Objectives
Image

At the end of this session the participant will:
- Describe sleep patterns in older adults.
- Identify common sleep abnormalities.
- Discuss medications used to improve sleep quality.
Issues of Age Overview
80% of elderly have sleep complaints
34% insomnia
15% non-restorative sleep
20% sleep-disordered breathing
20% restless legs syndrome
0.5% rapid eye movement (REM) sleep behavior disorder
Issues of Age
- Sleep disorders result in daytime sleepiness, which is a known factor in automobile accidents
- A particular concern when driving skills may already be impaired by age-related declines in reaction time and information processing
- Sleepiness and disturbed nocturnal sleep may increase the risk of falls
- May lead to hip fractures or other trauma
- Disturbed sleep and nocturnal delirium (sundowning) is a major factor in precipitating the transfer of elderly patients to nursing homes
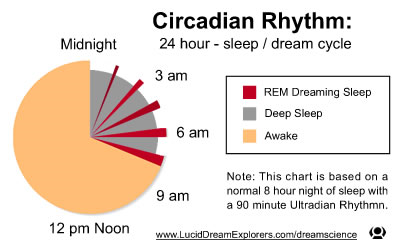
Circadian Rhythm
Image
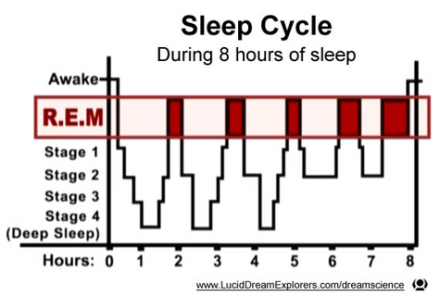
Sleep Cycle
Image
Circadian Disruption
- Inadequate exposure to zeitgebers (e.g., exposure to light and dark), resulting in defective circadian rhythmicity
- Insufficient exercise due to physical infirmity
- Poor exposures to light in those confined to long-term care facilities
- Irregular meal times associated with living alone
Changes in Sleep Architecture with Age
- Nocturnal sleep becomes lighter, more frequently disrupted, and shorter
- Sleep efficiency decreases to 70%-80% compared with > 95% for younger individuals
- Higher number of arousals and awakenings
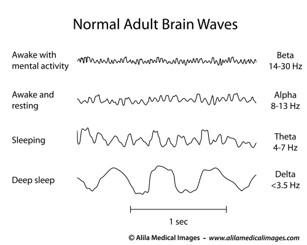
- Greater proportion of nonrapid eye movement (NREM) I sleep at the expense of deeper stages of sleep (i.e., NREM II and III)
- Slow-wave sleep starts to decline about age 20 and may disappear entirely in the later years.
- Slow waves have a frequency of 0.5-2.0 (delta waves) with an amplitude of > 75 µV
- REM sleep declines with age
- Defect in the ability of the individual’s circadian pacemaker to respond appropriately to various zeitgebers, such as exposure to morning bright light
- Tendency for circadian rhythms to phase advance (i.e., move the time of sleep onset and awakening forward )
Normal Adult Brain Waves
Image
Consequences of Sleep Deprivation
- Increase in pain sensitivity
- Increase in sympathetic cardiac modulation
- Decrease in parasympathetic cardiac modulation
- Impaired immune response
- Alteration in metabolic and endocrine systems
- Behavioral: impaired attention and psychomotor performance, increased daytime sleepiness, and impaired mood that includes fatigue and irritability
- REM deprivation may include mood and memory alterations
Reference
Bonnet & Arand, 2003
Physical Disorders that Disrupt Sleep
Physical and emotional disorders take their toll on sleep depth and continuity
- Rheumatologic disorders
- Pain, inability to change position
- Parkinson disease
- Inability to change position
- Congestive heart failure
- Orthopnea/paroxysmal nocturnal dyspnea
- Chronic lung disease
- Dyspnea, cough, wheezing
- Diabetes
- Nocturia*
- Peripheral neuropathy
- Prostatism
- Nocturia*
*Nocturia is the leading cause of disturbed sleep
Medications/Preparations that May Disturb Sleep
Medications
- Anticonvulsants
- Levodopa
- Diuretics
- Bronchodilators
- Thyroid replacement
- Calcium antagonists
- Corticosteroids
- Beta-blockers
- Antidepressants that are activating
Preparations
- Herbal preparations (gingko, caffeine, ginseng)
- Nicotine
- Caffeine
Emotional Disorders that Can Affect Sleep
- Depression
- Anxiety associated with bereavement
- Major life changes such as retirement
- Fear of dying
- Post-traumatic stress disorder
Freedom to Nap?
