Pre and Post Test Questions
Question 1
What is the most appropriate tool to measure pain in the developmentally-delayed, non-verbal child?
Question 2
Question 3
Which of the medications below are indicated for mild pain?
Question 4
Which opioid is the standard opioid to use in the opioid-naïve child with moderate severe pain?
Question 5
When starting an opioid on a child with moderate-severe pain, what additional medication should be started?
Supplementary Teaching Materials
Learning Objectives
- Describe the anatomy and physiology associated with normal sensory transmission
- Define terms commonly associated with abnormal pain states (i.e. hyperalgesia, allodynia)
- Describe the difference between acute and chronic pain
- Classify pain syndromes (i.e. nociceptive, neuropathic, inflammatory)
Pain
Definition
“An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.” (IASP)
Additional definitions can be found at the International Association for the Study of Pain (IASP)
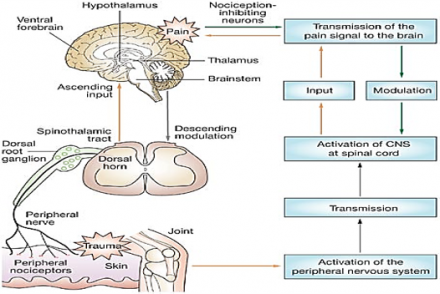
Pain Processing
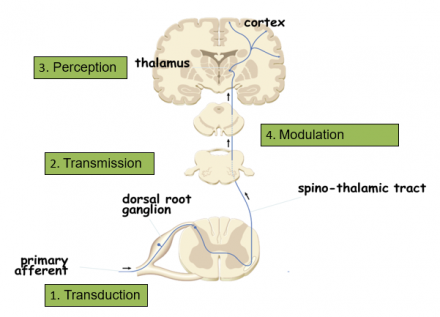
Transduction
- Nociceptors (free nerve endings) of A and C fibers are exposed to noxious stimuli
- Noxious stimuli include:
- mechanical (pressure, swelling, incision)
- thermal (burn, scald)
- chemical (neurotransmitters, toxic substance, ischemia, infection)
- Chemical messengers released by damaged cells may be targets for pharmacotherapy
- bradykinin
- serotonin
- substance P
- prostaglandins
- Chemical messengers may also sensitize nociceptors
Transmission
- Begins at the site of transduction traveling along the nociceptor fibers to the dorsal horn in the spinal cord
- Aδ and C fibers terminate in the dorsal horn
- Excitatory neurotransmitters are released propagating the signal from the spinal cord to the brain
- The pain impulse is transmitted from the spinal cord to the brain stem and thalamus via the ascending pathways
- The brain does not have a discrete pain center, so the impulse is processed at the thalamus and then directed to additional brain regions
Perception
- Pain becomes a conscious multidimensional experience
- Activation of multiple cortical regions
- The reticular system:
- responsible for the autonomic and motor response to pain (i.e. quickly removing a hand when it touches a hot stove)
- Somatosensory cortex:
- important for the interpretation of pain information being processed
- identifies the intensity, type and location of the pain sensation and relates the sensation to past memories and experiences
- Limbic system:
- responsible for the emotional and behavioral responses to pain
Modulation
- Beginning at the brain, the descending pain pathway utilizes inhibitory signals to block the pain signal from being processed in the spinal cord
- Descending inhibition involves the release of inhibitory neurotransmitters that produce analgesia
- Inhibitory neurotransmitters involved with the modulation of pain include:
- endogenous opioids, serotonin, norepinephirine, GABA
- Analgesics commonly used in the treatment of pain may produce their pharmacological actions through these neurotransmitter pathways
Descending Modulation
For additional resources on nociception:
Dubin A, Patapoutian A. Nociceptors: The sensors of the pain pathway. J Clin Invest; 2010; 120(11):3760-3772.
Bingham B, Ajit SK, et al. the molecular basis of pain and its clinical implications in rheumatology. Nature Clin Practice Rheumatology 2009; 5; 28-37.
