pain Characteristics
Anatomy of Pain
This section should include information about the anatomical system signaling pain. Reference should be made to the case presented.
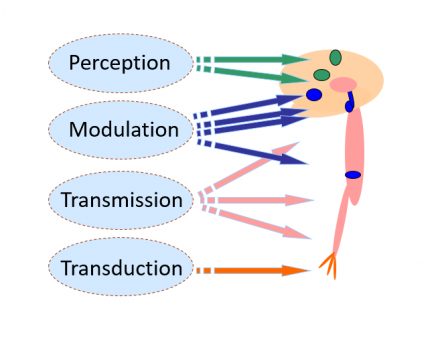
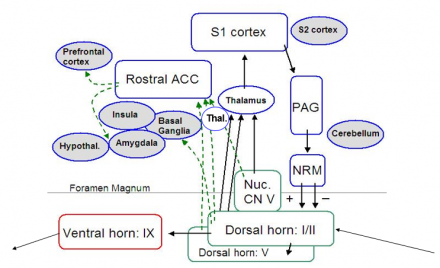
Modulation
- Both suppression and facilitation occur
- Modulation occurs at multiple levels
- Insula
- PAG
- Nucleus Raphe Magnocellularis
- Dorsal horn
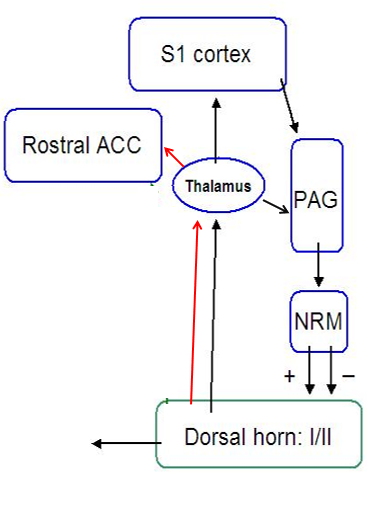
Spinal Dorsal Horn
Pain Treatment Plan Elements
This section should include information about pain treatment plan elements. Reference should be made to the case presented.
Pain Treatment Plans
4 components
- Goals for treatment
- Expectations
- Treatment modalities
- Time Course
1. Goals for treatment
S.M.A.R.T. I
- Specific
- Measurable
- Attainable
- Relevant
- Timely
S.M.A.R.T. II
- Specific
- Mutually agreeable
- Adaptable
- Realistic
- Time-bound
Patient + Provider = Success
2. Expectations for Treatment
Expectations for treatment vary depending on:
- Type of Pain
- Setting and context
- Patient needs
Expectations should be outlined explicitly and include the patient:
- Check for understanding
- Ensure shared-decision making
- Balancing pain relief and side effects
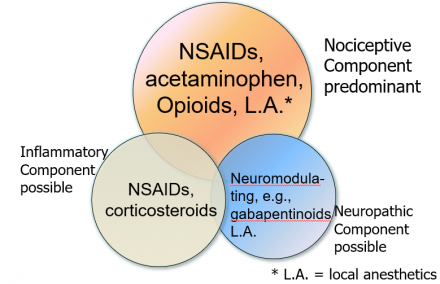
3. Treatment Modalities
Pharmacological
- NSAIDS and acetaminophen (OTC analgesics)
- Neuromodulating agents
- Anti-depressants
- Anti-convulsants
- Local anesthetics
- Others
- Opioids
- Non-pharmacological
- Psychological
- Manual (PT, massage)
- Activating (occupational)
- Complimentary and alternative
Mechanism-Based Classification of Pain
- Generally straight-forward to understand and apply
- Enhances understanding of relevant disease mechanisms
- Guides the choice of pharmacological treatments
- Determines the extent and type of non-pharmacological treatments
- Anticipates the time course and degree of disability associated with pain
Mechanism-Based Classification of Pain: Management of Acute Pain
4. Time Course
- Reflects realities of underlying disease:
- Make sure to supply analgesia for the anticipated duration of acute pain: once analgesia wears off, your patient may have a sharp increase in pain!
