Patient-Centered Medical Home (PCMH) Definition
- The provision of comprehensive, multidisciplinary primary care to a group of patients on an on-going basis.
- Focuses on the management of chronic illness,
- improving patient outcomes and lowering health care costs through evidence-based guidelines and health information technology.
- Emphasizes the monitoring, evaluation, reporting
- and improvement of the quality of care and patient outcomes.
Why the PCMH?
Early evidence shows it may meet the Triple Aim for improving health care by:
- Producing better patient outcomes
- Facilitating superior health care (and provider satisfaction)
- Reduce health care costs
For early results of evaluations of the PCMH, see:
https://pcmh.ahrq.gov/page/defining-pcmh
For more about the Triple Aim, see: www.IHI.org
Training For the PCMH
Medical, dental, nursing, pharmacy and other health professional schools are adopting new accreditation standards requiring their students to train with students in other health professional degree programs, so they may build skills in working on interdisciplinary teams.
See: AACN (2011) Core Competencies for Interprofessional Collaborative Practice
Accessed at: https://www.aacom.org/docs/default-source/insideome/ccrpt05-10-11.pdf?sfvrsn=77937f97_2
PCMH Resource Center
For guidance on designing, implementing, or evaluating your own PCMH, see the PCMH Resource Center at the Agency for Healthcare Research and Quality website:
http://www.pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483
Health Care Using the Biopsychosocial Approach
- Systematically consider biological, psychological, and social factors and their complex interactions in understanding health, illness, and health care delivery.
- Recognize that relationships are central to providing health care
- Use self-awareness as a diagnostic/therapeutic tool
- Elicit the patient’s history in the context of life circumstances
- Decide which aspects of biological, psychological, and social domains are most important to the patient’s health
- Provide multidimensional treatment
Reference
Engel, GL. The need for a new medical model: A challenge for biomedicine. Science 1977; 196:129-136.
RN Role in the Patient - Centered Medical Home Model
- Assists the provider on collection of pertinent history, diagnostic studies and ongoing re-assessment of patient status (e.g., INR levels, Hgb A1c, pain, HTN)
- Establishes a relationship with patient to promote more healthy choices with identified goals of care
- Identifies health maintenance goals with the patient included as an active team member
- Assists in coordinating education and community resources to support the patient in meeting health care goals
- Assists the medical team, including patient, with re-assessment of treatment goals
Role of a Pharmacist in the Medical Home
- Advise patients, physicians, and other health practitioners on the selection, dosages, interactions, and side effects of medications.
- Monitor patients’ health and progress to ensure that they are using their medications safely and effectively.
When to Make a Referral to a Mental Health Professional
- Any chronic problem
- Patient’s request
- You can not meet the patient’s needs for time and attention
- Further assessment or consultation necessary
- Frustration
- Problem has been present for over one year with little improvement yet
- Patient requesting to learn pain management techniques
Principles of Pain Processing
Learning Objectives
- Describe the anatomy and physiology associated with normal sensory transmission
- Define terms commonly associated abnormal pain states (ex. hyperalgesia, allodynia)
- Describe the difference between acute and chronic pain
- Classify pain syndromes (i.e.. nociceptive, neuropathic and inflammatory)
Pain: Definition
“An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.” (IASP)
