The emergency department physician ruled out a medical necessity in the hospital and recognized that the source of Jane’s complaint was a non-life threatening condition that is best managed by a dentist. Short-term pain relief was achieved with a local anesthetic block. Jane was instructed to see a dentist as soon as possible to obtain a definitive diagnosis and a long-term solution for her pain.
The dentist will now try to determine the definitive diagnosis through:
- Listening to the Jane as she gives a history of the present illness
- Looking at Jane by performing a problem focused dental exam
- Taking appropriate radiographs.
Jane Follows Up with the Dentist
Watch the initial interaction between the dentist and Jane at the emergency dental clinic.
Jane’s description of her symptoms and the treatment she received at the hospital ED is not sufficient to make a definitive diagnosis.
Summary of Visit to the ED
- Not a life-threatening medical condition
- Condition is best managed by a dentist
- Short-term pain-relief provided
- Instructions to see a dentist ASAP
To obtain a definitive dental diagnosis, the dentist must perform a problem-focused dental exam.
- History of present illness
- Problem-focused dental exam
- Clinical testing
- Radiographs
- Determine the diagnosis
Problem-Focused Dental Exam Part 1
Watch Jane and the dentist continue conversation at the emergency dental clinic.
Components of Problem-Focused Exam
- Visual Inspection
- Palpation
- Periodontal Exam
- Percussion
- Thermal Testing
Step 1: Visual Inspection
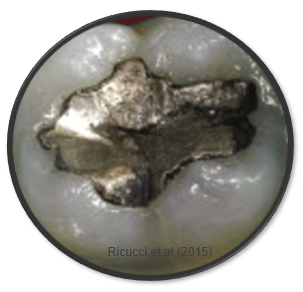
First, the dentist visually examines the area of concern, and notices a large silver filling that is showing wear at the margins.

Step 2: Palpation
The dentist will then digitally palpate the soft tissues around the area of concern. Patients with true dental infections often experience pain when digital pressure is applied to the area of infection.
The dentist did not observe visible swelling, and Jane did not experience discomfort when he palpated the soft tissue around the tooth. The dentist does not suspect a true bacterial infection, although this cannot be ruled out until all data are attained.
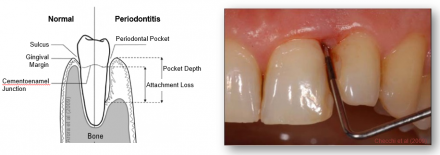
Step 3: Periodontal Exam
Next a periodontal exam is performed to see whether the problem originates from the gums rather than the tooth itself. Periodontitis, or gum disease, is one of the most common dental diseases in that it affects nearly 50% of all US adults. Periodontitis is most commonly detected by observation of gingival attachment loss, alveolar bone loss, and periodontal pocketing.
The dentist observes generalized inflammation and evidence of poor dental hygiene. Jane reports that she has been having difficulty brushing and flossing since the pain started two weeks ago.
Problem-Focused Dental Exam– Part 2
Watch as the dentist finishes his problem-focused exam.
Thermal Test
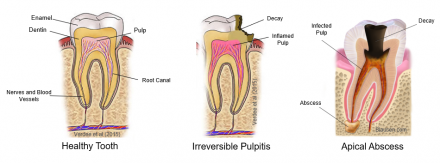
A patient’s response to the thermal test is a good indicator of dental pulp health.
- The first diagram illustrates a healthy tooth with normal pulp. The nerves and blood vessels within the root canal or around the root have no infection or inflammation. When tested, a healthy tooth typically has a non-painful response to a cold stimulus, which stops shortly after the stimulus is removed. A healthy tooth will not experience severe pain when tapped (percussed) or if the gum tissue is pressed over the root surface (palpation).
- The second diagram illustrates an inflamed tooth that is not infected, but painful. This condition is often inaccurately referred to as an “abscess”. This illustration demonstrates an unhealthy tooth that is inflamed; a condition referred to as pulpitis where the nerves and blood vessels of the dental pulp are still alive. In this illustration the tissue beyond the root is swollen and inflamed. When tested, a tooth with pulpitis will display an abnormal, painful and prolonged response to a cold stimulus, will experience moderate to severe pain when tapped (percussed), and may experience pain when pressing (palpating) the bone over the roots of the tooth. A patient with pulpitis will not present with swelling and antibiotics are not indicated since it is not an infection.
- The third diagram illustrates an unhealthy abscessed tooth that is infected. A patient with this condition is often swollen, in pain, and shows signs of regional lymphadenopathy and elevated temperature. When tested, the tooth typically is not responsive to thermal stimulation, but may be sensitive when tapped (percussed), and may experience pain when pressing (palpating) the bone over the roots of the tooth. The tooth often has visible signs of disease, such as decay. Antibiotics should be considered as part of the treatment for a patient with an abscessed tooth.
Summary of Findings
Let’s review the findings from Jane’s exam:
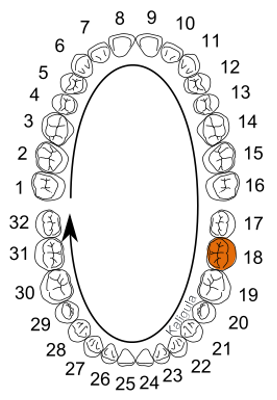
Based on United States nomenclature, the problem tooth is designated as tooth number 18.
- The tooth has an amalgam (metal) filling
- No visible or palpable swelling, or pain to digital pressure.
- Positive, painful, and lingering response to cold testing
- Painful response to percussion.
- Periodontal status (condition of gums) appears to be within normal limits
- Based on these findings, the dentist orders a periapical radiograph of tooth #18.
Tooth 18
Amalgam (Metal) Filling
Digital Pressure
Jane feels no pain with digital pressure.
Cold Testing
Jane has a positive, painful, and lingering response to cold testing.