- Influenced by individual factors
- Personal history of pain, other conditions, psychological and social state
- Includes a plan for re-assessment
- Don’t assume therapy is effective, check for pain relief
- Treatment end
- If opioids are prescribed for more than 3 days, make sure to structure a sound tapering plan to avoid withdrawal symptoms
Recognizing Acute Pain in Patients with Chronic Pain
This section should include information about assessment of pain. Reference should be made to the case presented.
Questions for Review
- What distinguishes neuropathic pain from nociceptive and inflammatory pain?
- What features of a patient’s description of pain can tip you off to a neuropathic pain element?
- Where is the pain generator or generators for this patient?
- How effective was the first treatment for this patient?
- What steps would you take to further optimize this patient’s pain management?
- Are there medications or treatments that you would not use in this patient?
Questions for the study of neuromodulating agents in the treatment of neuropathic pain.
What are the characteristic qualities of neuropathic pain, e.g., burning?
- Burning, zinging (electric-shock like), tingling, painful numbness, cold
What are some common neuropathic pain conditions (name 5)?
- Shingles, post-herpetic neuralgia, diabetic neuropathy, sciatica, lumbar and cervical radiculopathy, carpal tunnel syndrome, ulnar neuropathy, HIV neuropathy.
What are the classes of drugs are used to treat neuropathic pain (name 3)?
- Pain-active anti-convulsants, pain-active anti-depressants, opioids, local anesthetics, botulinum toxin.
What mechanistic features distinguish the pain-active anti-depressants?
- SNRI mechanism
What are the major mechanistic features of the drugs originally classified as anti-convulsants but used in the treatment of neuropathic pain?
- Gabapentin and pregabalin act at pre-synaptic calcium channels to decrease the influx of calcium into pre-synaptic nerve terminals and decrease nociceptive signaling.
Regarding the use of anticonvulsants for the treatment of neuropathic pain:
Name 4 anti-convulsants used to treat neuropathic pain
- Gabapentin, pregabalin, carbamazepine, lamotrigine
What are the major side effects of each agent?
- Gabapentin – dizziness, fatigue
- Pregabalin – dizziness, fatigue, mental clouding, ankle swelling
- Carbamazepine – hyponatremia, bone marrow suppression, hepatic effects
- Lamotrigine – life threatening rash (Stevens Johnson syndrome possible)
What are the major indications for each agent? (i.e. what diseases is each drug used for?)
- Gabapentin, pregabalin: neuropathic pain
- Carbamazepine: trigeminal neuralgia
- Lamotrigine: HIV neuropathy
Which agents are typified by few drug interactions?
- Gabapentin
Can the drugs be used prn (as needed) or do treatment plans require daily dosing?
- Daily dosing is require for these agents.
Regarding the use of anti-depressants for the treatment of neuropathic pain:
Name 4 anti-depressants used to treat neuropathic pain.
- Duloxetine, venlafaxine, amitriptyline, desipramine, nortriptyline.
What are the major side effects of each agent?
- Suicidal ideation is possible with all of these agents and the risk of suicide is real. Patients should be warned to stop the medication immediately and seek medical attention if this happens. It occurs unpredictably.
- Amitriptyline causes profound sedation and should be taken only at bedtime. No driving afterwards. Dry mouth and other autonomic effects are present.
- Nortriptyline can cause urinary delay, it is metabolized into amitriptyline and can cause mild sedation..
- Desipramine is not sedating but can cause tachycardia, patients should be warned to stop the medication is this occurs
- Duloxetine can cause dizziness and been noted to increase liver enzymes, packageinformation should be consulted for all of these medications
- Venlafaxine can cause dizziness, nausea and headaches among other symptoms. Patients can experience serotonin syndrome with abrupt discontinuation.
