History of Present Illness

Devon, a fifteen year old black male presents to the ED (July 5th) with severe, uncontrolled pain (numeric rating scale score of 10/10). The pain, while widespread, seems to be the worst in the distal lower extremities and hips. A common pain assessment tool completed by Devon is available here. The patient has a past medical history of sickle cell disease and avascular necrosis of the hip. This is his fourth ED visit at this institution in the last six months with two of the previous visits resulting in admission. The ED triage team suspects drug seeking behavior. Rapid urine drug screen performed at intake positive for hydrocodone, hydromorphone, and cannabis.
Medical / Surgical History
Sickle Cell Disease, Avascular Necrosis of the Right Femoral Head
Social / Family History
+ tobacco (0.5 ppd), + etoh (3-4 12 oz beers / week), + cannabis use (a couple times per week). Denies other rec drug use. Pt is adopted with little information regarding biological parents other than significant drug abuse history with biological mother
Insurance
Illinois Public Assistance (Medicaid)
Primary Provider
Non listed, previously pediatrics.
Review of Systems
Constitutional
No fever reported with this episode
HEENT
Denies visual impairment, hearing loss, headache
CV / Pulm
Denies wheezing, shortness of breath, cough, palpitations, or swelling.
Abdomen
Denies acute locus of pain in abdomen, denies N/V/D/C. Reports diminished appetite
GI
Denies urinary difficulty, change in urine, blood in urine, prolonged or painful erection
Musculoskeletal
Reports pain in both hips resulting in limp, worse today than normal
CNS
Reports difficulty with focusing and concentration
Psych
Normal affect with appropriate speech, dress, and hygiene
Current Medications (based on patient H & P)
- Acetaminophen 500mg tablets sig. Take 2 tablets every 6 hours as needed for pain
- Hydrocodone 5mg/ acetaminophen 325mg tablets sig. Take 1-2 tablets every 4-6 hours as needed for pain
- Hydroxyurea 500mg capsules sig. Take 2 capsules every morning
- Celecoxib 200mg capsules sig. Take 1 capsule twice daily
- Folic acid 1mg tablets sig. Take 1 tablet every morning
- Multivitamin w/ iron tablets sig. Take 1 tablet every morning
Over the counter / herbal medications
Denies use
Allergies
Penicillin (hives, rash), codeine (nausea, itching)
Physical Exam
Vitals
BP 145/70 mmHg right arm sitting, HR 98 bpm, Temp 98.6 F, RR 18, Wt 72 kg, Ht 68 in, Pain 10/10 now, 8/10 least, 10/10 worst, and 9/10 average previous 24 hours
General
WDWN black male in acute distress. Alert, agitated, and oriented X 3.
HEENT
PERRLA, TMI, NCAT, thyroid midline, symmetrical & anodular, no cervical LAD
CV/Pulm
RRR, no m/g/r, +S1/S2 no S3, no apical bruits, no wheezes, rales, or rhonchi noted.
Abd
Soft, NTND, no guarding or rebound tenderness, decreased BS X 4 quadrants
GI/GU
Deferred
Musculoskeletal
Preserved strength and ROM bilaterally UE. Diminished strength and significant guarding and pain on passive and active ROM bilaterally LE. Unable to externally rotate either hip on PA.
Ext
No c/c/e, normal skin turgor, pale, cap refill > 3 sec
CNS
CN II-XII grossly intact, DTR + 3 bilaterally. Full affect and linear thought pattern.
Previous Discharge Summaries
September 14th, previous year
Admitting diagnosis: Pain (electronic record not avail)
February 1st, this year
Admitting diagnosis: Pain (electronic record not avail)
January 13th, this year
ED treated and released: Pain
Discharge Summary
Result type: Discharge Summary
Result Date: Jan 13, 202020
Result status: auth
Result title: ED discharge summary
Encounter Info: 236190028756, Emergency 1/13/2020
DC SUM
Patient name: Devon Smith
Age: 15
MRN: xxxxxxx
Attending Physician: E. Darlene Settler, M.D.
Dictating Physician: E. Darlene Settler, MD
Discharge Summary
Account#: xxxxxxx
Date of Admission: 1/13/2020
Date of Discharge: 1/13/2020
Cc:
Admitting Complaint:
Severe pain in lower extremities and hip.
History of present illness
This patient is a 15-year-old male with a history of sickle cell disease and uncontrolled acute on chronic pain. His current medication regimen includes Acetaminophen 500 mg tablets 2 tabs every 4-6 hours as needed, Hydroxyurea 500 mg capsules 2 tabs every morning, Celecoxib 200 mg capsules 1 tablet every morning and Multivitamin w/Iron 1 tablet every morning.
Patient denies any over the counter or other supplemental medication. Denies use of any illicit drugs. Allergies include Penicillin (hives,rash) and codeine (nausea, itching).
Vital signs were all within normal limits, no fever.
On physical examination, range of motion of the right and left hip were normal, Palpation of the right hip elicited moderate pain while no pain was elicited upon palpation of the left hip. No muscle atrophy was noted in either leg, hip or pelvis.
Patient was treated with Morphine 4 mg IV and Ketorolac 10 mg IV which provided relief of the pain. All labs were within normal limits. No blood transfusion was required. Patient was discharged with a follow up appointment made for tomorrow with his primary care physician.
Discharge Instructions
The patient is being discharged to home with the plan to follow up with his primary care physician tomorrow where they will review and make recommendations for continued care of his sickle cell disease. He was continued on all of his current home medications. No further analgesics were ordered for use after discharge.
March 18th, this year
Admitting diagnosis: Pain
Discharge Summary
Result type:Discharge Summary
Result Date: March 18, 2020
Result status: auth
Result title: ED discharge summary
Encounter Info: 236190028756
DC SUM
Patient name: Devon Smith
Age: 15
MRN: xxxxxxx
Attending Physician: Jaclyn Smarjessi, M.D.
