Harold's Pain
Harold's physician reviews his Brief Pain Inventory to assess the severity of his pain.
Harold's Brief Pain Inventory (Short Form)
1. Throughout our lives, most of us have had pain from time to time (such as minor headaches, sprains, and toothaches). Have you had pain other than these everyday kinds of pain today?
Yes
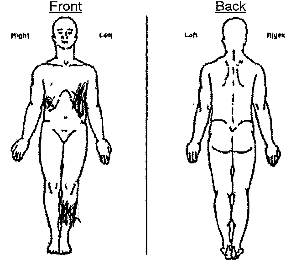
2. On the diagram, shade in the areas where you feel pain. Put an "X" on the area that hurts the most.
3. Please rate your pain by marking the box beside the number that best describes your pain at its worst in the last 24 hours. (Harold's score is listed below.)
From 0 (no pain) to 10 (pain as bad as you can imagine), Harold lists his pain at its worst in the last 24 hours as a 7.
4. Please rate your pain by marking the box beside the number that best describes your pain at its least in the last 24 hours. (Harold's score is listed below.)
From 0 (no pain) to 10 (pain as bad as you can imagine), Harold lists his pain at its least in the last 24 hours as a 4.
5. Please rate your pain by marking the box beside the number that best describes your pain on the average. (Harold's score is listed below.)
From 0 (no pain) to 10 (pain as bad as you can imagine), Harold lists his average pain in the last 24 hours as a 4.
6. Please rate your pain by marking the box beside the number that best describes your pain right now. (Harold's score is listed below.)
From 0 (no pain) to 10 (pain as bad as you can imagine), Harold lists his pain right now as a 4.
7. What treatment or medications are you receiving for your pain?
- Naproxen
- Acetaminophen
- Gabapentin
- Suboxone®
8. In the last 24 hours, how much relief have pain treatment or medications provided? Please mark the box with the percentage that most shows how much relief you have received.
From 0% (no relief) to 100% (complete relief), Harold says he received 70% relief from his pain from pain treatment/medications.
9. Mark the box beside the number that describes how, during the past 24 hours, pain has interfered with your:
A. General Activity:
From 0 (does not interfere) to 10 (completely interferes), Harold rates his pain as interfering with his general activity as a 4.
B. Mood:
From 0 (does not interfere) to 10 (completely interferes), Harold rates his pain as interfering with his mood as a 4.
C. Walking Ability:
From 0 (does not interfere) to 10 (completely interferes), Harold rates his pain as interfering with his walking ability as a 3.
D. Normal Work (includes both work outside the home and housework):
From 0 (does not interfere) to 10 (completely interferes), Harold rates his pain as interfering with his normal work as a 4.
E. Relations with other people:
From 0 (does not interfere) to 10 (completely interferes), Harold rates his pain as interfering with his relations with other people as a 2.
F. Sleep:
From 0 (does not interfere) to 10 (completely interferes), Harold rates his pain as interfering with his sleep as a 4.
G. Enjoyment of life:
From 0 (does not interfere) to 10 (completely interferes), Harold rates his pain as interfering with his enjoyment of life as a 4.
Copyright 1991 Charles S. Cleeland, PhD, Pain Research Group, All rights reserved.
Harold's Follow-Up Pain in His Own Words
As the doctor examines him, Harold experiences residual pain from his injuries.
Harold's Follow-Up Opioid Use Disorder
The doctor checks with Harold to see how he's handling his opioid use disorder in the face of residual pain.
Urine Drug Monitoring
Baseline
- Definitive testing at baseline for patients prescribed opioids for chronic pain unless presumptive testing is required by institution or payer policy
- A rational approach to choosing the most relevant substances to analyze is recommended
Risk Assessment
- Obtain relevant patient history
- Use validated tools to assess risk for aberrant medication-taking behavior, opioid misuse, opioid use disorder, and potential respiratory depression/overdose
- Check PDMP (Prescription Drug Monitoring Program) and previous UDM (Urine Drug Monitoring) results
- Evaluate behaviors indicative of risk
Risk Level
- Low Risk: UDM at least annually
- Moderate Risk: UDM greater or equal to 2 times per year
- High Risk: UDM greater than or equal to 4 times per year
Reference:
Adapted from "Rational Urine Drug Monitoring in Patients Receiving Opioids for Chronic Pain: Consensus Recommendations," by Charles E. Argoff, MD et al., 2018, American Academy of Pain Medicine, 19,p.102. Adapted with permission.
Harold's Discharge
Pharmacotherapy
The following discusses appropriate pharmacotherapy for Harold's emergency pain management:
Buprenorphine
Harold should receive buprenorphine/suboxone (Suboxone®). With Harold's history of opioid use disorder (OUD), buprenorphine/naloxone, would be most appropriate because it is used for opioid detoxification or maintenance treatment of OUD, and can be used to treat pain.
Acetaminophen
Harold should receive acetaminophen. Acetaminophen is a nonopioid analgesic that can be used as part of multimodal analgesia, and is not known to cause physical dependence.
Regional anesthesia
Harold could receive an ankle block to allow for early mobilization with assisted devices to prevent further injury. A block using bupivacaine could last approximately 18 hours. See below for more.
Oxycodone
Harold should not receive oxycodone because this was his drug of choice for his opioid use disorder. In Harold's case, we want to minimize his exposure to complete agonist opioids such as oxycodone. Oxycodone will not be effective in the presence of buprenorphine/naloxone (Suboxone®), which Harold is taking, because full agonists are antagonized by the use of partial agonists-antagonists.