Additional definitions can be found at the International Association for the Study of Pain (IASP) https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698
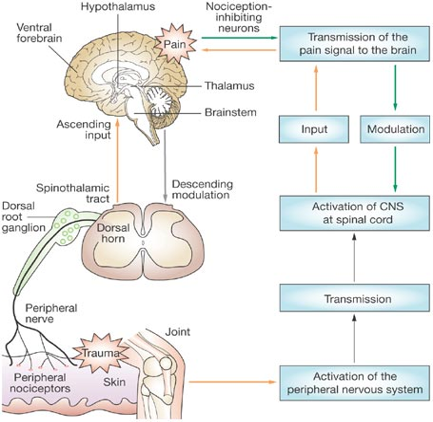
Pain Processing
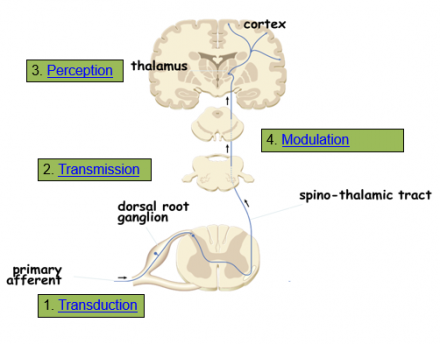
Transduction
- Nociceptors (free nerve endings) of Aδ and C fibers are exposed to noxious stimuli
- Noxious stimuli include:
- mechanical (pressure, swelling, incision)
- thermal (burn, scald)
- chemical (neurotransmitters, toxic substance, ischemia, infection)
- Chemical messengers released by damaged cells may be targets for pharmacotherapy
- bradykinin
- serotonin
- substance P
- Prostaglandins
- Chemical messengers may also sensitize nociceptors
Transmission
- Begins at the site of transduction traveling along the nociceptor fibers to the dorsal horn in the spinal cord
- Aδ and C fibers terminate in the dorsal horn
- Excitatory neurotransmitters are released propagating the signal from the spinal cord to the brain
- The pain impulse is transmitted from the spinal cord to the brain stem and thalamus via the ascending pathways
- The brain does not have a discrete pain center, so the impulse is processed at the thalamus and then directed to additional brain regions
Perception
- Pain becomes a conscious multidimensional experience
- Activation of multiple cortical regions
- The reticular system:
- responsible for the autonomic and motor response to pain (i.e. quickly removing a hand when it touches a hot stove)
- Somatosensory cortex:
- important for the interpretation of pain information being processed
- identifies the intensity, type and location of the pain sensation and relates the sensation to past memories and experiences
- Limbic system:
- responsible for the emotional and behavioral responses to pain
Modulation
- Beginning at the brain, the descending pain pathway utilizes inhibitory signals to block the pain signal from being processed in the spinal cord
- Descending inhibition involves the release of inhibitory neurotransmitters that produce analgesia
- Inhibitory neurotransmitters involved with the modulation of pain include:
- endogenous opioids, serotonin, norepinephirine, GABA
- Analgesics commonly used in the treatment of pain may produce their pharmacological actions through these neurotransmitter pathways
Descending Modulation
Additional resources on nociception:
http://www.jci.org/articles/view/42843
http://www.nature.com/nrrheum/journal/v5/n1/fig_tab/ncprheum0972_F1.html#figure-title
Pain Categories
Nociceptive Pain
- Nociceptive Pain: Pain that arises from actual or threatened damage to non-neural tissue and is due to the activation of nociceptors.
- Can be divided in to:
- Somatic
- Visceral
Somatic
Pain arising from tissues such as skin, muscle, tendon, joint and bone. Well localized.
Visceral
Pain arising from the internal organs. Often diffuse or referred.
Neuropathic
- Pain caused by a lesion or disease of the somatosensory nervous system.
- Neuropathic pain is a clinical description and not a diagnosis.
- Patients may describe the pain as burning, electric, searing, tingling, and migrating or traveling.
- Some causes of neuropathic pain include
- Amputation (phantom limb pain), herpes zoster, AIDS (peripheral neuropathy), diabetic neuropathy, fibromyalgia, and cancers that affect the spinal cord, among others.
Terms Associated with Neuropathic Pain
- Hyperalgesia
- Increased pain from a stimulus that normally provokes pain.
- Allodynia
- Pain due to a stimulus that does not normally provoke pain.
- Sensitization
- Increased responsiveness of nociceptive neurons to their normal input, and/or recruitment of a response to normally sub-threshold inputs.
Inflammatory Pain
- A localized protective reaction of tissue to irritation, injury, or infection, characterized by pain, redness, swelling, and sometimes loss of function.
- Activates the nociceptive pathway.
- Examples of inflammatory pain include:
- Appendicitis, rheumatoid arthritis and inflammatory bowel disease.
