Deciding on Treatment, Part 1
Following the physical examination, Mike discusses with Sarah his findings of myofascial pain and fibromyalgia.
Now that we have completed the history and physical examination. Mike explains to Sarah, what he thinks is causing her symptoms and what he recommends for treatment.
Is Sarah's expectation to be pain free appropriate?
Deciding on Treatment, Part 2
Mike discusses with Sarah a treatment plan to improve her functionality and activity while counteracting fatigue.
Pain Processing in Fibromyalgia
Two main neuropathways are involved in pain processing. The ACE sending pain pathway and the descending pain pathway. The ACE ending pain pathway starts with peripheral nerves called nociceptors, which are nerves activated by painful stimuli.
Nociceptors transmit pain sensations from the body to the brain for processing. Nociceptors transmit pain signals by releasing chemicals, such as substance P glutamate and nerve growth factor and other neurochemicals that mediate pain, descending pain pathways run from the brain to the spinal cord and inhibit pain signals.
This descending pain pathway is modulating by chemicals, such as norepinephrine, serotonin, and GABA. Studies suggest that there is an imbalance in the two pain pathways in [00:01:00] fibromyalgia patients research suggests that there is increased activity in the ascending pain pathway and decreased activity in the descending pain pathway.
This is compared to the pain volume being turned up.
Ascending Pathway
- Facilitates pain transmission
- Uses substance P, CGRP, nerve growth factor and glutamate
Descending Pathway
- Inhibits pain transmission
- Uses norepinephrine, serotonin and GABA
Fibromyalgia = increased activity ascending pathway and decreased descending pathway.
Brain Activity
Research also shows that brain activity in response to experimental pain is heightened in fibromyalgia patients compared to healthy adults. In this diagram, the pink areas show increased brain activity and response to the experimental pain in fibromyalgia patients compared to those without fibromyalgia.
Some of these areas such as the insula and anterior cingulate cortex are involved in the emotional processing of pain. This brain activity is believed to account for the increased pain sensitivity seen in fibromyalgia patients.
Pain Processing in Fibromyalgia
In one study, fibromyalgia subjects and control subjects were exposed to a pressure stimuli and reported their pain intensity. The fibromyalgia subjects represented reported a significantly higher pain intensity after exposure to a pressure stimulus compared to the control group represented by the blue square.
In fact, a 73% stronger stimulus was needed for the control group to report a similar pain intensity as the fibromyalgia subjects.
Reference
Gracely RH, Petzke F, Wolf JM, Clauw DJ. Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum. 2002;46(5):1333-43.
Higher CSF Substance P Levels in FMS
Numerous studies show higher levels of substance P in the cerebral spinal fluid of fibromyalgia patients and other patients with chronic pain conditions. Substance P is a neuropeptide that is fundamental to pain processing. Some suggest that these higher levels of substance P play a role in the abnormal pain processing seen in the fibromyalgia syndrome.
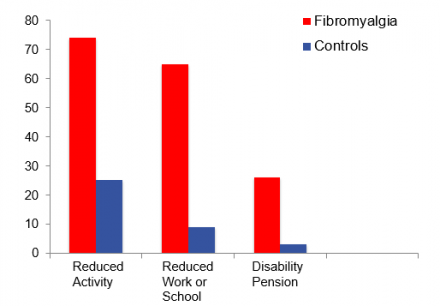
- Serotonin levels are lower in fibromyalgia subjects compared to controls
- Central serotonin plays a role in blocking pain signals
As this graph shows lower levels of serotonin are found in the cerebral spinal fluid of fibromyalgia patients compared to control subjects. Serotonin is an important neurotransmitter involved with the descending pathways that block pain transmission from the periphery. Some suggests that lower central serotonin contributes to the heightened pain levels seen in fibromyalgia patients.
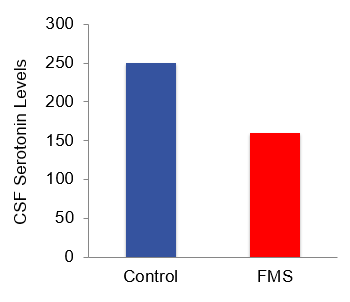
Antidepressant medications increase central serotonin and are often helpful for treating fibromyalgia pain.
Reference
Russell IJ. Neurotransmitters, cytokines, hormones and the immune system in chronic non-neuropathic pain. In: Wallace DJ, Clauw DJ, editors. Fibromyalgia and Other Center Pain Syndromes, Philadelphia, PA: Lippincott, Williams & Wilkins; 2005. p.63-80.