Pain Categories
Nociceptive Pain
- Nociceptive Pain: Pain that arises from actual or threatened damage to non-neural tissue and is due to the activation of nociceptors
- Can be divided in to:
- Somatic
- Visceral
Nociceptive Pain Categories
- Somatic
- pain arising from tissues such as skin, muscle, tendon, joint and bone
- well localized
- Visceral
- pain arising from the internal organs. Often diffuse or referred
Neuropathic Pain
- Pain caused by a lesion or disease of the somatosensory nervous system
- Neuropathic pain is a clinical description and not a diagnosis
- Patients may describe the pain as burning, electric, searing, tingling, and migrating or traveling
- Some causes of neuropathic pain include:
- amputation (phantom limb pain), herpes zoster, AIDS (peripheral neuropathy), diabetic neuropathy, fibromyalgia, and cancers that affect the spinal cord, among others
Terms associated with neuropathic pain:
- Hyperalgesia
- increased pain from a stimulus that normally provokes pain
- Allodynia
- pain due to a stimulus that does not normally provoke pain
- Sensitization
- increased responsiveness of nociceptive neurons to their normal input, and/or recruitment of a response to normally sub-threshold inputs
Reference
International Association for the Study of Pain (IASP)
Inflammatory Pain
- A localized protective reaction of tissue to irritation, injury, or infection, characterized by pain, redness, swelling, and sometimes loss of function
- Activates the nociceptive pathway
- Examples of inflammatory pain include:
- appendicitis, rheumatoid arthritis and inflammatory bowel disease.
Time Course of Pain
- Acute
- typically does not last longer than three to six months, and resolves when the underlying cause of pain has been treated or has healed
- Chronic
- persists despite the fact that the injury has healed
- pain signals persist beyond three to six months and can last for years
Pain and Cognitive Impairment
- Recognize that pain is a frequent complication of motor impairment in certain populations with cognitive and neurological impairments (e.g., cerebral palsy)
- Recognize that individuals with cognitive and motor impairment have multiple potential sources of pain
- Be aware that people with cognitive impairments are not immune from the everyday pains suffered by non-individuals
- headaches, menstrual pains, toothache, and earache
- Be aware of the other pains that are commonly reported in patients with cognitive impairments
- musculoskeletal pain, pain from reflux esophagitis, constipation
- Recognize limited ability to communicate pain
Reference
Charlton JE. Pain issues in individuals with limited ability to communicate due to cognitive impairment. 2005; Core Curriculum for Professional Education in Pain. IASP Press, Seattle; Chapter 43:1-7
Absorption, Distribution, Metabolism, Excretion (ADME) of Drugs
Drugs are delivered to the body by different routes of administration.
- Pharmacokinetics includes:
- Absorption
- Distribution
- Metabolism
- Excretion
- Pharmacodynamics includes:
- Drug Target (Receptor)
- Mechanism of Action
- Drug Response
- Genes and gene variants can affect a drug’s response
Importance of ADME In the Clinical Use of Drugs
Why is ADME important in the clinical use of drugs?
Understanding the basic concepts of ADME is important because:
- ADME determines the onset, intensity, duration, and termination of drug action
- Drug metabolism is the major mechanism for termination of drug action
- Pharmacokinetic drug interactions can be associated with altered drug metabolism
- Idiosyncratic adverse drug events and drug-induced toxicity can affect drug metabolism
- In the future, ADME genotyping will be central to personalized medicine
The diagram below shows the absorption, distribution and metabolism of clinical drugs. In Nestor's case, the route is enteral, through the GI.
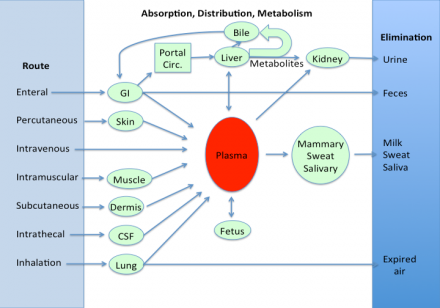
Factors Affecting Oral Absorption
- Disintegration of dosage form
- Dissolution of particles
- Chemical stability
- Resistance to enzymatic degradation
- Motility and mixing in GI tract
- Presence and type of food
- Passage across GI tract wall
- Blood flow to GI tract
- Gastric emptying time
Prodrugs
Prodrugs are agents developed to improve the pharmacokinetic properties of drugs (e.g., enhanced intestinal absorption)
- Codeine is a prodrug for morphine. Codeine is demethylated by the liver enzyme cytochrome P450 to morphine.
- Tramadol is a prodrug that is metabolized to a compound that binds to opioid receptors.
How Aging Affects Drug Metabolism
Our patient, at age 7, will metabolize many drugs more rapidly than a neonate or elderly patient.