Dictating Physician: Jaclyn Smarjessi, MD
Discharge Summary
Account#: xxxxxxx
Date of Admission: 3/18/2013
Date of Discharge: 3/21/2013
Cc:
Admission Diagnosis: Avascular Necrosis of the Hip
History of present illness
This patient is a 15-year-old male admitted from the emergency department with a history of sickle cell disease and uncontrolled acute pain. His current medication regimen includes Acetaminophen 500 mg tablets 2 tabs every 4-6 hours as needed, Hydroxyurea 500 mg capsules 2 tabs every morning, Celecoxib 200 mg capsules 1 tablet every morning and Multivitamin w/Iron 1 tablet every morning.
Patient denies any over the counter or other supplemental medication. Denies use of any illicit drugs. Allergies include Penicillin (hives,rash) and codeine (nausea, itching).
On physical examination, range of motion of the right and left hip were limited and painful in all ranges, with most pain being felt in abduction and internal rotation. Palpation of the right hip region revealed extreme tenderness. The left hip tenderness was less severe. Muscle atrophy was noted in the right thigh musculature. An orthopedic surgeon was consulted on 3/18/2013. His recommendations included conservative treatment at this time with activity restriction and partial weight bearing.
Patient was treated Morphine PCA and Ketorolac IV while providing joint rest. No major laboratory abnormalities were present. No blood transfusion was required. Patient was discharged with a follow up appointment made for one week with his primary care physician and a follow up in one month with the orthopedic surgeon.
Discharge Instructions
The patient is being discharged to home with the plan to follow up with his primary care physician in one week where they will review and make recommendations for continued care of his sickle cell disease with avascular necrosis of the right hip. He was continued on all of his current home medications.
May 8th, this year
Admitting diagnosis: Pain
Discharge Summary
Result type:Discharge Summary
Result Date: May 8, 2013
Result status: auth
Result title: ED discharge summary
Encounter Info:236190028756
DC SUM
Patient name: Devon Smith
Age: 15
MRN: xxxxxxx
Attending Physician: Jaclyn Smarjessi, M.D.
Dictating Physician: Jaclyn Smarjessi, MD
Discharge Summary
Account#: xxxxxxx
Date of Admission: 5/8/2013
Date of Discharge: 5/13/2013
Cc:
Admission Diagnosis: Avascular Necrosis of the Hip
History of present illness: This patient is a 15-year-old male re-admitted from the emergency department with a history of sickle cell disease and uncontrolled acute pain and avascular necrosis of the right hip. His current medication regimen includes Acetaminophen 500 mg tablets 2 tabs every 4-6 hours as needed, Hydroxyurea 500 mg capsules 2 tabs every morning, Celecoxib 200 mg capsules 1 tablet every morning and Multivitamin w/Iron 1 tablet every morning.
Patient denies any over the counter or other supplemental medication. Denies use of any illicit drugs. Allergies include Penicillin (hives,rash) and codeine (nausea, itching).
