Introduction to Sarah
Find out more about Sarah's experience with widespread pain and fibromyalgia.
Meet Sarah
- Whiplash injury after car accident
- X-ray films of cervical spine are normal
- Rest and ibuprofen
- Pain interferes with daily activity and work
- MRI of cervical spine shows small disc bulge at C5-C6
- No response from epidural injections, ibuprofen and hydrocodone
- Stops physical therapy secondary to pain
- Develops widespread pain and associated fatigue
Six weeks after her accident, Sarah calls her PCP and tells her about her continued neck pain. Sarah's PCP an MRI of her cervical spine. The MRI shows a minor disc bulge at C5 C6 without any nerve compression, based on the MRI findings, her PCP refers Sarah to a neurosurgeon and physical therapist.
The neurosurgeon performs three monthly epidural injections and prescribes hydrocodone. Sarah goes to the physical therapist, but quits after two sessions because it hurts the hydrocodone and ibuprofen do not improve her pain. And they upset her stomach. Since the day of her accident, her neck pain has not improved in many ways.
Sarah's pain is worse. She keeps her neck still because it hurts to move. She feels that the pain is now spread throughout her body. She is frustrated and feels exhausted all the time. She just wants the pain to go away and makes an appointment with her primary care physician.
Taking the Health History
Let's begin as the provider takes the patient's history. As you watch this video, there are typical errors that will affect decisions. There are also parts of the history that are well done. Will you be able to identify the differences you may want to jot notes as you watch?
Let's break down the individual components of the actual history.
Taking an Adequate Pain History
Fatigue
Fatigue is common in chronic pain patients, especially those with fibromyalgia studies of fibromyalgia patients show that fatigue may be a more disabling symptom than the pain itself. Sara's fatigue may be secondary to her pain and poor sleep. Alternatively, her fatigue may be a symptom of a comorbid condition such as depression and hypothyroidism.
Depression and hypothyroidism are commonly associated with chronic pain and fibromyalgia. The practitioner can use simple screening tools to test for depression. We are providing a link to some screening tools for mood disorders, asking about weight gain and hair loss can alert the practitioner to possible hypothyroidism blood work can be done to make the diagnosis.
Finally, it is helpful to screen for sedating medications, which may contribute to fatigue.
Ask questions to determine underlying cause of chronic fatigue.
- Poor sleep
- Mood disorder
- Hypothyroidism
- Sedating medications
It is helpful to discuss with the patient how fatigue affects daily function. Most patients will describe a reciprocal relationship or a vicious cycle of fatigue, pain, and sleep. Each symptom is problematic on its own and also makes the other symptoms worse.
Ask the patient how fatigue impacts her pain and daily function.
Sleep Cycles
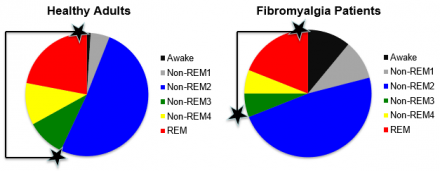
Sarah's report of chronic fatigue should naturally lead to a discussion of sleep. The vast majority of patients with fibromyalgia report, poor sleep for fibromyalgia patients. It's not just a problem with the number of hours spent sleeping, but also a problem with sleep quality. As you can see in the chart, fibromyalgia patients spend less time sleeping and more time.
They also have less deep sleep, which includes. Stages three and four sleep. These deep sleep stages are indicated by the areas between the two black stars stages. Three and four sleep are referred to as restorative sleep. Restorative sleep helps to support. Daytime function provides energy to the brain and body increases blood supply to muscles and supports tissue growth.
Patients who are deprived of restorative sleep as is seen with fibromyalgia patients. Report feeling unrefreshed upon awakening, fibromyalgia patients also report difficulty falling asleep and prolonged awakenings during the night.
