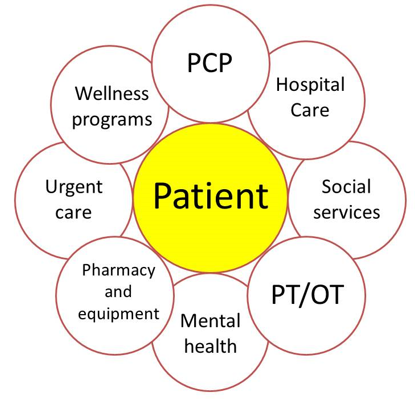
Patient is at the Center
Patient is at the center of an comprehensive and integrated healthcare delivery system
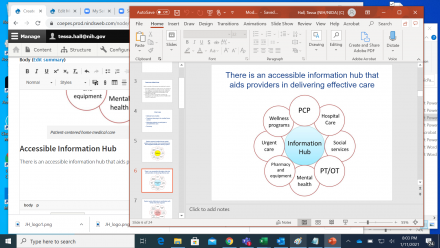
Accessible Information Hub
There is an accessible information hub that aids providers in delivering effective care
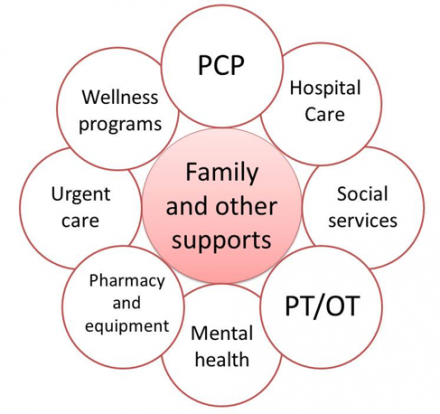
Coordination with Family and Other Supports
System works effectively in coordination with family and other supports.
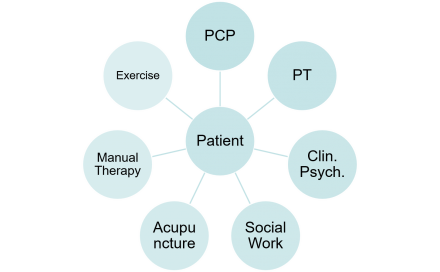
Patient is Always at the Center

Primary Care Provider
The primary care provider outlines and follows up on comprehensive care plan.
Benefits of Comprehensive Care
- Less sedation and cognitive impairment
- Improved long-term health
- Fewer adverse effects of medication
- Less reliance on opioids
- Higher patient satisfaction
- Higher levels of good functional outcomes
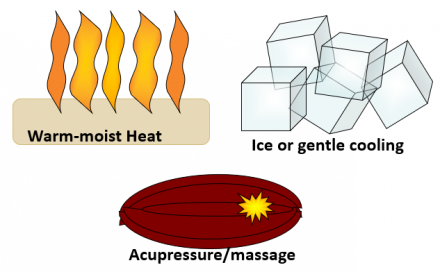
Pain Treatments
Pain treatments: active utilization of specific non-pharmacological therapies as appropriate.
Patients Should Take an Active Role
Encourage patients to take an active role in pain management: document and follow up on recommendations.
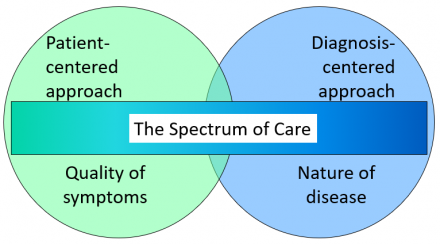
The Spectrum of Care
Treatments for pain vary with the situation: Sometimes dominated by the patient’s symptoms and sometimes by the specific diagnosis.
Mechanism-Based Classification of Pain
| Mechanism | Nociceptive | Inflammatory | Neuropathic |
|---|---|---|---|
| Non-pharmacologic treatments |
Ice and cooling Distraction |
Cooling Warming Moderate exercise |
CBT Pacing Orthotics Pleasant activities |
| Pharmacologic choices for mild-moderate pain | Standard anagelsics | NSAIDs | Neuromodulating |
| Pharmacologic choices for moderate-severe pain | Opioids, local anesthetics, nerve blocks |
Disease modifying Opioids |
Multi-drug regimens Opioids |
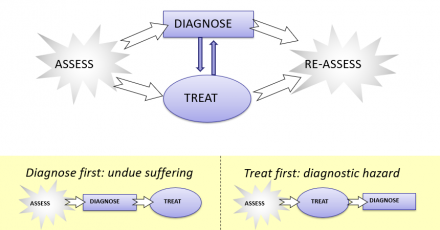
Parallel Path Model of Pain Intervention
‘Parallel path’ model of pain intervention: diagnosis and treat in parallel.