Myofascial Pain versus Fibromyalgia
It is also important to recognize the difference between myofascial trigger points and fibromyalgia tender points. Practitioners may use these terms interchangeably, but there are differences between the two, as we can see from Sarah's case patients with localized myofascial pain, like Sarah's neck pain may also have generalized pain associated with fibromyalgia syndrome.
Trigger points are associated with myofascial pain. And often have taught bands or nodules within the muscle belly, which are palpable on examination. allodynia, hyperalgesia and pain are found with trigger point palpation referred pain, distant to the trigger point site may be seen on examination on occasion.
The examiner may notice a localized muscle Twitch or jump sign when examining the muscle trigger point. Tender points on the other hand are associated with fibromyalgia syndrome and are multiple by definition pain, allodynia, and hyperalgesia are also seen with tender points. Tender points do not have palpable knots and do not have a jump sign while pain and allodynia may spread outside of the tender point region.
A referred pain pattern is not typically seen.
Myofascial
- Myofascial pain
- Taut bands
- Palpable nodule
- Referred pain often
- Single or multiple
Fibromyalgia
- Fibromyalgia syndrome
- No taut bands
- No palpable nodule
- No referred pain
- Multiple by definition
Overlap Between Myofascial Pain and Fibromyalgia
- Pain
- Allodynia
- Hyperalgesia
Adjunctive Approaches: Stepped Approach
Healthcare practitioners use a stepped approach to the treatment of fibromyalgia and myofascial pain. Both pharmacologic and non-pharmacologic approaches are used and shown in this diagram. Stepwise treatment should be tailored to meet patient's individual needs. Patients are encouraged to be active participants in their care, regardless of the approach, the following diagrams will elaborate on the individual treatment steps.
Step 1
Education, Aerobic Exercise, Treat Co-morbidities
A good first treatment step includes education about fibromyalgia. It is helpful for patients to understand typical fibromyalgia symptoms and how the condition evolves over time. Early on. It is helpful to educate patients about the symptoms of fibromyalgia, typical treatment approaches and expectations.
Paced aerobic exercise should be introduced and co-morbidities including depression and anxiety should be addressed. Adjunctive approaches and complimentary alternative medicine therapies such as Tai Chi acupuncture and massage may be useful at any stage in treatment. Other adjunctive approaches such as trigger point and topical medications may reduce co-existing myofascial pain.
The RIGHT exercise will help improve fibromyalgia pain.
Aerobic Exercise
Helpful Tips
- Start low and go slow
- Whole body stretches prior to work out
- Paced aerobic training 4 days/week
- Light strength training 2-3 days/week
- Avoid high resistance exercise
- Be patient! It may take 1-2 months before seeing results
The wrong exercise routine may flare pain in fibromyalgia patients. On the other hand, a carefully paced exercise program is an effective treatment for fibromyalgia pain. Here are some workout tips to give to fibromyalgia patients prior to exercise one, choose your own pace and intensity fibromyalgia patients may choose a less intense routine, but still get significant benefits with less discomfort.
Adherence will be improved to stretch prior to your workout. Three, do aerobic exercise for at least four days a week for about 20 to 30 minutes, each session four, do strength training two to three days per week. Five, avoid high resistance exercise workouts. When resistance exercises introduced. It should include moderate repetitions of low resistance.
It takes time to see results, stick with the program and make it a routine. It is normal to have a mild increase in pain when starting exercise on a bad day, modify your activity level, which may include alternating rest and activity. But don't stop completely.
Step 2
Physical therapy, 1st line medications
A second step in fibromyalgia treatment included adding physical therapy. If patients have difficulty exercising on their own formal physical therapy may be helpful. Aqua therapy is equally effective and is a good option for patients with comorbid arthritis, physical therapist, with experience treating chronic pain may be preferred as they understand that fibromyalgia patients acquire a slower pace and less aggressive approach.
If the physical therapy is too aggressive, fibromyalgia patients are likely to stop. First-line medications are introduced at this step. These medications are used off label for fibromyalgia pain and are usually chosen first because they are less expensive and easily covered by insurance plans.
Tricyclic, antidepressants, and cyclobenzaprine are believed to work by increasing norepinephrine and serotonin that modulating the descending pain pathways. They may also improve sleep.
Gabapentin is believed to work by binding to neurons and decreasing the release of neurochemicals that transmit pain.
Step 3
2nd line medications
As part of the third treatment step pregabalin, duloxetine milnacipran and Tramadol are often prescribed pregabalin, duloxetine and milnacipran are FDA approved for fibromyalgia and are often more expensive. Pregabalin is an anticonvulsant, which is believed to work by binding to neuronal calcium channels in the central nervous system and decreasing release of chemicals that transmit pain.