Percussive Testing
Jane has a painful response to percussion.

Periodontal Inflammation
Jane has mild inflammation of the periodontal tissues.

Periodontal Radiographs
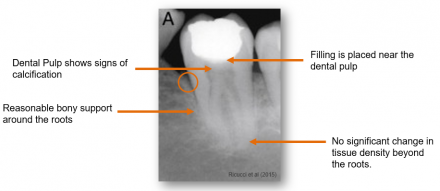
Periapical radiographs provide useful diagnostic information.
A radiographic image contains much useful information for the dentist in the diagnostic process for a toothache. This radiograph shows a molar that has a metallic filling in the crown of the tooth. It is white in color, indicating great radiodensity. Next, let’s look at the image of the dental pulp and root canals located directly beneath the metal filling. The pulp and root canals appear darker in color, meaning less radiodensity. Careful examination shows the root canals that extend to the ends of the roots of the tooth. The dentist will also take note of the position of the tooth in the jawbone, as well as radiographic presence or absence of pathology within or around the tooth. In this image, no pathology is evident at the end of the root, however we see the metal filling was placed near the dental pulp and remarkable radiographic changes within the pulp consistent with an unhealthy tooth.
The cottony, cloudlike appearance within the pulp chamber is a common finding in teeth with chronic pulpitis, which is an inflammatory condition of the dental pulp. Calcification of the pulp tissue often occurs when a tooth has or had a cavity and/or a filling.
The radiodense object seen in the crown of this tooth represents a filling placed near the dental pulp. This finding is significant for a few reasons. First, it indicates that the tooth was drilled-on in the past, and second, the tooth likely had a “cavity” (which is a bacterial infection). Both of these conditions may cause a future pulpitis.
The radiographic appearance of the bone around and in between the roots is normal though some bone loss is evident around the crown of the tooth.
Radiographic changes are not apparent around or beyond the roots of the tooth. A dental pulp abscess manifests itself as an apparent radiolucency at the apex of the root or abnormal widening of the space between the root and jaw bone. (These findings are not seen on this radiographic image). Radiographic findings are important to a dentist when considering treatment options; in this case, whether the dentist should recommend tooth extraction (pulling) and/or a root canal.
Diagnosis and Treatment Options
Watch as the dentist discusses the diagnosis and treatment options with Jane.
Post-operative Instructions (First 24 Hours)
- Do:
- Eat soft foods
- Limit strenuous activity
- Do not:
- Smoke
- Rinse vigorously
- Drink through a straw
- Clean the teeth next to the healing tooth socket
- Avoid:
- Hot liquids
- Alcoholic beverages
- Mouthwashes containing alcohol
After a discussion of the pros and cons of each treatment option, Jane has elected to have the tooth extracted. Following the extraction, the dentist provides Jane with post-operative instructions that she should follow during the next 24 hours. These include eating soft foods, limiting strenuous exercise, and avoiding activities that may irritate or put stress on the surgical wound, such as smoking, vigorous rinsing, drinking through a straw, consuming hot liquids, and drinking or using mouthwashes that contain alcohol. Jane also is advised to refrain from cleaning the teeth next to the healing tooth socket.
Because Jane does not have any issues that contraindicate NSAIDs or acetaminophen, the combination of these two drugs is the most appropriate treatment choice for relieving pain.
Pain Management
Alternate ibuprofen and acetaminophen every six hours.