Time Course of Pain
- Acute
- Typically does not last longer than three to six months, and resolves when the underlying cause of pain has been treated or has healed.
- Chronic
- Persists despite the fact that the injury has healed. Pain signals persist beyond three to six months and can last for years.
Components of a Comprehensive Pain Assessment
- Pain History (e.g., OLD CART + P)
- Medical / Surgical / Psychosocial History
- Physical Exam and Mental Status assessment
- Classify pain, determine extent of disease, identify support systems -- Pain Diagnosis
- Obtain appropriate laboratory and imaging studies
- Determine therapies for organic component and for affective and cognitive components of pain
Assessment of Pain Using the OLD CART+P Model
- Onset
- Location
- Duration
- Characteristics - Quality/Intensity
- Aggravating factors/Associated symptoms
- Relieving factors
- Treatments Tried
- Perception
Onset
- When did it start?
- Associated with a trauma, surgery or ‘just came on?
Location
- Where is the pain?
- Is this the same pain they usually have, or a new problem?
Duration
- Is it constant?
- Intermittent? If intermittent what is the frequency & how long does it last?
Characteristics
- Quality/Intensity
- What does the pain feels like?
- Aching, cramping, burning, shooting throbbing, pressure, electric shock, numbing, gnawing, deep aching, hot itching, squeezing stabbing, tingling
Intensity
- Numeric Pain scale
- 0 = no pain, 10 = worst pain possible
- (1-3 mild, 4-7 moderate, 8-10 severe intensity)
- Pain now
- On average in past week
- Least pain in past week
- Worst pain in past week
Aggravating Factors/Associated Sx
- What makes the pain worse?
- Bending, lifting, twisting
- Eating, light, loud noises
- weather changes, stress
- walking, touching area
- Is there any fever? Chills? Nausea? Loss of mobility?
Relieving Factors
- What makes the pain better?
- Rest, heat, ice, medications
- dark room, movement
- eating/not eating
- If patient responds, “Nothing” -- then explore what methods they have tried
Treatments Tried
- Explore what the patient has tried to this point to relieve this pain
- Include what treatments have worked in the past for similar experience
Patient's Perception
- Impact of pain on Quality of Life
- mood
- relationships
- sleep
- functional level
- appetite
- activity
- work
- What are their thoughts regarding the pain?
- How is it impacting their life?
- Use a Functional Capacity Questionnaire to obtain baseline function and intermittently measure changes with your interventions
Other Commonly Used Assessment Tools
- Faces Scales
- Categorical Scales
- (e.g., none mild moderate severe)
- See the reviews below for a more comprehensive discussion of the many options for pain assessment available.
www.nursingtimes.net/nursing.../pain.../assessment...pain/1861174.article
http://pain-topics.org/clinical_concepts/assess.php
Opioid Allergy Versus Intolerance
Many Patients Have an Initial Reaction to Opioids
- Nausea and sometimes vomiting are symptoms experienced by many patients who have not been taking opioids.
- Tolerance develops within a few days to the nausea and vomiting effects associated with opioid use.
- These symptoms are NOT due to an opioid allergy. Patients often state that they have an opioid allergy if they have experienced nausea and vomiting in the past after the administration of an opioid.
- Opioid allergies are rare.
- Medication History
- Determine reaction to listed “allergies” and time reaction occurred relative to dose
- N/V, constipation, sedation, mental status changes, etc. are adverse effects
- Able to prophylaxis patient
- Side effects that mimic immune reaction
- Mild pruritis, uticaria, bronchospasm, mild hypotension
- May or may not occur if rechallenged
Reference
Woodall HE, Chiu A, Weissman DE. Opioid Allergic Reactions #175. J Palliat Med. 2008;11(5):776-77.