On physical examination, range of motion of the right and left hip were more limited that seen two months ago during his last admission. Patient stated that hip and lower extremity pain has been present almost continuous for two months with limited relief with activity restriction. His orthopedic surgeon was consulted on 5/8/2013. The radiology report stated that there was marked irregularity to the right and left femoral head. Orthopedics recommended right and left hip core decompression and bone grafting. No blood transfusion was required. Patient received two liters of normal saline and two doses of 1.0mg hydromorphone IV push with good response. Patient was discharged with a follow up appointment made for one week with his primary care physician and a follow up in one month with the orthopedic surgeon.
Discharge Instructions
The patient is being discharged to home with the plan to follow up with his primary care physician in one week where they will review and make recommendations for continued care of his sickle cell disease. He was continued on all of his current home medications.
PDMP
| Last Name | First Name | Street Address | City | Date Filled | Label Name | Strength | Metric Qty/Days Supply | Payment Type 2 | Pharmacy Name/City | Prescriber Name |
|---|---|---|---|---|---|---|---|---|---|---|
| SMITH | DEVON | PO Box 850 | Alton | 31 JUNE | HYDROCODONE-ACETAMINOPHEN | 5MG-500MG | 20/4 | PRIVATE PAY | WALGREENS/ALTON | PATEL, DUPREET MD |
| SMITH | DEVON | PO Box 850 | Alton | 15 JUNE | HYDROCODONE-ACETAMINOPHEN | 5MG-500MG | 20/4 | MEDICAID | WALGREENS/ALTON | PATEL, DUPREET MD |
| SMITH | DEVON | PO Box 850 | Alton | HYDROCODONE-ACETAMINOPHEN | 10MG-325MG | 60/30 | MEDICAID | WALGREENS/ALTON | PEDI, CHRIS ANP | |
| SMITH | DEVON | PO Box 850 | Alton | HYDROCODONE-ACETAMINOPHEN | 10MG-325MG | 60/30 | PRIVATE PAY | WALGREENS/ALTON | PEDI, CHRIS ANP | |
| SMITH | DEVON | PO Box 850 | Alton | HYDROCODONE-ACETAMINOPHEN | 5MG-325MG | 20/3 | MEDICAID | WALGREENS/ALTON | PEDI, CHRIS ANP | |
| SMITH | DEVON | PO Box 850 | Alton | HYDROCODONE-BIT-IBUPROFEN | 7.5-200MG | 65/18 | MEDICAID | WALGREENS/ALTON | PEDI, CHRIS ANP | |
| SMITH | DEVON | PO Box 850 | Alton | HYDROCODONE-BIT-IBUPROFEN | 7.5-200MG | 65/18 | MEDICAID | WALGREENS/ALTON | PEDI, CHRIS ANP | |
| SMITH | DEVON | PO Box 850 | Alton | ALPRAZOLAM | 0.25MG | 10/10 | MEDICAID | WALGREENS/ALTON | PEDI, CHRIS ANP | |
| SMITH | DEVON | PO Box 850 | Alton | HYDROCODONE-BIT/ACETAMINOPHEN | 325-10 MG | 120/15 | MEDICAID | WALGREENS/ALTON | PEDI, CHRIS ANP | |
| SMITH | DEVON | PO Box 850 | Alton | HYDROCODONE-BIT/ACETAMINOPHEN | 325-7.5 MG | 120/30 | MEDICAID | WALGREENS/ALTON | PEDI, CHRIS ANP | |
| SMITH | DEVON | PO Box 850 | Alton | HYDROCODONE-BIT-IBUPROFEN | 7.5-20MG | 65/18 | MEDICAID | WALGREENS/ALTON | PEDI, CHRIS ANP | |
| SMITH | DEVON | PO Box 850 | Alton | HYDROCODONE-ACETAMINOPHEN | 7.5-750MG | 40/10 | MEDICAID | WALGREENS/ALTON | PEDI, CHRIS ANP |
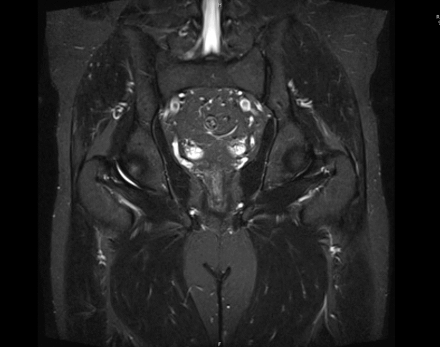
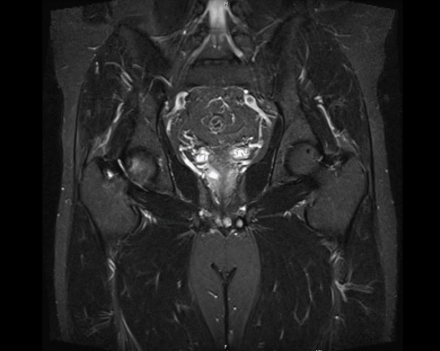
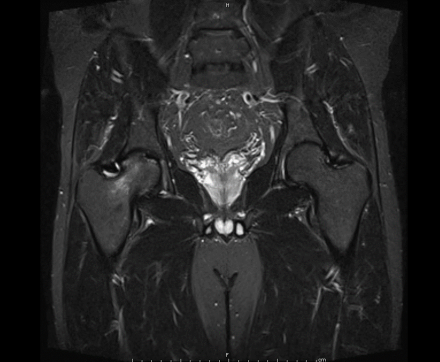
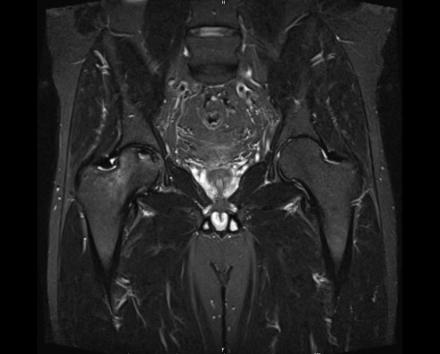
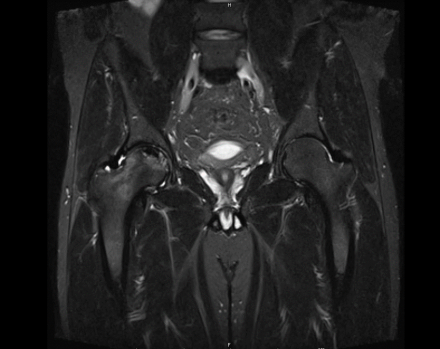
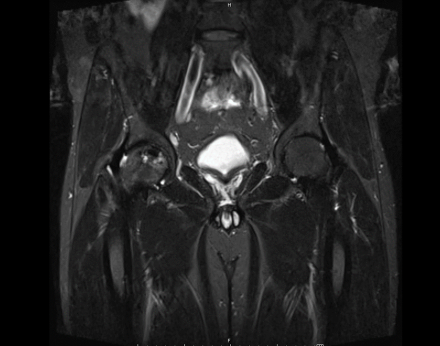
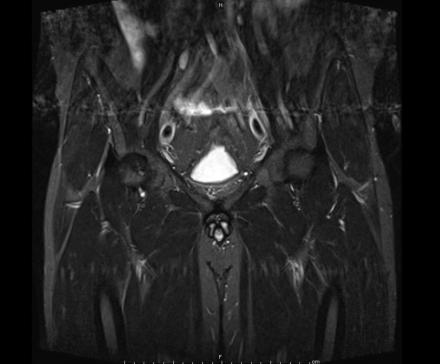
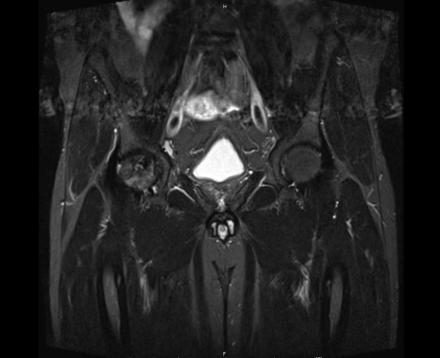
MRI Report
Smith, Devon M. ORDERING: HERNDON, CHRISTOPHER PHARMD
MRN: MD00548654 ACCT: D00000598654
SEX: M ORD SITE: ST. ELSEWHERE HOSPITAL
STUDY DATE REPORT # PROCEDURE CODE PROCEDURE
HIPWOCR MRI HIP W/O RT
IMPRESSION
AVASCULAR NECROSIS OF THE FEMORAL HEAD BILATERALLY WITH MILD ASSOCIATED CYSTIC
CHANGES IN THE FEMORAL HEAD AND REACTIVE BONE MARROW EDEMA RIGHT GREATER THAN LEFT. MILD SUBCHONDRAL BONE IRREGULARITY WITHOUT SIGNIFICANT COLLAPSE AT THIS TIME.