- Sleep requirements
- No changes in sleep requirements
- Sleep is rescheduled
- Less sleep at night and more during the daytime napping
- Excessive daytime sleepiness is often considered a “normal” attribute of aging and therefore frequently goes unrecognized and unreported
- Early-morning awakenings may be secondary to depression or significant comorbidities
- Freedom to nap
- Retirement, boredom
Sleep Disorders with Increased Prevalence in the Elderly
Restless Leg Syndrome (RLS)
- Irresistible urge to move the legs during periods of inactivity
- 80% of patients with RLS will also have periodic limb movements in sleep (PLMS)
- Patients often complain of sleep-onset insomnia because of the irresistible urge to move their limbs
Periodic Limb Movement Disorder (PLMD)
- Movement of the legs occurring in a repetitive manner during sleep
- Movement may cause frequent arousals
- Sleep maintenance insomnia
- Daytime symptoms of sleepiness
- Estimated 4% of younger age group has PLMD/RLS
- Age > 60: > 20% endorse symptoms of RLS
- Age > 65: 45% had > 5 PLMS
- Don’t treat everything that moves
Reference
Ancoli-Israel et al., 1991
RLS/PLMD in the Elderly
- Treatment often involves dopamine agonists pramipexole and ropinirole
- A side effect can be sleepiness
- Gabapentin also useful and has a favorable profile to decrease evening pain and promote sleepiness (pregabalin)
- Renal excretion: decrease dose in elderly
- Clonazepam useful; however, must be used cautiously in the elderly
- Hip fractures increased
- Long half-life of 20 hours
- Opioids very effective (acetaminophen with codeine)
- Careful use of benzodiazepines and opioids with COPD and untreated sleep-disordered breathing
Sleep Disorders with Increased Prevalence in the Elderly: Sleep-Disordered Breathing
- 2%-4% of the adult population have sleep apnea syndrome (laboratory diagnosis plus symptoms); middle-aged working adults
- 20% at age 60
- After menopause, sleep apnea prevalence between males and females the same
- Edentulous subjects (those who remove their dentures at bedtime) have more sleep apnea than do control subjects
- Smoking is a risk factor for sleep apnea
Sleep-Disordered Breathing (SDB)
- Sleep-disordered breathing may accelerate dementia due to hypoxemia
- SDB exacerbates hypertension with resultant cerebrovascular disease, reduced cerebral blood flow during respiratory events leading to localized infarcts or the effect of repeated hypoxia
- Cognitive function in older persons with mild-moderate sleep-disordered breathing is related to the amount of respiratory disturbances occurring at night. Increase in respiratory disturbance index was associated with cognitive performance over time
- Treatment typically for symptomatic disease
Reference
Cohen-Zion et al., 2004
Treatments for Sleep-Disordered Breathing
- Positive airway therapy
- Oral appliance, mandibular advancement devices
- Uvulopalatopharyngoplasty with cure rates ranging 30%-50%
- Many elderly individuals are not surgical candidates due to comorbid conditions
- Avoidance of alcohol and sedative agents prior to bedtime
- Sleep position training for patients with predominantly supine sleep apnea
Rapid Eye Movement (REM) Behavioral Disorder (RBD)
- May be idiopathic
- Associated with CNS diseases
- Precipitated by medications
- Tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors
- Drug or alcohol withdrawal
- Responds well to melatonin and clonazepam
- RBD is characterized by violent behaviors during REM sleep due to loss of REM sleep atonia
- Behaviors are usually in context with a dream
- > 90% are males > 60 years of age
- Frequently seen in the α-synucleinopathies Parkinson disease, dementia with Lewy body disease, multiple system atrophy
Sleep and Dementia
- Senile dementia of the Alzheimer’s type (AD)
- More NREM I sleep
- Greater numbers of arousals and awakenings than occur in the nondemented elderly
- Nocturnal delirium (sundowning): defined as the appearance or exacerbation of behavioral disturbances at night
- Agitation, pacing, restlessness, inappropriate verbalization, decreased alertness, confusion, aggression, paranoid ideation
- Prevalence of sundowning in nursing home residents 12%-14%
- Prevalence of sundowning in AD 12%-25%
- Factors include: worsening dementia, nocturnal awakenings by caregivers, room changes, incontinence, and sensory deficits
- Neuronal degeneration of the suprachiasmatic nucleus and melatonin secretion
- Loss of circadian rhythmicity
- This affects the normal physiology of sleep, the biological clock, and core body temperature
- With disease progression, it becomes difficult to separate EEG features of NREM 1 and NREM II sleep
- Sleep spindles and K complexes are poorly formed, are of lower amplitude, are of shorter duration, and are much less numerous
- The percentage of time spent in REM sleep is reduced
- This decrease is attributed to degeneration of the nucleus basalis of Meynert
Reference
Weldemichael & Grossberg, 2010
Sleep and Dementia: Treatment
- Eliminate metabolic, toxic, pharmacologic, and infectious factors that may exacerbate delirium
- Avoid daytime napping
- Morning bright light
- Regular activities during the day
- Minimize nighttime awakenings (bed checks, lights on at night)
- Sleeping agents: melatonin first line, Z-drugs second line
- If all else fails: consider scheduling nighttime activities for the sundowning nursing home resident
Elderly and cognitively impaired populations:
- Often underreport pain
- May be nonverbal
- “Acting out” is often secondary to pain
- Acetaminophen at bedtime
- Melatonin
- Vitamin D
Don’t be afraid to treat the cognitively impaired!
