Equianalgesic Dosing
Equianalgesic refers to the approximate dose of an opioid which is required to elicit the same analgesic benefit of another opioid. Most opioids are compared to each other in terams of equianalgesic dose compared to oral morphine. While imprecise, the equianalgesic ratios are now being used to approximate the risk of harm from a particular dose of an opioid.
The table describes common analgesics and equianalgesic dosing between parenteral and oral applications.
| Drug | Parenteral Equianalgesic Dose (mg) | Oral Equianalgesic Dose (mg) |
|---|---|---|
| Morphine | 10 | 30 |
| Buprenorphine | 0.3 | 0.4 (sl) |
| Codeine | 100 | 200 |
| Fentanyl | 0.1 | N/A |
| Hydrocodone | NA | 30 |
| Hydromorhone | 1.5 | 7.5 |
| Meperidine | 100 | 300 |
| Oxycodone | 10 (not available in the US) |
20 |
| Oxymorphone | 1 | 10 |
| Tramadol | 100 (not available in the US) |
120 |
Reference
McPherson ML. Demystifying Opioid Conversion Calculations: A guide For Effective Dosing. Amer Soc of Health Systems Pharm, Bethesda, MD. 2010. Copyright ASHP, 2010. Used with permission. NOTE: Learner is strongly encouraged to access original work to review all caveats and explanations pertaining to this chart.
CDC Recommendations
The CDC guideline for Prescribing Opioids for Chronic Pain provide 12 key recommendations for safe opioid prescribing and are paraphrased as follows:
- Use nonpharmacologic and non-opioid modalities for pain prior to opioid modalities when possible.
- Establish realistic treatment goals with the patient
- Discuss known risks and realistic benefits of the drug therapy.
- Use the lowest dose possible with careful consideration when exceeding 50 mg of morphine equivalents daily and avoiding greater than 90 mg of morphine equivalents daily without "justifcation."
- Prescribe opioids for the shortest duration possibel with less than or equal to 3 days typically sufficient and greater than or equal to 7 days "rarely necessary."
- Evaluate benefits and harms of ongoing opioid use regularly.
- Assess risk for overdose and co-prescribe naloxone in cases of greater than or equal to 50 mg of morphine equivalents.
- Review the prescription drug monitoring program regularly.
- Assess adherence to therapy and aberrant drug taking behaviors by preforming random urine drug screening.
- Avoid concurrent prescribing of benzodiazepines with opioids.
- Frequently assess for opioid use disorder and offer medication assisted therapy (e.g., methadone or buprenorphine/naloxone).
Reference
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. MMWR Recomm Rep 2016;65:1-49. DOI: http://dx.doi.org/10.15585/mmwr.rr6501e1
Risk Mitigation Strategies
Risk Mitigation Strategies include (click on each to learn more):
- FDA Risk Evaluation and Mitigation Strategies
- Prescription Drug Monitoring Program Review
- Random urine, saliva, or blood toxicologic screening
- Observed pill counts
- Abuse deterrant formulations
- Risk assessment using validated screening tools
- Interdisciplinary communication
Opioid Use Disorder (OUD)
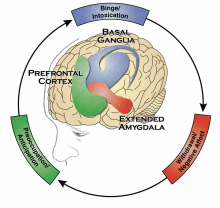
Opioid Use Disorder is a neurobiologic disorder characterized by:
- Use in larger amounts or longer durations than intended
- Personal desire to cut down or stop use, but unable to do so
- Excessive time spent in getting, using, or recovering from opioids
- Cravings
- Failure to honor personal commitments
- Ongoing use despite known harm to relationships or health
- Worsening phyiscal or psychological problems.
- Tolerance
- Withdrawal
Risk factors for opioid use disorder include:
- Family history of alcohol abuse
- Family history of illegal/illicit drug abuse
- Family history of prescription drug abuse
- Personal history of alcohol abuse
- Personal history of illegal/illicit drug abuse
- Personal history of prescription drug abuse
- Age between 16-45 years
- Personal history of ADD, OCD, bipolar, schizophrenia
- Personal history of depression or anxiety
The Opioid Risk Tool is a common scoring tool for assessing opioid abuse risk. You will need this information later in the module.
Reference
Webster LR. Anesth Analg 2017;125(5):1741-1748.
Naloxone Co-Prescribing
Naloxone is a non-selective, centrally-acting opioid antagonist available for administration either prenterally or intranasally.
Key takeaways:
- Co-prescribing of naloxone should always be considered when prescribing opioid or when illicit opioid use is suspected
- Many states have enacted laws to increase access to naloxone
- Patients or care-givers should be properly educated on the use of naloxone in the event of an opioid-overdose
Watch a brief video demonstration of naloxone delivery.