SMALL RIGHT HIP JOINT EFFUSION.
HISTORY
3 YEAR HISTORY OF CHRONIC HIP PAIN.
RIGHT AND LEFT HIP MRI WITHOUT CONTRAST 09/24/11
COMPARISON: HIP RADIOGRAPHS, 03/24/2010.
TECHNIQUE
CORONAL T1 AND STIR. AXIAL T1 AND T2 FAT-SAT. SAGITTAL PROTON
DENSITY FAT-SAT. CORONAL OBLIQUE STIR OF THE RIGHT HIP.
FINDINGS
IN THE RIGHT HIP, THERE IS AN AREA OF AVASCULAR NECROSIS IN THE SUPERIOR FEMORAL HEAD MEASURING AT LEAST 4.0 X 3.1 CM. THIS INVOLVES GREATER THAN 50% OF THE SUPERIOR WEIGHTBEARING ASPECT OF THE FEMORAL HEAD. CHARACTERISTIC CURVILINEAR SCLEROSIS AND EDEMA AT THE BORDER OF THE LESION. THE SUBCHONDRAL FRAGMENT IS SOMEWHAT SCLEROTIC, WITH THICKENED CORTEX. NO SIGNIFICANT COLLAPSE IS SHOWN AT THIS TIME. ASSOCIATED REACTIVE BONE MARROW EDEMA IN THE FEMORAL NECK. SMALL RIGHT HIP JOINT EFFUSION. IN THE LEFT HIP, THERE ARE ONLY MILD DEGENERATIVE CHANGES WITH SMALL OSTEOPHYTES OF THE FEMORAL HEAD AND ACETABULUM. NO JOINT EFFUSION OR SUBCHONDRAL BONE CHANGES. SACROILIAC JOINTS AND PUBIC SYMPHYSIS ARE UNREMARKABLE.
ELECTRONICALLY SIGNED BY:
IRMA BLANCO, MD
CC: HERNDON, CHRISTOPHER PHARMD
Sagittal Imaging: T1 Weighted

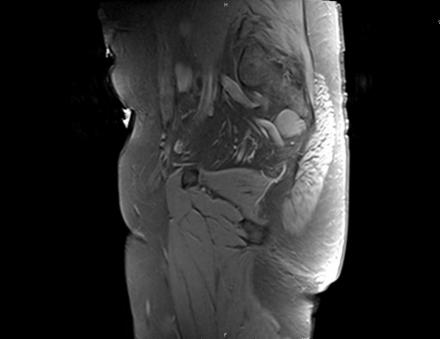
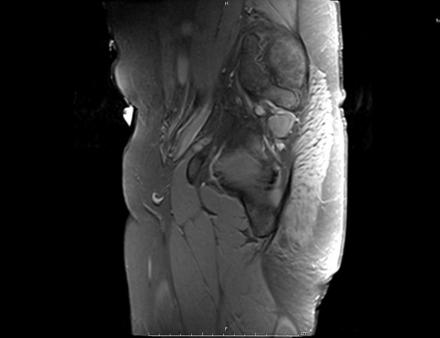
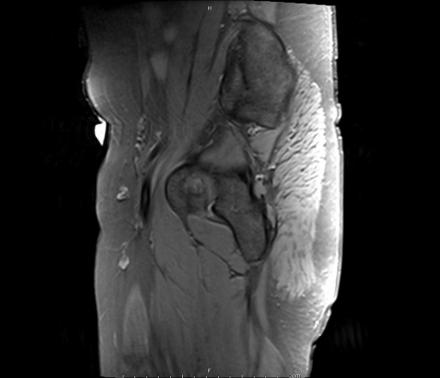
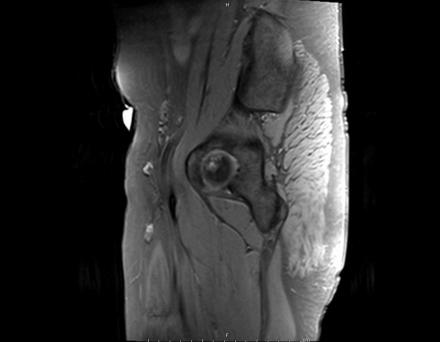
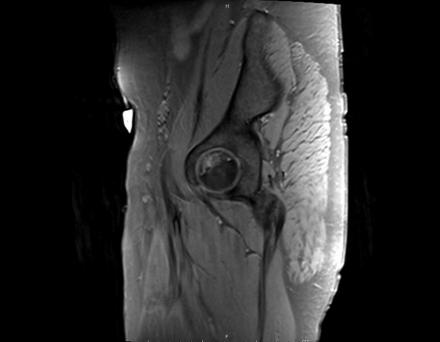
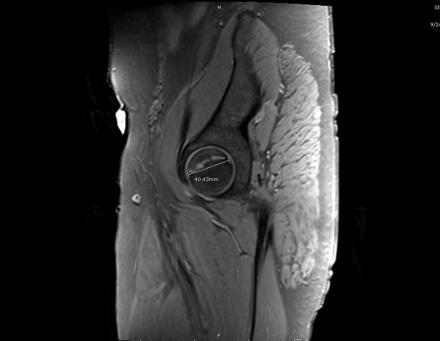
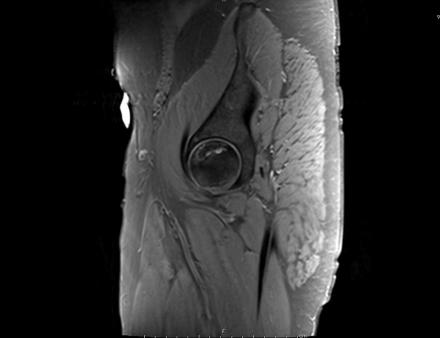
