The Experience of Pain
- Places emphasis on the patient (patient-centered) and focuses on the development of a multi-modal, comprehensive care plan
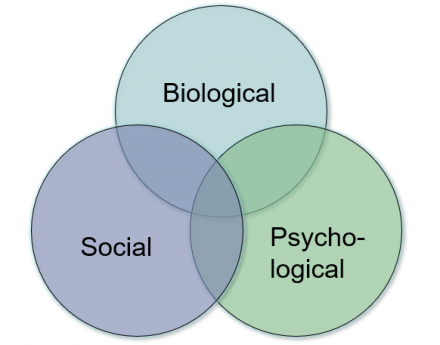
- Generalized biopsychosocial model incorporates
- Biological
- Psychological
- Social factors
- Pain-specific biopsychosocial model
- Nociception-Pain-Suffering-Pain Behavior
Generalized Biopsychosocial Model
Image
Pain Specific ‘Biopsychosocial’ Model (Loeser Model)
Image
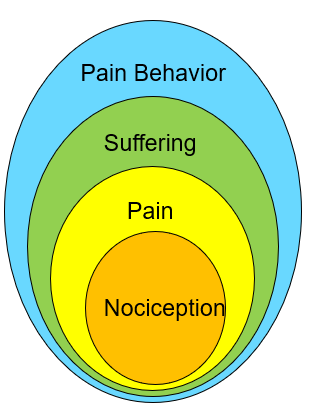
Interpretation: a specific nociceptive event may result in a range of responses including: pain, suffering and pain behavior, depending on the context in which nociception occurs.
Application of the Biopsychosocial Model in Pain Care
The biopsychosocial model is used in develop more effective plans for pain care with goals that include:
- Decreased pain
- Increased physical activity
- Improved sleep
- Lower stress levels
- Patient specific personal goals
Pain Treatment Plans: 4 Components
- Goals for treatment
- Expectations
- Treatment modalities
- Time Course
1. Goals for Treatment
S.M.A.R.T. I
- Specific
- Measurable
- Attainable
- Relevant
- Timely
S.M.A.R.T. II
- Specific
- Mutually agreeable
- Adaptable
- Realistic
- Time-bound
Patient + Provider = Success
2. Expectations for Treatment
Expectations for treatment vary depending on:
- Type of Pain
- Setting and context
- Patient needs
Expectations should be outlined explicitly and include the patient:
- Check for understanding
- Ensure shared-decision making
- Balancing pain relief and side effects
3. Treatment Modalities
Pharmacological
- NSAIDS and acetaminophen (OTC analgesics)
- Neuromodulating agents
- Anti-depressants
- Anti-convulsants
- Local anesthetics
- Others
- Opioids
Non-pharmacological
- Psychological
- Manual (PT, massage)
- Activating (occupational)
- Complimentary and alternative
4. Time Course
- Reflects realities of underlying disease
- what is the natural history of pain for this condition
- Influenced by individual factors
- personal history of pain, other conditions, psychological and social state
- Includes a plan for re-assessment
- cannot assume first pain therapy is effective, need to check for pain relief
- Treatment end
- even good treatments must come to an end some day
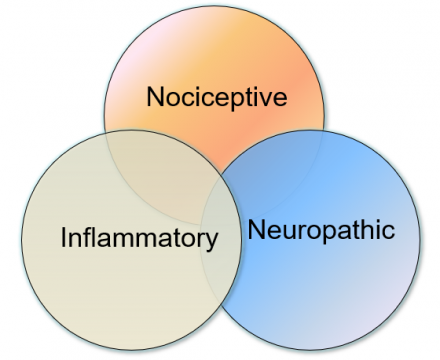
Mechanism-Based Classification of Pain
- Generally straight-forward to understand and apply
- Enhances understanding of relevant disease mechanisms
- Guides the choice of pharmacological treatments
- Determines the extent and type of non-pharmacological treatments
- Anticipates the time course and degree of disability associated with pain
Image
Nociceptive Pain
- Commonly signals tissue injury
- Sprains, strains, contusions, lacerations
- Iatrogentically induce pain
- Surgeries
- Procedures
- Dressing changes
- Ranges from mild and transient to severe and persistent depending on the cause and context of the pain
- Generally responsive to NSAIDs and/or acetaminophen when mild-to-moderate and transient
- May require opioids when more severe
Inflammatory Pain
- Generally reflects release and/or production of inflammatory mediators in the periphery, e.g.
- Joints
- Tendons
- Muscles and other tissues
- May range from mild to severe and may impair function
- May response to NSAIDs when mild-to-moderate
- Side effects, some serious, may limit utility of NSAIDs in treatment planning
- May require disease-modifying therapies when more severe, including: surgery, e.g. joint replacement, or immunomodulation
Neuropathic Pain
- Results from disease or dysfunction of nervous system
- Peripheral causes include neuropathy, root compression
- Central causes include MS, spinal cord compression, stroke syndromes, myelopathy
- Ranges from bothersome to severe and persistent although typically associated with affective component that makes suffering especially prominent in these patients
- Generally NOT responsive to NSAIDs or acetaminophen
- May require neuromodulating agents when persistent and opioids when severe
Mechanism Based Classification of Pain
- Useful in terms of understanding potential mechanisms of pain-associated conditions and in treatment planning.
- Specific conditions may involve one or more of these mechanisms and these mechanisms may be involved dynamically over the course of an illness, e.g., pain immediately after an ankle sprain is nociceptive, pain later on after the sprain may have a significant inflammatory component.
- The presence of one of these mechanisms may amplify pain arising from another.
Questions for Review
- What are the elements of the generalized biopsychosocial model of illness? How is this reflected in the pain-specific biopsychosocial model of Loeser?
- What are the components of an individualized pain treatment pain (name all 4)?
- What ideas will you use to guide you in establishing goals for treatment?
- Apply a mechanism-based classification of pain to sketch out a treatment plan for someone with a severely painful ingrown toenail. What mechanisms do you think are involved? What mix of pharmacological and non-pharmacological treatment options will you choose?