Duloxetine and milnacipran our duel serotonin and norepinephrine re-uptake inhibitors. They are believed to decrease pain by increasing central nervous system, serotonin and norepinephrine and enhancing activity of the descending inhibitory pain pathways. Tramadol is a synthetic opioid that also increases central nervous system serotonin.
It has a lower abuse potential than typical opioids. It is a scheduled and controlled pain medication. It should be used cautiously in select patients.
- Pregabalin
- Duloxetine
- Milnacipran
- Tramadol
Step 4
Multi-disciplinary Treatment, Combination Drug Tx.
The final step is to coordinate care from a variety of practitioners in the form of an interdisciplinary treatment. It is useful if the practitioners work together to guide the patient's treatment. At this point, fibromyalgia medications are often combined to improve symptom relief. A rational treatment approach may include using medications with different mechanisms of action, like antidepressants and anticonvulsants at the same time.
Caution is advised when combining multiple medications as this can increase side effects.
Treatment Team
- Physician
- Physical therapist
- Nursing
- Integrative medicine practitioner
- Psychologist
- Occupational therapist
Just as we perform targeted physical exams, the treatment team provides targeted treatment. This starts with asking the patient about the symptoms they want to address. First fibromyalgia patients will likely report multiple concerns, including pain, poor sleep, depressed, mood, and fatigue. In these cases, a comprehensive treatment approach is optimal.
Various practitioners provide unique information for the patient. When these approaches are used together, the outcome is best.
Various members of the treatment team that work with patients to modify behaviors, make ongoing lifestyle changes and improve function and quality of life communication between the members of the treatment team, optimizes efficacy.
Targeted Treatment
Fibromyalgia pain may be improved by combining a number of treatment strategies. The physician may begin by prescribing appropriate medications, physical therapists, work with patients to improve conditioning and develop an aerobic exercise and stretching routine. The integrative medicine practitioner provides pain relief via complimentary therapies, such as Tai Chi, acupuncture, massage and craniosacral therapy.
Relaxation and other psychological techniques reduce stress and pain. Cognitive therapy can help patients modify negative thoughts that exacerbate pain, occupational therapists teach body mechanics to reduce pain and improve function, evaluation and modification of the workstation may improve productivity.
Each team member can use various forms of targeted treatment.
For Pain
- Physician
- Anticonvulsants
- Antidepressants
- Muscle relaxants
- Physical Therapist
- Aerobic Exercise
- Reconditioning
- Stretching
- Integrative Medicine Practitioner
- Tai Chi
- Acupuncture
- Massage
- Craniosacral therapy
- Psychologist
- Stress management
- Cognitive behavioral therapy
- Relaxation techniques
- Occupational Therapist
- Body mechanics
- Work station modification
For Sleep
- Physician
- Sleep medications
- Screen for sleep apnea, refer for sleep study
- Stimulants
- Physical Therapist
- Paced aerobic exercise
- Nursing
- Sleep habits
- Review list for sedating medications
- Psychologist
- Relaxation training
- Visual imagery
- Occupational Therapist
- Pacing skills
- Work simplification
Sleep Improvement
Fatigue and sleep can be improved with a variety of approaches. Paced, aerobic exercise improves sleep. Nursing staff may provide information about improving sleep habits and adjusting nightly routines. They can also screen for sedating medications, psychological techniques, such as relaxation techniques and guided imagery are helpful for patients with difficulty falling asleep.
The occupational therapists are helpful to guide patients with difficulty completing their daily activities, secondary to fatigue. They can also advise patients who tend to overexert themselves on a daily basis and thereby exacerbate their pain levels.
For Mood
- Physician
- Antidepressants
- Anxiolytics
- Encourage health habits
- Physical Therapist
- Paced aerobic exercise
- Psychologist
- Counseling
- Stress management
Self-Efficacy
Improving self-efficacy is an important part of fibromyalgia treatment. Self-efficacy is the patient's belief that she can successfully control her symptoms and achieve treatment goals. Fibromyalgia patients with a strong sense of self efficacy will have less pain and improved function. Self-efficacy can also be defined as the patient's locus of control.
A patient with a strong internal locus of control believes that her actions control her pain and symptoms. A patient with an external locus of control believes that her symptoms are unmanageable. They tend to be hopeless and helpless and function poorly overall.
Locus of Control
External
"Fibromyalgia controls me"
Internal
"I control my fibromyalgia"