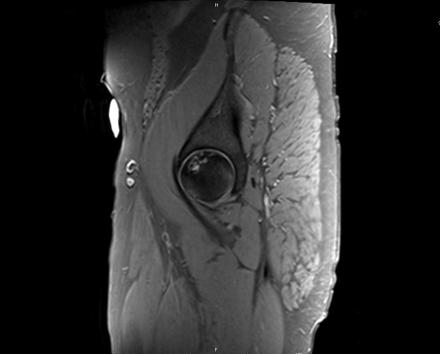
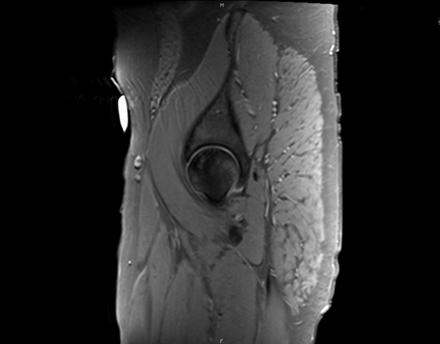
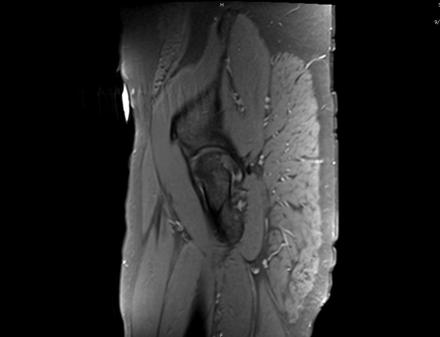
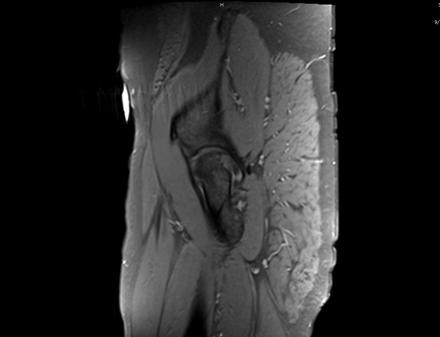
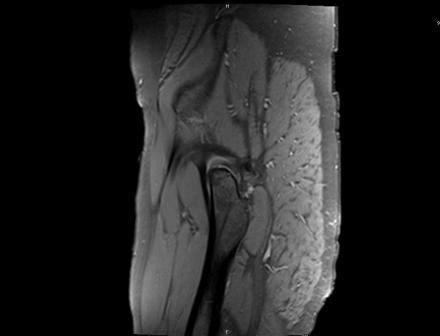
Axial Imaging: T1 Weighted
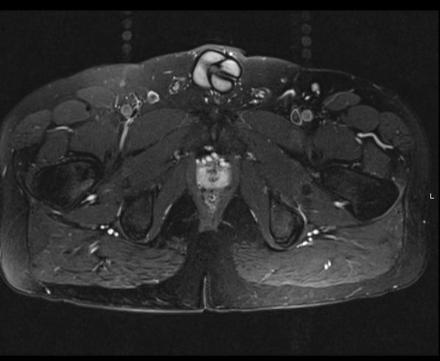
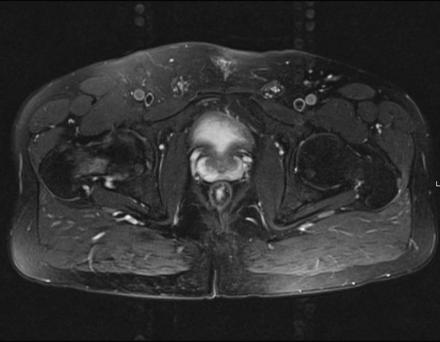
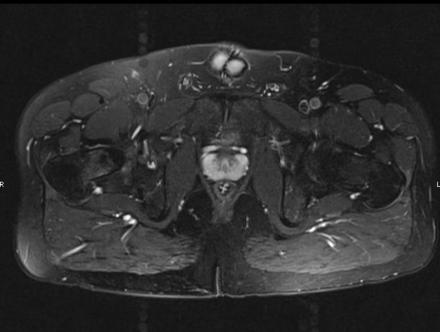
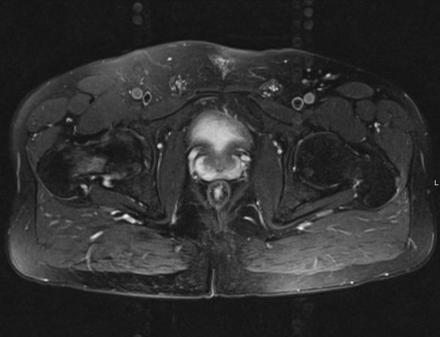
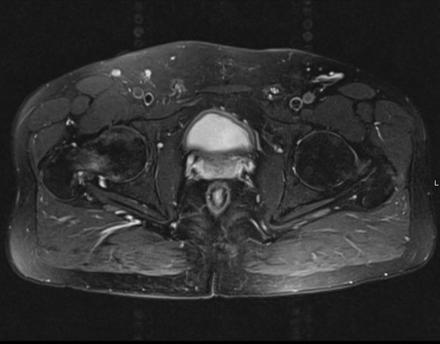
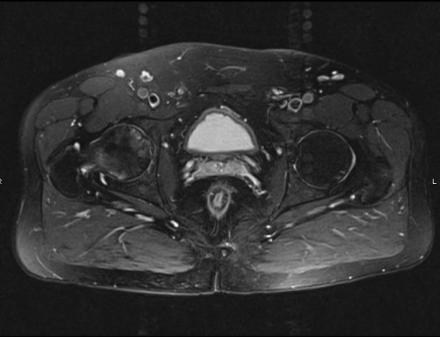
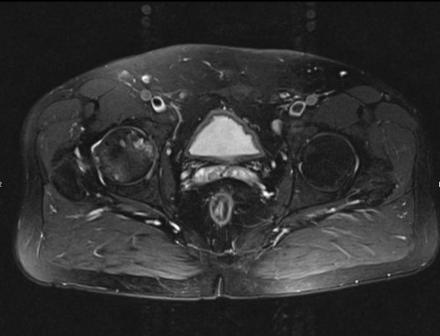
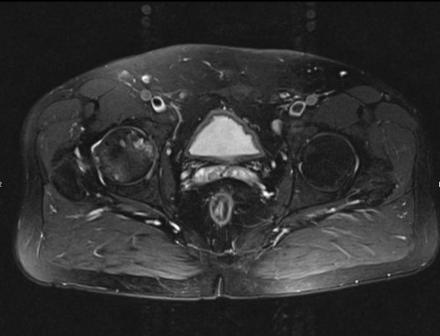
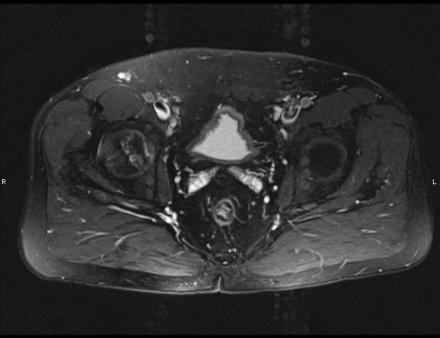
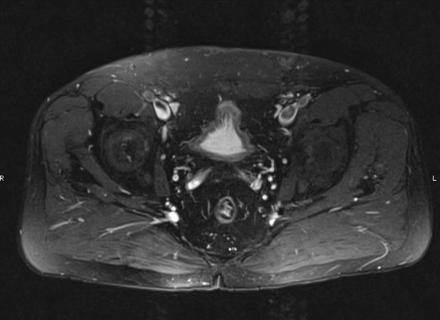
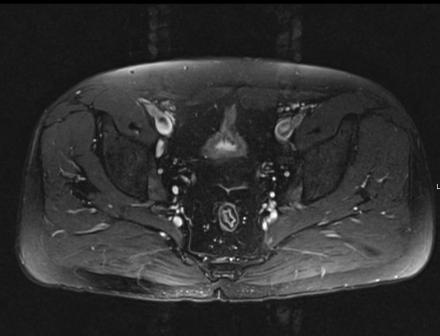
Coronal Imaging: T1 Weighted
Lab Work
| Test Type | Normal Range | Current Admission | 13-May | 12-May | 11-May | 10-May | 9-May | 8-May | 21-March | 20-March | 19-March | 18-March | 13-Jan |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WBC | 4.0-9.8 | 4.2 | 5.9 | 6.3 | 7.8 | 9.7 | 11.2 | 13 | 9.7 | 9.9 | 10.8 | 11 | 10.5 |
| Hgb | 11.8-14.8 | 6.4 | 7.9 | 7.9 | 8.1 | 8 | 8.1 | 8.2 | 7.8 | 7.8 | 8.1 | 8.6 | 8.5 |
| Hct | 35.5-44.0 | 18.5 | 27.8 | 28.3 | 27.7 | 28.1 | 18.7 | 22 | 23.5 | 23.3 | 24.7 | 26.1 | 24.4 |
| Plt | 140-350 | 362 | 310 | 340 | 345 | 330 | 355 | 370 | 365 | 360 | 375 | 380 | 352 |
| MCV | 82-99 | 80.8 | 84.8 | 84.2 | 84.5 | 84.1 | 84.2 | 83 | 86.1 | 85.7 | 87.3 | 87.3 | 85.6 |