Opioid Allergy
- Immune-mediated reactions
- Allergic dermatitis
- Possible Type IV hypersensitivity reaction
- Confirm with dermatologist or allergist
- Allergic dermatitis
- Anaphylaxis: IgE mediated
- Anaphylactoid reactions: NOT IgE mediated
- Clinically appear the same
- Rare
- Symptoms anaphylaxis/anaphylactoid reactions
- Early: nasal congestion, flushing, pruritus, angioedema
- Late: nausea, diarrhea, urinary urgency, brochospasm, hypotension, death
Opioid Allergy Treatment
- Acute anaphylaxis/anaphylactoid reaction: epinephrine, antihistamine, corticosteroid
- If patient requires continued opioid use
- Collaborate with dermatologist or allergist for desensitization
- Rotate to a different opioid class
- Close patient monitoring
- Prophylaxis with antihistamine and/or corticosteroid
Efficacy of Over the Counter (OTC) Pain Medications
Topical Counterirritants
- Paradoxical effect
- Produce less severe pain to counter a more intense one
- Alter pain perception
- Includes topical salicylates, capsicum, camphor, menthol, methyl nicotinate
- Large variety of commercially available strengths and combination products
- Methyl salicylate
- Vasodilation with resultant hyperemia
- Avoid in children, ASA sensitivity, severe asthma
- Camphor, menthol
- Simulates nerves to perceive cold and depresses nerves that perceive pain
- Avoid camphor in children
Most common counterirritants with varying ingredient combinations and concentrations.
- Methyl nicotinate
- Vasodilation and increased skin temperature
- Decreased response with concurrent NSAID or ASA use
- Capsicum
- Initial sensation of warmth/burning pain with application
- Tachyphylaxis
- Depletes substance P
- Delayed pain relief
- Do not touch mucous membranes after application
Capsicum: cream or topical patches
Tachyphylaxis: Rapid appearance of progressive decrease in response to a given dose after repetitive administration of a pharmacologically or physiologically active substance
Topical Salicylate Efficacy
- BMJ systematic review for efficacy in acute and chronic pain (see reference below)
- Decrease pain by 50% compared to placebo
- Trials limited by small size, inadequate design, validity, and different product compositions
- May be effective in acute pain (< 7 days)
- NNT: 2.1 (95% CI: 1.7-2.8)
- Moderate-poor efficacy in chronic pain (< 14 days)
- NNT: 5.3 (95% CI: 3.6-10.2)
Reference
Mason L, Moore RA, Edwards JE, McQuay HJ, Derry S, Wiffen PJ. Systematic review of efficacy of topical rubefacients containing salicylates for the treatment of acute and chronic pain. BMJ. 2004;328:995–7.
2012 FDA Drug Safety Communication
- Alert regarding rare cases of first-third degree chemical burns at topical counterirritants application site
- May occur after first application
- Severe pain, swelling, or blistering within 24 hrs
- More common with menthol or menthol/methyl salicylate combination products than capsaicin
- Menthol concentrations > 3%
- Methyl salicylate concentrations > 10%
- No warnings added to product packaging presently
Patient Education
- Patients should seek medical attention immediately for any severe burning, swelling, or blistering with topical counterirritant use
- Do not bandage or apply local heat to areas of topical counterirritants application
- Further increases risk of chemical burns
- Do not apply topical counterirritants to open or irritated skin, eyes, or mucosal membranes
Glucosamine and Chondroitin
- Glucosamine
- An aminomonosaccharide used in the biosynthesis of proteoglycans and glycosaminoglycans
- Chondroitin sulfate
- Proposed to provide a substrate for the formation of a healthy joint matrix and to inhibit enzymes responsible for metabolizing cartilage
- Lack of clinically significant efficacy in studies
- Should not continue, if patients have not experienced benefit
- Not recommended knee and hip osteoarthritis by 2012 ACR guidelines
- slower loss of cartilage compared to placebo in knees of OA pts
- should use the sulfate salt of glucosamine as opposed to the HCl salt…nearly all positive efficacy studies use the better-absorbed sulfate salt
- SEs: gas, bloating, cramps, nausea
- it has mild anti-inflammatory props, similar to using OTC Advil
- Glucosamine reduces joint narrowing and cartilage loss;
- Conflicting results on this with poor quality studies…..if this was the case, all younger individuals presenting with OA would be placed on this and never develop OA
- chondroitin effects are mixed and may increase risk of SE
- Glucosamine promotes the synthesis of glycosaminoglycans
- Decreased in cartilage and ECM in OA patients
- Dosing
- Glucosamine 500mg TID; chondroitin 1200mg/day
- CI: Hypersensitivity to shellfish
- Safety similar to placebo
- GI events most common, but are infrequent
- Low adverse effect treatment burden
- Contraindication: Hypersensitivity to shellfish/shark
Medication Safety in Older Adults
A focus on the 2012 Beers Criteria.
