Physical Exam
Vital Signs
Temperature 97.2, Blood Pressure 112/68, Heart Rate 80, Respirations 20
Ht/Wt
69 inches, 318 lbs
General appearance
Morbidly obese man, in distress, winces and supports lower back with his hands.
HEENT
Normocephalic, sclera anicteric, PERRLA, eye movement conjugate , no nystagmus, conjunctivae pink, oral mucosa moist and pink, oropharynx clear, tongue midline and mobile. Teeth are present and in good repair. Good neck range of motion, palpable thyroid without nodules, no cervical lymphadenopathy. Ear canals clear with minimal cerumen; ear drum visible and without redness. No pain with palpation or tragus or manipulation of auricle.
Lungs
Clear to auscultation
Heart
Normal sinus rhythm, no murmurs
Abdomen
Very round, BS + x 4 quadrants, soft to palpation and without masses, mild tenderness noted over epigastric region, no other point tenderness or referred pain.
Extremities
No cyanosis or clubbing, bilat lower legs with ruborous edema, +2-+3 pitting over dorsal feet. Scars on both legs from surgeries.
Skin
Warm, smooth and dry. Without diaphoresis or rashes.
Musculoskeletal
Reduced ROM of back, limited by pain in lower lumbar region with flexion and extension. Straight leg raise testing is negative to 50 degrees elevation, limited by pain in knees. There is increased tone in the lumbar paraspinal muscles diffusely but no focal tenderness. Crepitus is present in the right knee. ROM of the knees is limited by pain.
Neurological
Alert and oriented x 3, Folstein MMSE = 25/30. Able to accurately draw a clock with hands set at a time of 3:40. Cranial nerves intact with exception of absence of lateral peripheral vision since occipital lobe stroke, Grip strength good and equal bilaterally. Leg strength 5/5 proximally and distally. Sensation is intact to light touch, sharp, position and vibration in arms or legs. Reflexes are ++ at biceps, triceps, patellae and ankles. Both toes are downgoing. Gait is slightly unsteady with wide base of support and reduced step height.
Lab Results
Hematology
- RBC: 4.5
- HgB: 14.8
- HCT: 47
- Plat: 185
- WBC: 7.9
Chemistry
- Fasting Glucose: 99
- T4: 7
- T7: 0.9
- TSH: 3.2
- Na: 140
- K: 4.1
- Cl: 100
- BUN: 18
- Creat: 1.1
- Bili Direct: 0.1
- Bili Tot: 0.4
- AST: 15
- ALT: 22
- Alk Phos: 83
Imaging Studies
MRI
A mid-sagittal MRI of the lumbar spine shows that there has been a spontaneous fusion of L4 and L5 (suggestive of chronic damage), advanced degeneration of the L5-S1 disc, disc bulging at L3-L4 and L2-L3 as well as ligamentous hypertrophy and some degree of spinal stenosis. This appearance is illustrative of degenerative changes that may be observed in patients with long-standing back pain and degenerative disc disease.

The relevance of MRI for assessing back pain that presents with neurological deficits or other worrisome symptoms is illustrated in this slide. This was an 82 year old man with known prostatic adenocarcinoma who presented with a long history of low back pain that had worsened over the last 2 weeks. He arrived to the emergency room with acute urinary retention and leg weakness. The MRI showed metastatic disease (star) superimposed on degenerative changes to the lumbosacral spine, the metastatic disease resulted in nerve root compression and a cauda equina syndrome (urinary retention, leg weakness in the sciatic distribution, and pain). Other causes may include infection, trauma and inflammatory disease.