What are the major indications for each agent? (i.e. what diseases is each drug used for?)
- All of these agents have been used for chronic and neuropathic pain. Only duloxetine has secured FDA approval for pain indications: fibromyalgia, diabetic peripheral neuropathy and chronic musculoskeletal pain. Remember that the NNT of this medication is 5-6 meaning 5 people will need to receive the drug for 1 person to obtain benefit equivalent to the clinical trial primary outcome measure, e.g. 30% pain relief. These drugs do not work for everyone and this is why so many options are needed and why we still use drugs that are ‘off-label’ meaning they do not have FDA approval for a specific condition
Which agents are typified by few drug interactions?
- All of these drugs have drug-drug interactions, you should run a Micromedex profile when adding to a patient’s regimen. It is especially true that when we treat neuropathic pain, we try not to mix drugs from the same class. These drugs should never be used with MAO inhibitors.
Can the drugs be used prn (as needed) or do treatment plans require daily dosing?
- Daily dosing is required. They do not work as prn drugs. Most of these medications require 1-2 weeks to achieve their effect.
Case 1 –New-Onset T11 Burning Pain
Mrs. A. presents to her primary care physician with new-onset, right-sided burning pain, constant in duration. Mrs. A. is a 63-year old woman recovering from a recent bout of right-sided thoracic shingles.
About four weeks ago, shingles began as a right-sided tingling sensation at the T11 dermatome with a day of nausea, vomiting and fatigue. Two days later, Mrs. A. presented to her primary care physician when she developed right-sided sharp stabbing pain and an elongated rash extending from her midline to back in the T11 region. She was prescribed an oral antiviral agent three times a day for 7 days. Oral prednisone was not prescribed since corticosteroids were contraindicated by both diabetes and hypertension. Mrs. A. rated the intensity of the stabbing pain as 8 out of 10 and was prescribed oxycodone for pain relief.
When Mrs. A returned for follow-up two weeks later, her lesions were in the process of crusting over and her pain had greatly subsided however, she complained of continued itching, fatigue, and nausea. Mrs. A.’s appetite was greatly decreased due to continued nausea and she was provided a referral to her endocrinologist due to difficulty regulating her blood sugar.
At today’s visit, Mrs. A.’s rash has cleared, however in addition to the new-onset burning pain, she complains of insomnia due to her persistent pain. Mrs. A. is nonfebrile, with a blood pressure of 125/80 and a resting pulse of 75. Her past medical history is significant for diabetes type 2 and high blood pressure, both diagnosed in 1995. Mrs. A. has had 5 five office visits since 2000 for pain due to gallstones. Her appendix was removed in 1982. Mrs. A. takes an ACE inhibitor for her high blood pressure and long acting insulin at bedtime and short acting insulin at meal times. Mrs. A. is married, has two grown children and reports no use of alcohol or tobacco.
Possible diagnoses include diabetic truncal neuropathy, postherpetic neuralgia, thoracic radiculopathy due to vertebral compression fracture, neuropathy due to another compressive lesion and visceral pain, possibly cholecystitis.
Diabetic truncal neuropathy presents with pain and dysesthesias in a dermatomal pattern involving one or more dermatomes. Allodynia to the touch of clothing or bedsheets is common. Patients may have no neuropathic pain diagnoses prior to presentation. Motor nerve involvement leads to weakening of the abdominal musculature and an abdominal bulge similar to a hernia may be observed.
Postherpetic neuralgia following shingles presents with pain, dysesthesias and allodynia to clothing or bed sheets. However, pain is localized a single dermatome and motor nerve involvement is not typical.
What else would you like to know from the patient?
What is the diabetes control like: are her morning blood sugars below 130? Has she had a hemoglobin A1C checked recently? Has she had any trouble breathing, has she had a change in bowel or bladder habits. Have there been any falls, or other trauma? Has the pain had a colicky pattern or changed with the consumption of various foods?
What other exam findings will you be looking for?