Percentage of Time in Sleep Stages
Percentage of Time Healthy Adults and Fibromyalgia Patients Spend in the Different Sleep Stages
- Healthy adults sleep twice as long as fibromyalgia patients
- Healthy adults spend more time in deep sleep (stage 3-4 and REM)
Behaviors that may Contribute to Disrupted Sleep
Ask about behaviors that may contribute to disrupted sleep:
- Do you keep regular sleep hours?
- Do you nap during the day and for how long?
- Do you use stimulants such as caffeine and tobacco?
- How much alcohol do you consume?
- Are you active during the day?
- Do you snore loudly at night?
It is helpful to ask patients direct questions about behaviors which may contribute to poor sleep, a disordered sleep schedule, going to bed and awakening at irregular times may result in poor sleep and fatigue. Excessive daytime napping may contribute to insomnia stimulants like caffeine and tobacco may keep patients awake and excessive alcohol is known to disrupt the sleep cycle.
Inactivity and sedentary lifestyles are common contributors to poor sleep as well. Lastly, screening for obstructive sleep apnea is important. Ask fibromyalgia patients about loud snoring and excessive daytime sleepiness, despite adequate time in bed, as well as daytime headaches, which are all symptoms of obstructive sleep apnea.
If obstructive sleep apnea is suspected. A referral to a sleep specialist for a sleep study is warranted.
Somatic Symptoms
Do not assume that pain is the most pressing issue for your fibromyalgia patients while this may be true for some others may be more concerned with symptoms such as fatigue, lack of energy, poor sleep, and fibro fog. As the above graph shows fibromyalgia patients will often report Avastin of somatic symptoms during the history, ask the patient, which symptom do you want to improve the most?
This will help you focus your treatment plan. Keep in mind, some symptoms are related to the fibromyalgia while others may be secondary to a comorbid disorder requiring further exploration.
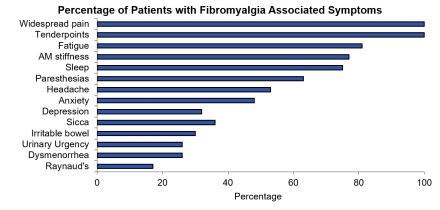
Reference
Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 199;33(2):160-72.
Fibromyalgia Patients and Disability
Most patients with fibromyalgia look fairly well, perform well on the physical exam in the office, and have seen many specialists and have undergone a number of tests which are negative. This has led some to describe fibromyalgia as an invisible disorder. A careful history, physical exam is the key to making the diagnosis.
This leads friends, family, and even some physicians to question whether their complaints are real. In fact many mistakenly consider fibromyalgia to be a psychiatric disorder. Despite their appearance, fibromyalgia patients may experience significant disability. As the graph shows fibromyalgia patients, miss work, school and social activities.
As a result of their symptoms, some patients with fibromyalgia may receive a disability pension.
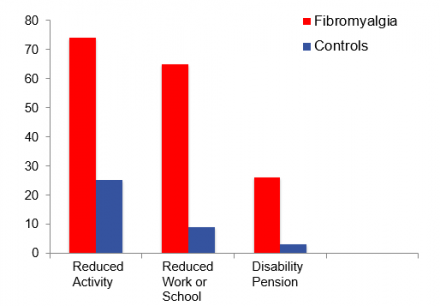
Reference
White KP, Speechley M, Harth M, Ostbye T. Comparing self-reported function and work disability in 100 community cases of fibromyalgia syndrome versus controls in London, Ontario: the London Fibromyalgia Epidemiology Study. Arthritis Rheum. 1999;42(1):76-83.
Physical Therapy Experience
Asking about the patient's physical therapy experience.
Doing the Physical Examination Part 1
Dr. Bernstein conducts a cursory examination of Sarah’s range of motion, muscle strength and reflexes.
Doing the Physical Examination Part 2
Sarah has taken Dr. Bernstein's referral to see a physical therapist. She meets with physical therapist Mike Schneider who takes a closer look at the pain she is experiencing.