Reference
Shega et al., 2012; Dalacorte et al., 2011
Vitamin D Study
- 2000 IU vitamin D daily
- Mayo Rehab Center: Rochester, NY; 267 outpatient chronic pain patients
- Vitamin D-deficiency group required more morphine
- Mean duration of opiate use: 71 months vs. 43 months
- Vitamin D-deficiency group averaged 133 mg/day opioid use vs. 70 mg/day in the Vitamin D-adequate group
Reference
Turner et al., 2008
Melatonin
- Melatonin to promote good sleep
- Decreases with age
- Neuroprotective effect
- Used in ICUs to decrease delirium
- Used with AD patients to blunt sundowning
- Doses: 0.5-10 mg 2 hours prior to anticipated bedtime
- Pharmacy grade (No B6!)
Treatment for Sleep
Medications
- Good sleep hygiene is the best “drug”
- Treat pain aggressively to improve sleep quality
- Acetaminophen at bedtime
- Hydrocodone
- Avoid diphenhydramine
- Treat underlying depression aggressively
- Melatonin--pharmacy grade
- Avoid B6
- Mirtazapine 7.5 mg
- Ask about new onset RLS
- Trazodone 12.5-50 mg
- Z-drugs: zaleplon, zolpidem, eszopiclone
Sleep Hygiene
- Regular bed times
- Regular wake-up times with bright light
- Avoid afternoon caffeine and tobacco
- Don’t fall asleep in front of the TV
- Avoid blue light 1 hour prior to sleep
- Limit afternoon nap to < 1 hour between 1 and 3 PM
Conclusion
- Sleep deprivation results in an increase in pain sensitivity
- Aggressively treat pain and depression
- Good sleep hygiene is the best medication
- Start with melatonin and vitamin D
- Add other agents slowly and carefully
- Avoid anticholinergics (diphenhydramine) and benzodiazepines
- Mirtazapine, trazodone, Z-drugs
References
- Ancoli-Israel, S., Kripke, D. F., Klauber, M. R., Mason, W. J., Fell, R., & Kaplan, O. (1991). Periodic limb movements in sleep in community-dwelling elderly. Sleep, 14(6), 496-500 http://www.journalsleep.org.libproxy.unm.edu/ViewAbstract.aspx?pid=24892
- Bonnet, M. H., & Arand, D. L. (2003). Clinical effects of sleep fragmentation versus sleep deprivation. Sleep Medicine Reviews, 7(4), 297-310, http://www.ncbi.nlm.nih.gov/pubmed/14505597
- Cohen-Zion, M., Stepnowsky, C., Johnson, S., Marler, M., Dimsdale, J. E., & Ancoli-Israel, S. (2004). Cognitive changes and sleep disordered breathing in elderly: Differences in race. Journal of Psychosomatic Research, 56(5), 549-553.
- Dalacorte, R. R., Rigo, J. C., & Dalacorte, A. (2011). Pain management in the elderly at the end of life. North American Journal of Medical Sciences, 3(8), 348-354, doi: 10.4297/najms.2011.3348 PMCID: PMC3234146, http://www.ncbi.nlm.nih.gov/pubmed/22171240
- Shega, J. W., Andrew, M., Hemmerich, J., Cagney, K. A., Ersek, M., Weiner, D. K., & Dale, W. (2012). The relationship of pain and cognitive impairment with social vulnerability – An analysis of the Canadian Study of Health and Aging. Pain Medicine, 13(2), 1-8.
- Turner, M. K., Hooten, W. M., Schmidt, J. E., Kerkvliet, J. L., Townsend, C. O., & Bruce, B. K. (2008). Prevalence and clinical correlates of vitamin D inadequacy among patients with chronic pain. Pain Medicine, 9(8), 979-984.
- Weldemichael, D. A., & Grossberg, G. T. (2010). Circadian rhythm disturbances in patients with Alzheimer’s disease: A review. International Journal of Alzheimer’s Disease, 10, 1-9, Article ID 716453, http://dx.doi.org/10.4061/2010/716453
Acknowledgements
Frank M. Ralls, M.D.
Assistant Professor, Internal Medicine
Sleep Disorders Center
University of New Mexico