Definitions
- Adverse drug reaction (ADR)
- A specific reaction usually related to a medication’s pharmacology
- Adverse drug event (ADE)
- Injury due to a medication
- May include ADR and events related to medication use
- Medication error
- Inappropriate medication use that may or may not result in harm
Reference
Nebeker JR, Barach P, Samore MH. Clarifying adverse drug events: a clinician's guide to terminology, documentation, and reporting. Ann Intern Med 2004;140:795-801
ADE - Risk Factors
- Increasing age
- Female gender
- Hx prior ADR
- Prolonged hospitalization
- Fragmented medical care
- Multiple disease states/poor health status
- Polypharmacy
ADE in Older Adults
- Most ADEs in older adults are preventable
- 27% in primary care
- 42% in long-term care
- Lead to poor outcomes
- Often occur with medication ordering and monitoring
- Influenced the development of potentially inappropriate medication (PIM) lists
Beers Criteria
- Most commonly used tool to avoid prescribing potentially inappropriate medication (PIM)
- Outlines clinical exceptions among the drugs to avoid
- Developed for use in ambulatory and institutional settings
- Recommendations compiled by geriatric panel
Reference
American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults J Am Geriatr Soc 2012;60(4):616-31
Beers Criteria Medication Categories
- Inappropriate medications for all older adults
- Inappropriate medications to avoid in older adults with selected disease states
- Medications that should be used cautiously in older adults
Beers List Pain Medications Inappropriate for All Older Adults
- Tricyclic Antidepressants (TCAs)
- Increased potential for anticholinergic effects
- Meperidine
- Increased potential for neurotoxicity
- Pentazocine
- Increased potential for confusion and hallucinations
- NSAIDs
- Increased potential for GI bleeding, acute kidney injury (AKI), and cardiovascular AEs
- Skeletal muscle relaxants
- Increased potential for anticholinergic effects and fractures
NSAID Adverse Effects
- N/V
- Dyspepsia
- Myocardial infarction
- CVA
- HTN
- Heart failure
- Acute kidney injury
- GI bleeding
- Anemia
- Bronchospasm
- Hepatic failure
Anticholinergic Adverse Effects
- Cardiac arrhythmias
- Cognitive impairment
- Falls
- Orthostatic hypotension
- Sedation
- Dizziness
- Constipation
- Urinary retention
- Thermoregulatory impairment
- Xerostomia
- Dry eyes
- Delirium/agitation
Beers List Pain Medications Inappropriate for Selected Older Adults
| Condition | Avoid |
|---|---|
| Seizures | Tramadol |
| Delirium | TCAs, corticosteroids, meperidine |
| Dementia | TCAs |
| Falls | TCAs, Anticonvulsants |
| Gastric or duodenal ulcers | NSAIDs |
| Chronic kidney disease | NSAIDs |
| Heart failure | NSAIDs |
Beers List Pain Medications to Be Used with Caution in Older Adults
- Carbamazepine, TCAs, and SNRIs
- Increased potential for Syndrome of Inappropriate Antidiuretic Hormone (SIADH) or hyponatremia
- Need to closely monitor sodium when initiating a medication or changing doses
Acetaminophen Updates
Acetaminophen Public Health Concerns
- Primary cause of acute hepatic failure in US
- Narrow therapeutic index
- Ceiling effect
- Risk of unintentional overdose
- High risk patient populations
- Pre-existing liver disease, malnutrition, alcohol abuse
Reference
Ostapowicz G, et al. Results of a Prospective Study of Acute Liver Failure at 17 Tertiary Care Centers in the United States. Ann Intern Med. 2002;137:947-954.