It is a good idea to see if there is evidence of peripheral neuropathy, e.g. decreased ankle reflexes, hyperalgesia to sharp testing or decreased sensation. It is a good idea to listen to the lunges as thoracic pain can result in significant respiratory splinting, atelectasis and eventually pneumonia. A brief abdominal exam would be appropriate as the patient has been treated with opioids and it is important to ask about constipation and confirm normal abdominal exam findings.
What diagnostic testing would you like to perform?
Depending on the index of suspicion, you might consider a blood count. Certainly it is reasonable to obtain serum glucose to see if blood sugars are elevated as they can be with the stress associated with the painful illness that this patient is clearly experiencing: poor sleep, elevated pain levels.
What do you want to know about her daily life?
What is she doing with her diet? How is she managing with the pain?
What are the management options you’d like to implement?
What medications would you want to implement for this patient, please name your first, second and third choices? What doses would you start with and what dosing regimen would you recommend for each?
For example:
Gabapentin, 300 mg at bedtime for 3 days increasing to 300 mg three times daily. This drug is good because it has few drug-drug interactions and can be titrated as high as 2400 mg daily in a patient with intact renal function.
Duloxetine, 30 mg in the morning times 7 days then 60 mg in the morning. This drug is good because it has relatively mild side effects, nonetheless some patients may not tolerate it and it will not provide a clinically significant benefit for many patients.
Amitriptyline, 10 mg at bedtime. This drug is good because it can help with nighttime pain, patients will often have more severe pain when sleep is disrupted and pain itself will interfere with sleep. This drug needs to be used with some care. There is a recommendation that patients over 40 undergo a screening EKG, but a more balanced recommendation is that patients over 50 need a screening EKG, and the drug should be avoided in those with a cardiac history. It is contraindicated in the post-MI period. It has a high rate of efficacy and has been widely used for neuropathic pain. It is inexpensive.
Lidocaine patches, apply one for 12 hours daily. This drug is good because it has relatively few systemic effects. Unfortunately, many insurance companies will not approve this treatment and the patches are quite expensive.
What approaches would you counsel this patient to take?
Stay busy but try to get plenty of rest. Schedule pleasurable activities. Consider a 20 minute walk each day if this does not make the pain worse. Make sure to take your medicine on time, don’t wait until the pain gets bad. Keep a pain calendar so that you can track your symptoms and make sure to bring this to clinic at the next visit. This will help us plan the next treatment steps. Call the clinic if any problems arise with the medication or if the pain gets worse.
Case 2 – Bilateral Burning Foot Pain
Mr. S., a 63-year old male, presents to the neurology department with increased bilateral foot pain. Mr. S. describes a painful burning sensation in both feet which has increased over the past two weeks. The pain is not localized to a specific region of either foot, although the soles of the feet are more painful than the dorsal surfaces. He rates the severity of the pain as 5 of 10 and reports that it interferes with walking. Mr. S. states that the pain is constant, is not diminished by ibuprofen or acetaminophen and is minimally better on days when he is not as active. Additionally, Mr. S. reports that the pain wakes him up at night, interfering with restorative sleep, resulting in constant tiredness. Mr. S. reported bilateral intermittent paresthesias in his feet during an annual checkup 13 months ago. The symptoms spontaneously diminished and test results revealed no evidence of diabetes. Mr. S. likens the present burning quality of the pain as similar to that of the pain he felt as the result of a herniated disc at the L5-S1 level 15 years ago.
Mr. S. experienced an acute-onset herniated disc at the age of 50 which resulted in left-sided radicular pain in a S1 distribution. The episode presented as nagging and aching low back pain but progressed to leg pain and numbness with some leg weakness. He described the pain at its worst as a deep burning, radiating from the left buttock to the posterolateral thigh to the lateral foot. The pain was aggravated by standing or coughing. After attempts at conservative management did not bring expedient results, Mr. S. underwent a successful microdiscectomy and has been pain free until recently.