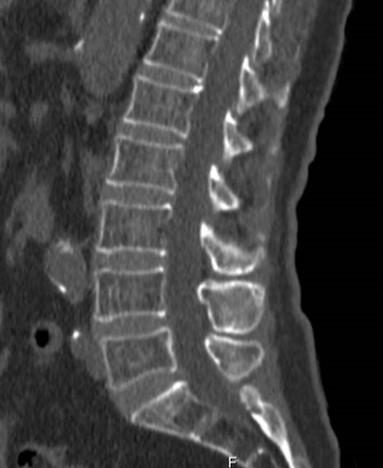
CT
Another imaging modality useful for assessing patients who have back pain with neurological deficits (or other worrisome symptoms) is CT. In this spine CT of an 82 year old woman with sudden onset myelopathy (pain, weakness and loss of sphincter control), there is relative preservation of disc morphology, spinal alignment and vertebral structures (normal for age). There is a degree of osteoporosis. Myelitis was subsequently diagnosed on MRI.
The importance of ordering the correct study is highlighted in this lumbar spine CT. This patient had severe low back pain after a fall. The lumbar spine structures are essentially normal, however there is bulging of the L5-S1 disc and a fracture of the S1 vertebral body visualized at the lower boundary of the CT window (star). Information such as this is helpful in prognosticating recovery for the patient and for anticipating the need for stronger pain medication such as might be required after vertebral fracture. In short, ‘low back pain’ can arise from structures in the sacrum and pelvis, it is important to make sure that the ordered study addresses the suspected problem.

Pain Assessment, Continued
How pain impacts Mr. Monahan’s usual daily activities:
- Does pain impact your ability to care for your own needs (shower, shave, get dressed, walk) ?
- Does pain impact your ability to do household chores (walk up and down stairs, home maintenance, yard work)?
- Does pain impact your relationships (wife, family, neighbors, acquaintances)?
- Does pain impact your ability to enjoy your life?
- Does pain impact your ability to sleep?
What are Mr. Monahan’s goals for pain treatment?
Pain’s Impact on Ability to Care for Self Needs
Sometimes Mr. Monahan's wife has to help him with personal hygiene, getting clothes out for him, otherwise he is able to attend to his own needs.
“Most of the time I am able to things for myself. I move slower, but that’s what happens when you get old. It really gets me down when Joan has to help me. I just can’t do things for myself anymore like I used to. Sometimes I don’t feel good enough to shower until 3 or 4 in the afternoon. That Tramadol really binds me up.”
Pain’s Impact on Ability to do Household Chores
Is able to mow the lawn, clear the snow from the driveway, feed and water their pony.
“I mow half of the lawn 1 day and the other half the next day. Our yard is bumpy so riding the lawn tractor jars my back.” “I can carry a pail of water to Buster [the pony]. I do better carrying heavy loads at my side, instead of in front of me. I can’t help Joan out with the vacuuming. I used to vacuum the carpet for her, it hurts my back too much. I try to help her make the bed, but it hurts my back to bend over and grab the sheet.” Mr. Monahan starts to cry.
Pain’s Impact on Relationships
Mr. Monahan denies that pain has impacted his relationships. Wife and children are supportive, and a grandson helps out with chores when Mr. Monahan is having problems with mobility.
Mrs. Monahan states “He gets grouchy and yells when his back hurts. I just go in the bedroom and watch TV,” she looks over at Mr. Monahan and says, “Pat, you know you get grouchy. You aren’t fun to be around.”
Pain’s Impact on Ability to Enjoy Life
Reports that his two closest friends are deceased. Reports has never had hobbies. Is happiest when his wife is with him and their children are home to visit.
“I used to play a lot of sports and I would run a lap around the farm every morning. We have 40 acres. I don’t have hobbies, other than the ponies. When the kids were little we did a lot with the ponies. Joan and I like to sit on the swing and talk. We go out to eat, or over to see her sister or my sister, or visit our kids. Our daughter takes us on vacations, sometimes my back hurts too much to get out and sightsee, but Joan is able to. I feel like a burden to everyone.” Mr. Monahan starts to cry.
Pain’s Impact on Ability to Sleep
Reports that he has problems sleep, sometimes due to pain, mostly due to other stress. Indicates that pain is worse on days after a poor night of sleep.
“Some nights my back hurts so much that I can’t get comfortable in bed. When that happens, I go out to my chair and watch TV. I always wear my headphones so I don’t wake up Joan. I usually fall asleep in my chair. My back and knees are worse after I haven’t slept good. And I have a harder time getting up and around the next day. I spend more time in my chair."