Codeine
Codeine is not the best choice for acute pain. It has variable metabolism, which creates unpredictable efficacy and is a weak synthetic opioid with little to no benefit to patients like Harold. Learn more about codeine.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Harold should receive NSAIDs. Because of his history with OUD, NSAIDs can be used as part of multimodal analgesia to reduce requirements for opioids.
Adjuvant drugs
Harold should receive adjuvant analgesics such as anti-convulsant medications as part of multimodal analgesia or antidepressants. Gabapentin is a commonly used anti-convulsant medicaton to treat pain. Alternatives include pregabalin, duloxetine, tricyclic anti-depressants (e.g., amitriptyline).
Tramadol
Harold should not receive tramadol. It is a weak mu opioid agonist for management of mild to moderate acute and chronic pain and should be avoided because of variable metabolism. It also has other serotonergic pathways. Because tramadol can lead to dependence, it should be avoided in patients with a history of substance use disorder.
Reference:
Dever C. Treating acute pain in the opiate-dependent patient. J Trauma Nurs. 2017;24(5):292-299. CDC Guideline for Prescribing Opioids for Chronic Pain | Drug Overdose | CDC Injury Center. cdc.gov. https://www.cdc.gov/drugoverdose/prescribing/guideline.html. Published 2018. Accessed July 26, 2018. Sporer KA. Buprenorphine: A primer for emergency physicians. Ann Emerg Med. 2004;43(5):580-584. Ahmadi A, et al. Pain management in trauma: A review study. J Inj Violence Res. 2016;8(2)89-98. Chou R, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2)113-130.
Harold's Pharmacotherapy Plan
Harold's new pharmacotherapy plan developed at his follow-up visit includes:
- Naproxen: 440 mg every 12 hours
- Acetaminophen: 650 mg every 4 to 6 hours as needed
- Buprenorphine/Naloxone (Suboxone®): 8 mg/2mg twice daily
- Gabapentin 600mg 3 times daily
- Continue physical therapy (PT)
Reference: Jamison RN, Edwards RR. Risk Factor Assessment for Problematic Use of Opioid for Chronic Pain. Clin Neuropsychol. 2012 Aug 30 https://www.ncbi.nlm.nih.gov/pubmed?term=22935011.
Behavioral Therapy
The following explains whether different behavioral therapy options are best suited for Harold.
Initiate psychological treatment
It is important to provide consistent outpatient psychological therapy to assist Harold in accepting and coping with his opioid use disorder as well as tolerating pain and its physical and emotional effects without using opioids.
Include Harold's wife in counseling sessions
Opioid Use Disorder (OUD) can disrupt a person's social and domestic environment. Harold and his wife experienced marital discord from Harold's OUD. It would be beneficial for Harold's wife, Janice, to join Harold's individual counseling sessions to show her support for his recovery.
Focus on Cognitive Behavioral Therapy (CBT)
CBT combines operant learning, cognitive and emotional strategies, and builds skills to deal with pain and its impact on biopsychosocial well-being. CBT will help Harold control his chronic pain and opioid use disorder by changing his thoughts.
Incorporate Motivational Interviewing
Motivational Interviewing (MI) could be beneficial for Harold as MI is based on principles of motivational psychology meant to enhance motivation for change. Harold was willing to seek treatment when given an ultimatum by his wife. MI can motivate Harold to make behavioral changes for himself rather than for others. MI is most effective when combined with other evidenced-based changes.
Provide educational materials and instructions on relaxation therapies
Relaxation therapies such as progressive relaxation, guided imagery, biofeedback, self-hypnosis, and deep-breathing exercises can be effective self-management techniques to reduce pain.
Emphasize counseling over medication use
A combination of medication treatment and counseling, an evidence-based practice is called medication-assisted treatment (MAT), MAT is treatment with buprenorphine or methadone in combination with behavioral therapies.
Risk Reduction
The following covers how different risk reductions might impact Harold.
Provide routine urine drug screening a minimum of three times per year
Because of Harold's opioid use disorder, he should receive urine drug monitoring (UDM) as part of a comprehensive risk monitoring. Harold is considered high risk, therefore, it is recommended he receive UDM at least three times per year when stable and up to monthly if needed to discourage relapse.
Admit Harold for inpatient treatment of opioid use disorder
Although Harold previously met the DSM V criteria for severe opioid use disorder, he was already treated inpatient several months ago following an opioid overdose. Harold was placed on buprenorphine/naloxone (Suboxone®) before being discharged from the hospital for his motor vehicle crash, and he does not require the need for abrupt inpatient detoxification. He should continue to follow-up with his doctor as requested and report any cravings he experiences.
Request regular office visits (at least once per six months)
Harold should plan to see his doctor on a regular basis as he heals from his motor vehicle crash and recovers from the pain. Patients who are at higher risk of opioid are encouraged to seek regular office visits for the physician to examine the patient's treatment propose alternative treatments if current treatment is insufficient, detect any side effects and assess for opioid misuse.
Restrict opioid refills (one or fewer opioid refills more than one week early)
Harold was reintroduced to buprenorphine/naloxone (Suboxone®) to treat his opioid use disorder and provide pain relief prior to his discharge from the hospital and should not receive any other opioids because of his history of opioid use disorder.
References
Argoff CE, et al. Rational urine drug monitoring in patients receiving opioids for chronic pain: Consensus recommendations. Pain Med. 2018;19(1):97-117. Starrels JL, et al. Low use of opioid risk reduction strategies in primary care even for high risk patients with chronic pain. J Gen Intern Med. 2011;26(9):958-964.