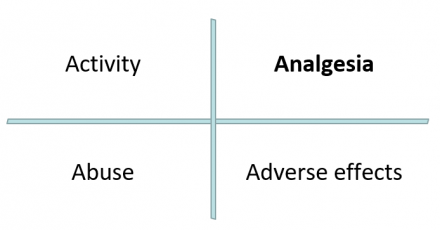
The Four ‘A’s of Follow-Up
For the patient with chronic pain, it is very important to balance analgesia with other goals of treatment.
Chronic and Persistent Pain
Motivational interviewing for Behavior Change
- Readiness for change
- stages of change model
- tailoring actions to stage of change
- Commitment
- ascertain values, talk values
- Confidence
- foster confidence, talk small steps
- Strategies for difficult moments
- Express empathy
- Develop discrepancy
- Roll with resistance
- Support self-efficacy
Stages of Change Model
Enduring value
| Stage in Model | Patient Characteristics | Other Models |
| Pre-contemplation |
Not considering change Resignation (no control) Denial (not relevant) Concern - low |
'locus of control' 'health beliefs' Motivational interview |
| Contemplation | Weighing benefits/costs | Motivational interview |
| Preparation | Experimenting with change |
CBT Motivational interview |
| Action | Taking steps to change | 12-step |
| Maintenance | Maintaining behavior | 12-step |
| Relapse |
Normal part of process Feels demoralization |
Motivational interview |
Core of Motivational Interviewing
Assess readiness to change.
- Pre-contemplative
- Contemplative
- Preparation
- Action
- Maintenance
- Relapse
Provide support and counsel that is stage appropriate.
If pre-contemplative
- talk about what patient values to discover what’s important to them
- frame the risks and benefits of potential change in terms of the values expressed by the patient
If contemplative
- Ask about the commitment to change
- Ask about their confidence to change
- Use information about patients values to boost commitment
- emphasize negatives that are most worrisome
- emphasize benefits that are most valuable
- e.g. teens typically worry about white teeth, middle-aged adults worry more about cancer
- Use brainstorming to find small steps would boost confidence
- Ask about what ideas the patient has or has tried
- Propose some small steps that you think might work well
- Make sure to check back on progress
If in preparation stage:
- Provide support with specific therapies, e.g. PT, CBT
- Provide ideas for substantive positive changes
- (e.g. a new program of moderate exercise)
- Continue to support motivation: commitment, confidence
- Use affirmation and encouragement
If in action stage:
- Ask about how the change is going
- Support the patient by addressing side effects, problems
- Suggest ways to avoid challenging situations
- (e.g. ask for help with lifting heavy objects)
If in maintenance stage:
- Ask about the behavior briefly
- Determine if challenges are present and aid if possible.
If in relapse:
- Express empathy- ‘Change is difficult but it is really important that you’ve already started’
- Develop discrepancy – ‘How is this different from your goals?’ ‘Is this what you really want?’
- Roll with resistance – stop pushing and reflect on patient’s standpoint (‘It sounds like this is really difficult’)
- Support self-efficacy - Encourage the patient to take up change once more, e.g. ‘I really believe you can…’
Reference
Miller WR, Rollnick S. Motivational interviewing: preparing people for change (2nd ed.) Guilford Press, 2002.
Summary
- The patient-centered medical home model is well-suited to providing comprehensive care to patients with pain.
- Physicians have a very important role in caring for patients with pain in the context of the medical home model: anticipating pharmacological and non-pharmacological treatment needs, adapting treatment to respond to patient and diagnosis, and employing an parallel pathway approach to commence pain-relieving treatments while diagnostic testing is underway are essential components.
- Motivational interviewing is an valuable skill for physicians to develop in order to promote positive changes in patient behaviors in the context of a chronic illness model.