Drug Metabolism (The Metabolic Fate of Drugs)
- Pharmacologic and clinical importance of drug metabolism:
- Major mechanism for the termination of drug action
- Basis of most pharmacokinetic drug interactions
- Activates prodrugs, such as tramadol
- May lead to the formation of toxic metabolites, (i.e., bioactivation, a major cause of drug and chemical toxicity) Acetaminophen is metabolized to a toxic compound
Drug Metabolism
- The most important oxidative reactions are catalyzed by CYTOCHROMES P450 (CYPs), a family of enzymes in the liver.
- CYPs catalyze 75% of drug-metabolism reactions
- ~90% of CYP-catalyzed reactions involve 5 CYPs
- CYP -1A2, -2C9, -2C19, -2D6, and -3A4/5
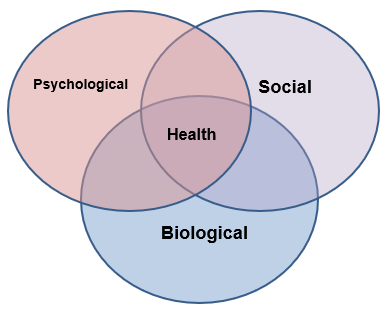
Biopsychosocial Model
- Health is best understood in terms of biological, psychological, and social factors rather than purely in biological terms
- It is critical to consider all three factors together to improve engagement in health behaviors and health outcomes
Reference
Engel GL. The need for a new medicinal model: A challenge for biomedicine . 1977; Science; 196(4286):129-136.
Community Health Nurse Visit
- CHN / Visiting Nurse Services
- Determine need and referral for additional supportive services in home / community setting such as:
- Around-the-clock or scheduled, periodic nursing care / home health aide care
- Rehabilitative care (physical therapy, occupational therapy, speech therapy)
- Hospice, respite care
- Social services, counseling
- Primary and acute medical and psychiatric care services
- CHN / Visiting Nurse Functions
- Components of home/community setting nursing
- assessment:
- Demonstrate awareness and sensitivity to patient’s culture and individual health beliefs, priorities
- Conduct organized, complete history of individual/family
- Conduct physical examination and documentation of home/community environment noting key features:
- Safe
- Clean
- Dry
- with Portable Water
- Adequate ventilation
- Proper human/animal waste management
Example of pediatric home environmental assessment.
Example of nurse observation instrument.
Opioid Conversion
- Refers to switch from one opioid to another to improve therapeutic response or reduce undesirable side effects
- Clinical situations warranting opioid rotation:
- Opioid escalation has yielded intolerable and unmanageable side effects
- Severe pain continues despite repeated dose escalation
- Switch to different route of administration or formulation
- Need for an opioid with different pharmacokinetic properties
- Cost considerations require a change in therapy
Additional factors to consider:
- Severity of patient’s pain
- Duration of opioid use
- Pharmacogenomics
- Medication history
- Clinical care environment
- Pharmacokinetic changes (age, comorbidities, gender)
Goal
- Effectively manage pain while ensuring patient safety
- Individualize therapy
- Collaborate with experienced clinicians
- Conservatively estimate doses
- Counsel patients and estimate doses
- Closely monitor patients
Reference
Knotkova H, Fine PG, Portenoy RK. Opioid Rotation: The Science and the Limitations of the Equianalgesic Dose Table. J Pain Symptom Manage 2009; 38:426-439
Opioid Rotation Steps
- Determine total opioid(s) use previous 24-hours
- Select the equianalgesic dose ratio that corresponds to the opioid and route that will be converted:
- “X” mg total daily dose of new opioid/mg total daily dose of current opioid = equianalgesic factor of new opioid/equianalgesic factor of current opioid
- Cross multiply the ratio to determine the total daily dose of new opioid
- Reduce the dose 25 – 50% (cross-tolerance)
- Determine how many long-acting doses per day patient should take
- Breakthrough dose 10% of long-acting daily dose
- Assess, respond, titrate according to opioid half-life
Calculations Used in Conversion Between Opiates
| Medication | Equianalgesic Dose IM/IV | Equianalgesic Dose PO |
|---|---|---|
| Morphine | 10 mg | 30 mg |
| Oxycodone | Not available | 20 mg |
| Hydromorphone | 1.5 mg | 7.5 mg |
| Fentanyl | 100 mcg |
24-hr MS Dose: 30 - 59 mg 60 - 134 mg 135 - 224 mg 225 - 314 mg 315 - 404 mg Initial Patch Dose: 12 mcg/hr 25 mcg/hr 50 mcg/hr 75 mcg/hr 100 mcg/hr |
| Codeine | 130 mg | 200 mg |
| Hydrocodone | Not available | 30 mg |
Developing Tolerance
- Tolerance develops more rapidly to drugs with low efficacy
- More receptors need to be activated to achieve a given physiological effect leading to a low receptor reserve
- With a high efficacy drug, fewer receptors need to be activated to produce the same physiological effect leaving a larger receptor reserve
Drug Tolerance
- Decreasing effectiveness of a drug when given over time to achieve the same physiological effect
- More opioid is needed to achieve the same level of analgesia
Dependence
- Dependence
- Altered or adaptive physiological state produced by repeated administration of a substance, resetting homeostatic balance. Individuals in this adapted, physically dependent state require continued administration of the substance to maintain normal function.