| RDW | 11.5-14.5 | 18.7 | 16 | 16.6 | 16.8 | 16.6 | 17.2 | 17.2 | 15 | 15.9 | 16.1 | 15.8 | 17.4 |
| Retic | 0.7-2.9 | 18.8 | 8.9 | 9.8 | 10 | 9.2 | 11.9 | 11.9 | 6.8 | 7.2 | 7.8 | 8.4 | 9.5 |
| Sodium | 135-145 | 138 | 139 | 138 | 137 | 140 | 144 | 143 | 136 | 138 | 141 | 135 | |
| Potassium | 3.5-4.9 | 4 | 3.6 | 3.5 | 3.3 | 3.5 | 3.7 | 3.5 | 3.5 | 3.6 | 3.5 | 3.9 | |
| Chloride | 96-108 | 107 | 105 | 106 | 107 | 108 | 114 | 105 | 106 | 105 | 107 | 105 | |
| CO2 | 22-30 | 22 | 26 | 24 | 22 | 23 | 22 | 22 | 24 | 24 | 25 | 23 | |
| Calcium | 8.6-10.2 | 8.9 | 8.8 | 8.9 | 8.7 | 9 | 8.8 | 8 | 8.8 | 8.7 | 8.7 | 9 | |
| BUN | 6-20 | 6 | 5 | 6 | 3 | 4 | 3 | 6 | 4 | 3 | 6 | 8 | |
| SCr | 0.51-0.95 | 0.58 | 0.5 | 0.46 | 0.44 | 0.49 | 0.4 | 0.4 | 0.5 | 0.46 | 0.45 | 0.53 | |
| Glucose | 65-99 | 85 | 99 | 98 | 98 | 88 | 106 | 92 | 97 | 94 | 99 | 114 | |
| LDH | 135-214 | 301 | 115 | 300 | 425 | 185 | 299 | 322 | 296 | ||||
| Albumin | 3.4-4.8 | 4.2 | 4.3 | 4.3 | 4.1 | 4 | 4.1 | 4.4 | |||||
| T Bili | 0.2-1.0 | 2.1 | 0.9 | 1 | 2.3 | 0.8 | 24 | 1.2 | |||||
| AST | 12-32 | 28 | 30 | 33 | 36 | 29 | 24 | 33 | |||||
| ALT | 0-31 | 30 | 28 | 30 | 29 | 19 | 18 | 30 |
Consult Notes
Orthopedics
Consult Note
Result type: Consultation
Result Date: March 18, 2020
Result status: auth
Result title: Consultation Report
Encounter Info:236190028756
Patient name: Devon Smith
Age: 15
MRN: xxxxxxx
Attending Physician: Jaclyn Smarjessi, M.D.