At the time of his microdiscectomy, Mr. S. quit smoking and has been in overall good health. After quitting smoking, Mr. S. was able to control his prehypertension with exercise and diet. Mr. S.’s only significant family history is a father who died suddenly of a M.I. at age 70. His father was obese and assumed to have hypertension although he refused medical check-ups. Mr. S. is retired and until recently spent his time playing golf and tennis and as well as boating. Mr. S. and his wife have an active social life, spending most evenings at their social club or at charity events. Mr. S. describes himself as a social drinker, having in the range of 3 to 10 alcoholic beverages daily.
Mr. S. is recommending that his doctors order some imaging as he suspects the occurrence of another disc problem. In addition, he is requesting oxycodone for pain relief.
What else would you like to know from the patient?
Have you ever felt you should cut down on your drinking? Have people annoyed you by criticizing your drinking? Have you ever felt bad or guilty about your drinking? Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover?
Have you had your blood sugar checked recently, have you ever been tested for diabetes, e.g. had a glucose tolerance test; have you had any other symptoms beyond burning feet and tiredness like profound fatigue or weakness? Is there anything that makes the pain better or worse?
What other exam findings will you be looking for?
You will want to examine for sensation, motor function and reflexes. A pattern of distal sensory changes (with or without) distal weakness and distal reflex lost (ankles: 0, knees: present) is consistent with peripheral neuropathy. Alcohol can very much produce a problematic neuropathy, it is unlikely that this patient has a malnutrition associated neuropathy (B12, B1, B6, etc.) but it is also true that many of the patients with new onset neuropathy have impaired glucose tolerance (does not show up as frank diabetes but does result in persistent elevations in blood sugar) that can produce a syndrome of painful burning feet.
What diagnostic testing would you like to perform?
If your exam confirms neuropathy, you will want to check a chemistry panel to look for hyperglycemia, renal dysfunction, hepatic dysfunction and thyroid dysfunction. All of these have been associated with neuropathy. Other causes include Lyme disease, syphilis, monoclonal gammopathy , B12 deficiency and hypersupplementation with vitamin B6.
What do you want to know about her daily life?
Is it important to explore alcohol and diet further? Absolutely.
What things alleviate the pain? There is usually little a patient can do to alleviate neuropathic pain, in some cases, people try immersing the feet in cold water or an ice bath. Some patients find that wearing sandals helps with pain, it seems that for many patients with neuropathy, mild cooling helps to quiet the nociceptors which become spontaneously active at 37 degrees centigrade as part of the disease.
What are the management options you’d like to implement?
What will you do if the patient demands an MRI? Use motivational interviewing to discover why they believe it is needed. It is completely not necessary for the evaluation of small fiber neuropathy. However, if a patient has a suspected radiculopathy, MRI of the spine can be helpful. Sometimes patients actually develop pain after a minor stroke, but this is almost always a unilateral pain syndrome, rather than effecting both feet.
Do you know enough at this stage to begin treatment? If so, what medications would you want to implement for this patient, please name your first, second and third choices? What doses would you start with and what dosing regimen would you recommend for each?
If your exam confirms the presence of neuropathy, you can start treatment as you wait for the bloodwork and other diagnostic tests to return. You can use the same medications as for the previous case. (This is why we teach about neuropathic pain and neuromodulating agents the way we do…. The treatments for neuropathic pain are often the same.)
What approaches would you counsel this patient to take?
Cut back on alcohol. It is a nerve poison. Make sure to keep the diet in balance. It is important to check you feet daily, people with neuropathy can injure the feet and it will be very slow to heal. It is known that 10% of people over 65 and 25% of people over 75 will have neuropathy. This is a silent epidemic. You may find it helpful to join a support group or to obtain treatment from a clinical psychologist to help cope with the pain. Physical therapy may be helpful as many people with this condition have worsened balance and are at risk for falls.