- Physical dependence
- Demonstrated through a withdrawal syndrome.
- Without withdrawing the drug or giving an antagonist, the degree of dependence is not known.
- Demonstrated through a withdrawal syndrome.
- Psychological dependence
- Manifested by an intense craving for the drug.
Potential Sources of Payment Coverage
- Medicaid – minimally required federal coverage
- Medicaid – state-specific expansions of coverage
- Medicaid – Waivers for innovative programs by state
- Private coverage- through an employed parent
Medicaid
- Insured must provide evidence of current resources to demonstrate eligibility
- Application required including disclosure of all sources of household income (wages, child support, etc.)
- Minimum federal requirements; States may choose to ease eligibility requirements or expand benefits within federal guidelines. State laws may vary significantly.
Medicaid Benefits by State
Searchable database, including comparison of prescription drug benefits by state:
State Health Facts: Medicaid Benefits. The Henry J. Kaiser Family Foundation
Median State Medicaid/CHIP Income (% of FPL) Eligibility Thresholds, 2009
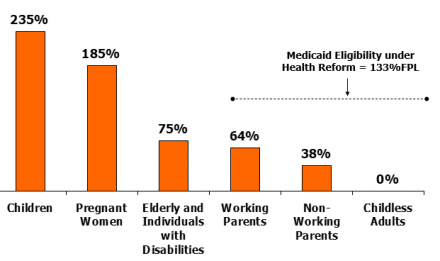
Children’s Eligibility for Medicaid/CHIP by Income, December 2009
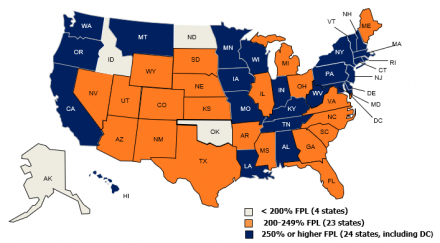
**IL uses state funds to cover children above 200% FPL. MA uses state funds to 400% FPL.
SOURCE: Based on a national survey conducted by KCMU with the Center on Budget and Policy Priorities, 2009.
Federal Requirements of States
General Requirements:
- Statewideness
- Freedom of choice of provider
- Same services for federally mandated groups and those covered under state discretion
Services
- Required services – nationally mandated
- Optional services – state-determined
New York State Medicaid
http://www.health.state.ny.us/health_care/medicaid/
New York State Medicaid Eligibility for Children & Parents, 2010
(NYS Dept. of Health, June 2010)
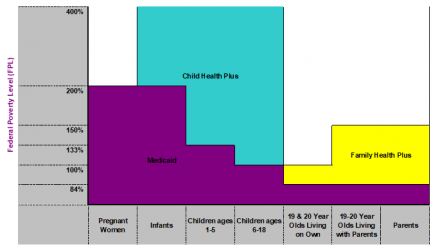
All Children Eligible
- High income families in New York State may enroll children in Child Health Plus and pay a low-cost premium
- Medicaid and/or Child Health Plus – seamless
- To better understand eligibility, go to: https://www.health.ny.gov/health_care/child_health_plus/eligibility_and_cost.htm
What is Covered by NYS Medicaid?
- No co-pays in managed care plans
- Medicare/other insurance premiums
- Treatment & preventive health and dental care (doctors and dentists)
- Hospital inpatient & outpatient care
- Lab & X-ray services
- Home health care
- Psychiatric hospitals care, mental health facilities, and facilities for the developmentally disabled
- Medicine, supplies, medical equipment, and appliances (wheelchairs, etc.)
- Transportation to medical appointments (i.e., public transportation/car mileage)
- Emergency ambulance transportation to a hospital
- Clinic services
- Nursing home care
- ….and more