Consulting Physician: Marcelle Olysaki, M.D.
Dictating Physician: Marcelle Olysaki, MD
Consultation Report
Account#: xxxxxxx
Date of Consultation: 3/18/2013
Date of Discharge: 3/21/2013
Cc:
Admission Diagnosis
Avascular Necrosis of the Hip
History of present illness
This patient is a 15-year-old male admitted from the emergency department with a history of sickle cell disease and uncontrolled acute pain. His current medication regimen includes Acetaminophen 500 mg tablets 2 tabs every 4-6 hours as needed, Hydroxyurea 500 mg capsules 2 tabs every morning, Celecoxib 200 mg capsules 1 tablet every morning and Multivitamin w/Iron 1 tablet every morning. Patient denies any over the counter or other supplemental medication. Denies use of any illicit drugs. Allergies include Penicillin (hives,rash) and codeine (nausea, itching).
Assessment
On physical exam range of motion of the right and left hip were limited and painful in all ranges, with most pain being felt in abduction and internal rotation. Palpation of the right hip region revealed extreme tenderness. The left hip tenderness was less severe. Muscle atrophy was noted in the right thigh musculature. Bone scan revealed a cold area in the right and left hip.
Impression/Plan
Recommendation at this time is to provide conservative treatment due to the patient’s age. Patient should have restriction of activity with only partial weight bearing and increase in analgesia until pain relief is achieved. We will follow up with the patient as needed.
Behavioral Health
Behavioral Health Consult Note
Result type: Consultation
Result Date: May 18, 2020
Result status: auth
Result title: Consultation Report
Encounter Info:236190028756
Patient name: Devon Smith
Age: 15
MRN: xxxxxxx
Attending Physician: Jaclyn Smarjessi, M.D.
Consulting Physician: Marcelle Olysaki, M.D.
Dictating Physician: Marcelle Olysaki, MD
Consultation Report
Account#: xxxxxxx
Date of Consultation: 5/18/2013
Cc:
Admission Diagnosis
Sickle Cell Disease, Avascular Necrosis of the Hip, Depression
History of present illness
This patient is a 15-year-old male admitted through the emergency department with a history of sickle cell disease and recent, uncontrolled pain. His current medication regimen includes Acetaminophen 500 mg tablets 2 tabs every 4-6 hours as needed, Hydroxyurea 500 mg capsules 2 tabs every morning, Celecoxib 200 mg capsules 1 tablet every morning and Multivitamin w/Iron 1 tablet every morning.
Patient denies any over the counter or other supplemental medication. Acknowledges use of illicit drugs x 1-3 months, including marijuana and opiates that he has purchased off the street. Allergies include Penicillin (hives,rash) and codeine (nausea, itching). He denies previous psychological/psychiatric treatment.
Current functioning
The patient is oriented x 3. He provides a coherent history of his present illness that includes an increasing number of pain exacerbations over the past year. Recent hospitalization led to a diagnosis of avascular necrosis of the right hip. Because of hip and low back pain, the patient has been unable to engage in his previous social and recreational activities (he previously played sports).
He has missed significant time from school over the past 2 months, as well. He reports that current levels of pain range between 3/10 and 8/10—his present hospitalization through the emergency department was triggered by an extended exacerbation of 8/10 pain.
He is reluctant to discuss his emotional state, but acknowledges that the pain and his resulting inability to be active have “got him down.” He further notes that he has little idea as to how to cope with pain exacerbations other than to use substances and medications that are available to him.
Assessment
- Severe pain secondary to sickle cell exacerbation
- Adjustment disorder with depressed mood
- Significant pain-related interference with customary role function
- Coping skills deficit relative to management of pain and emotional sequelae
Plan
- Confer with treatment team regarding planned medical/surgical/rehabilitation management of current exacerbation.
- Consider psychiatric consultation regarding possible initiation of anti-depressant medication, preferably one with analgesic properties.
- Consider psychological follow-up on discharge to address behavioral strategies for pain management (hypnosis and/or relaxation training, pacing activities, restoration of role function (importantly school attendance).
- There may be value to some family therapy to assist parents in developing an approach that can support patient’s coping efforts.
Social Work
Social Work Note
Devon is a 15 year old adolescent diagnosed with sickle cell disease living in New York City. He is African American, a high school sophomore, the youngest of 3 children; his sister Charmayne is 17 years old and a senior in high school; brother Eric, age 19 is a freshman in a local college and living at home. Neither have sickle cell disease. Devon’s mother is a pre-school teacher and his father a transit police officer. The family is Baptist. Additionally grandparents and aunts and uncles create an extended family system that is both a support and a challenge for Devon as they are often involved in his medical care especially during pain crises and have varied values and beliefs related to adolescents, pain, and medications. Devon reports that some of his more religious aunts and uncles suggest that bearing pain and suffering are spiritual paths to redemption and others act as if he is exaggerating his experience.