Metabolism of Acetaminophen: Cause of Hepatic Toxicity
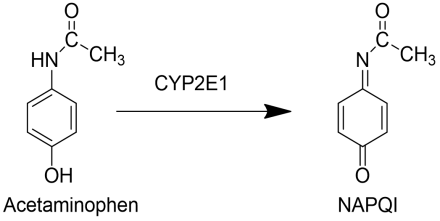
The Cytochrome P450 enzyme CYP2E1 is a bioactivation reaction that yields NAPQI, the metabolite responsible for the liver toxicity of acetaminophen.
Scope of Problem
- Lack of consumer understanding about potential liver injury
- Concurrent use of 2 acetaminophen containing products
- Potential harm from exceeding maximum daily dose
- Difficult to recognize onset of acute liver injury
- Some patient populations are more prone to liver injury
- Dose errors
- Different product concentrations
- Measuring dose incorrectly
- Incorrectly calculating weight based dose
- Large variety of acetaminophen containing over the counter (OTC) and prescription products
- Consumer failure to recognize active ingredients in combination products
- Prescription labels
- Abbreviations
- Maximum daily dose not listed
Acetaminophen Timeline
| Date | Action |
|---|---|
| 2004 |
FDA public education campaign to promote safe NSAID and acetaminophen use Letter to State Boards of Pharmacy |
| 2009 |
FDA Center for Drug Evaluation and Research (CDER) Acetaminophen Workgroup
|
| 2014 | Combination acetaminophen prescription products >325mg/dose to be removed from market over 3 years (January 2011 FDA action). No impact on acetaminophen containing OTC products |
http://www.fda.gov/Drugs/DrugSafety/ucm239821.htm
Actions to Ensure Patient Safety
- Patient Education
- Avoid concurrent use of >1 acetaminophen containing product
- Avoid alcohol
- Do not exceed maximum daily dose of OTC + prescription products
- Encourage patient questions
- Do not use abbreviation on prescription label
- Write out “acetaminophen”
- Include maximum daily dose on prescription label
- Dispense calibrated measuring devices if needed
- Patient should demonstrate measuring technique
- Patient education materials available from FDA
Opioid Tolerance and Dependence
Drug Tolerance
- Decreasing effectiveness of a drug when given over time to achieve the same physiological effect
- More opioid is needed to achieve the same level of analgesia
Developing Tolerance
- Tolerance develops more rapidly to drugs with low efficacy
- More receptors need to be activated to achieve a given physiological effect leading to a low receptor reserve
- With a high efficacy drug, fewer receptors need to be activated to produce the same physiological effect leaving a larger receptor reserve
Tolerance develops more rapidly than dependence.
Dependence
- Dependence
- Altered or adaptive physiological state produced by repeated administration of a substance, resetting homeostatic balance. Individuals in this adapted, physically dependent state require continued administration of the substance to maintain normal function.
- Physical dependence
- demonstrated through a withdrawal syndrome. Without withdrawing the drug or giving an antagonist, the degree of dependence is not known.
- Psychological dependence
- manifested by an intense craving for the drug.
Pharmacokinetics and Metabolism of Opioids
Absorption, Distribution, Metabolism, Excretion (ADME) of Drugs
Drugs are delivered to the body by different routes of administration.
- Pharmacokinetics includes:
- Absorption
- Distribution
- Metabolism
- Excretion
- Pharmacodynamics includes:
- Drug Target (Receptor)
- Mechanism of Action
- Drug Response
- Genes and gene variants can affect a drug’s response
Why is ADME important in the clinical use of drugs?
- Understanding the basic concepts of ADME is important because:
- ADME determines the onset, intensity, duration, and termination of drug action
- Drug metabolism is the major mechanism for termination of drug action
- Pharmacokinetic drug interactions can be associated with altered drug metabolism
- Idiosyncratic adverse drug events and drug-induced toxicity can affect drug metabolism
- In the future, ADME genotyping will be central to personalized medicine
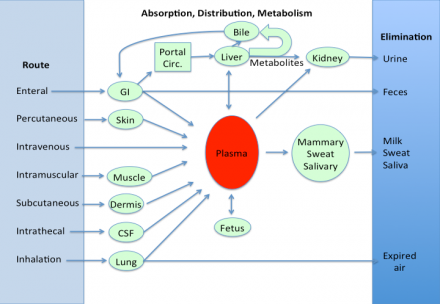
Factors Affecting Oral Absorption
- Disintegration of dosage form
- Dissolution of particles
- Chemical stability
- Resistance to enzymatic degradation
- Motility and mixing in GI tract
- Presence and type of food
- Passage across GI tract wall
- Blood flow to GI tract
- Gastric emptying time
Drug Metabolism (The Metabolic Fate of Drugs)
- Pharmacologic and clinical importance of drug metabolism:
- Major mechanism for the termination of drug action
- Basis of most pharmacokinetic drug interactions
- Activates prodrugs, such as tramadol
- May lead to the formation of toxic metabolites, (i.e., bioactivation, a major cause of drug and chemical toxicity) Acetaminophen is metabolized to a toxic compound
Prodrugs
Prodrugs are agents developed to improve the pharmacokinetic properties of drugs (e.g., enhanced intestinal absorption)
- Codeine is a prodrug for morphine. Codeine is demethylated by the liver enzyme cytochrome P450 to morphine.
- Tramadol is a prodrug that is metabolized to a compound that binds to opioid receptors.
Drug Metabolism
- The most important oxidative reactions are catalyzed by CYTOCHROMES P450 (CYPs), a family of enzymes in the liver.
- CYPs catalyze 75% of drug-metabolism reactions
- ~90% of CYP-catalyzed reactions involve 5 CYPs
- CYP -1A2, -2C9, -2C19, -2D6, and -3A4/5
Metabolism of Acetaminophen to a Toxic Metabolite
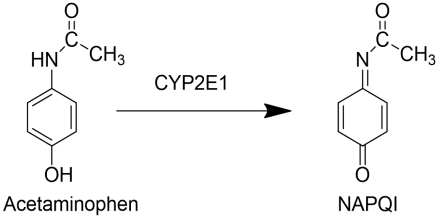
The Cytochrome P450 enzyme CYP2E1 is a bioactivation reaction that yields NAPQI, the metabolite responsible for the liver toxicity of acetaminophen.
Induction and Inhibition of CYPs
- Prescription/OTC medications and herbs (e.g., St. John’s Wort) can alter drug metabolism.
- Relevant to Mrs. Johsnon
- ethanol induces CYP2E1, an enzyme that metabolizes certain medications more rapidly if the patient has been drinking alcohol
- smoking will induce CYP1A2, so medications metabolized using this enzyme will be less effective
- Relevant to Mrs. Johsnon
ALWAYS ASK WHAT MEDICATIONS OR HERBS THE PATIENT IS TAKING
How Aging Affects Drug Metabolism
- Aging is associated with a ~40% reduction of blood flow to the liver and a similar reduction in liver mass. There is a greater chance of adverse drug reactions in the elderly.
- Our patient, at age 80, will metabolize many drugs more slowly than a younger patient.
For an excellent review on aging and geriatric clinical pharmacology: McLean AJ, LeCouteur DG, del Cabo R. Aging, Drugs, and Drug Metabolism. J Gerontol: A Biol Sci Med Sci. 2012 ; 67A(2):137–139.
Impact of Disabling Pain on Quality of Life
Loss of:
- independence & control
- role
- intimacy
- dreams of future
- friendships, partnership
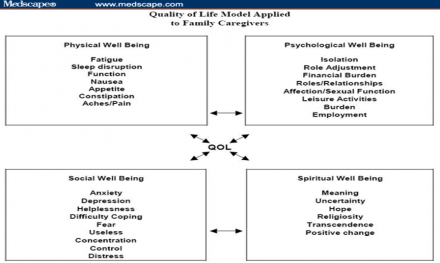
Quality of Life Model
How Do Nurses Help Patients/Families with their Struggles?