While Devon has reported no use of illicit drugs through May, in July a urine toxicology is positive for hydrocodone, (prescribed), hydromorphone, (metabolite of hydrocodone) and cannabis, which Devon acknowledged using prior to urine toxicology results. He now also acknowledges use of tobacco (0.5 ppd), + etoh (3-4 12 oz beers / week) and cannabis use (a couple times per week). Aside from recreational drinking in his family and experimental substance use by his brother the only history of addiction is a maternal uncle who has a history of cocaine abuse and currently attends Narcotics anonymous.
Devon reports changes in his function consequent to more frequent pain crises. He no longer participates in sports and describes an isolation and confusion in his relationship to peers. Additionally his access to opioids has complicated both his peer and family relationships. He has been pressured by peers to sell or give away his hydrocodone and at the same time various members of his family now worry that he is or will become an “addict”. In exploring the context in which he smokes, drinks and smokes marijuana it is clear that these shared activities are a way that he feel part of a peer group.
Assessment
In addition to the normal developmental challenges of adolescence, Devon’s life in complicated by a chronic life-limiting illness which includes pain crises that have interfered with developmentally appropriate activities (school and sports), required inpatient hospitalizations and access to controlled substances which increase his vulnerability to peer pressure and the worry of his family who fear the potential for addiction. Devon has an ambivalent relationship with medications - they often relieve his pain, provide him a potential path to acceptance and esteem amongst peers at the same time that he reacts to family and clinician worry that he is drug seeking. During a developmental stage marked by the work of developing an identity and separating from family Devon struggles with the complications of an identity that includes “sickler” and is now confused further by worry about becoming an “addict”.
Interventions
Psycho education
- In consult with selected team members provide information related to:
- Difference between addiction, dependence and abuse and the public health and political climate influencing prescribing of controlled substances to enhance awareness of the context in which pain is viewed.
- Introduce the concept of safety and its unique relationship to Devon’s illness – Risks and responsibility are shared by clinicians, prescribers, pt and family with the result that Devon’s safety as well as enhancing his quality of life is a primary goal of all
- Enhanced risk for Devon related to substance use behaviors – smoking, alcohol and marijuana; purchasing medications from the street
- After exploring further the context in which these behaviors occur, problem solve to create other choices for Devon to participate with peers while unobtrusively minimizing use of substances.
Cognitive interventions focused on:
- Explore the meaning attributed to identity as “sickler”, often heard in health care settings, with goal of assisting Devon and his family to identify emotional reactions to labels and reframe meaning from a disease that becomes who you are to a person who manages a disease as part of their life
- Consider the meaning and impact of pain crises in Devon’s life and the life of his family objectifying the spiritual and religious values for discussion and analysis with the goal of lessening their unspoken power over Devon’s sense of self
- Introduce the concept of pain as multidimensional to encourage Devon to look beyond his physical self to emotional, cognitive aspects of self that are malleable and influence his experience of the disease and pain.
Family interventions – in consult with Devon:
- Assist family with framing the complexity of the task that asks them to react and assist Devon as he moves through periods of physical dependence and then return to a style that encourages and allows his striving for independence – a challenge unique to families with adolescents who manage a chronic illness.
- In order to support autonomy and defuse pain and sickle cell disease as Devon’s core identify explore family’s responses to determine those that are supportive of his developmental goals and those that may need to be adapted. .
- Assist Devon and his parents to evaluate the change in his substance use from May through July to explore the factors that may have influenced this behavior such as lack of structure provided in school etc.
Individual counseling
- Assist Devon to weigh the risks and benefits of sharing health related and medication information with selected peers to inform decision making
- Introduce internet links that have been vetted and may provide peer support for adolescents managing pain and chronic illness
- In consult with teams members introduce music, art, and technology as interventions to enhance pain coping skills.
Systems & team interventions
- Consider a prescribing schedule that avoids the need for Devon to wake in the night or take medications to school.
- Explore community resources for comprehensive health care given Devon’s developmental stage and the need to build trust and continuity over time for Devon and his family as he moves toward adulthood.
- Assist Devon and his family to understand the value of decreased Emergency department visits not as a way to withhold treatment but rather to replace crises care with stable access to comprehensive quality community care that supports his life in the community.
- Explore Devon’s readiness to counseling with a community mental health clinician specialized in adolescence to continue to assist Devon and his family to negotiate adolescence in the setting of a chronic life-limiting illness.
Hematology/Oncology
Consult Note / Hematology – Oncology Service
Result type: Consultation
Patient name: Devon Smith
Age: 15
MRN: 49234
Attending Physician: Tait, Ray
Consulting Physician: Hecht, Keith
Dictating Physician: Hecht, Keith
Consultation Report
Account#:
Date of Consultation:
Cc: Severe pain
Admission Diagnosis
History of present illness
This is a 15-year old African –American male well known to our service for management of sickle-cell disease. We have had him taking hydroxyurea to try to prevent acute painful crises. The dose has been titrated from 500mg daily to 1000mg daily. We had been managing his pain with scheduled celecoxib and PRN acetaminophen. Was admitted to hospital in March with hip pain that was found to be related to avascular necrosis. He was supposed to follow up with us regarding his sickle cell and with orthopedics regarding his hip. He missed his appointment that was scheduled for April. He called our office on the morning of admission stating that the pain has become unbearable and wanting us to call out something stronger for him. Since he missed his previous appointment our office would not send out prescriptions. We referred him to the emergency room for further evaluation and acute management of his pain.
Impression/Plan
Patient with history of sickle cell disease admitted with severe pain likely due to progression of necrosis in hips. We have been able to avoid blood transfusions with him in the past. Recommend blood transfusion if hemoglobin < 7 g/dL or if he is experiencing shortness of breath. Consider imaging of hips to evaluate progression. Also recommend consulting orthopedics for evaluation of surgical intervention. Initiate opioids to get current pain under control. Will continue to follow patient while admitted and schedule follow up in my office one week after discharge. Will be sure to discuss with him the importance of keeping appointments and clarify expectations for pain medications.