- We see it all… the front row seat to suffering:
- physical, emotional, spiritual
- The primary intervention we can do is to be.
- To be present with the patient /family
- To listen and facilitate
Most Common Sleep Disruptors
- Stress and pain
- Use of alcohol
- Exposure to light
- Use of caffeine
- Travel
- Exercising too close to bedtime
- Room conditions
- Rapid swings in blood sugar
- Obstructive sleep apnea
Sleep Deprivation Effects
- Strong association between sleep deprivation and obesity
- Impaired glucose tolerance
- Metabolic syndrome
- Changes in appetite hormones
- Changes in muscle and lean body mass
- Decreased concentration and longer response times
- Decreased memory
- Decreased ability to multi-task
- Poor judgment
- Potential for increased depression, anger, impulsivity, aggression
Sleep Stages
- Stage 1
- brief transition when first falling asleep
- Stages 2 through 4 (slow-wave sleep)
- successively deeper stages of sleep
- Stage 4
- characterized by an increasing percentage of slow, irregular, high-amplitude delta waves
Maintain Daytime Alertness
- Keep morning wake time the same
- Sunlight exposure in the morning
- Limit naps to <1 hour early in the day
- Exercise early in the day
Sleep Hygiene to Promote Better Sleep
- Ask your patient: What do you do to prepare for sleep, starting around dinner time?
- Set up a routine to slow down in in the evening hours:
- bathing or showering
- turning off TV / other electronics
- listening to calming music
- getting up from bed if sleep onset is >20 minutes
Urinary Incontinence
- Defined as involuntary urinary leakage
- Can occur due to:
- Functional abnormalities of the lower urinary tract
- Infection or other associated illnesses
Risk Factors for Urinary Incontinence
- Age
- Obstetric factors (e.g., pregnancy and parity)
- Menopause and hysterectomy
- Lower urinary tract symptoms
- Family history and genetics
- Smoking, diet, and obesity
- Cognitive or functional impairment
Classification of Urinary Incontinence
- Stress Incontinence
- on effort, exertion, sneezing, or coughing
- Mixed Urinary Incontinence
- urgency with exertion, effort, sneezing, or coughing
- Overactive Bladder Syndrome
- with or immediately preceded by a sensation of urgency to urinate, with or without frequency
Urinary Incontinence Evaluation
- Comprehensive history including quality of life factors
- Physical exam to include cardiovascular, abdominal, musculoskeletal, neurologic, and genitourinary exams
- Testing may include bladder diary, stress test, urinalysis, renal function
Bladder Training Techniques
- Schedule Voiding
- Initially every 2 hours throughout the day
- If no incontinence occurs after 1-2 weeks, increase timeframe to every 3 hours
- Urgency Suppression
- Be still, don’t rush to the bathroom
- Do pelvic muscle contractions
- After urgency passes, go to bathroom
Obesity Definition
- Body Mass Index (BMI) describes relative weight (kg) to height (m²)
- Overweight = 25–29.9 BMI
- Obesity = >30 BMI
Health Benefits of Weight Loss
- Decreased
- cardiovascular risk
- glucose and insulin levels
- blood pressure
- LDL and triglycerides, increased HDL
- severity of sleep apnea
- symptoms of degenerative joint disease
- Improved
- gynecological conditions
Goals of Weight Management Treatment
- Assist patient in preventing further weight gain (as minimum goal) with healthy food choices.
- Reduce body weight slowly with healthy changes and increased physical activity.
- Maintain a lower body weight over the long term.
Aspects of Nicotine Addiction
Aspects of Nicotine Addiction
The cigarette provides a highly efficient, engineered vehicle to deliver nicotine, facilitating a complex addiction that involves physical/biochemical, psychological, behavioral, and social aspects.1,2 The act of smoking becomes incorporated into daily routines and is often associated with ritualized behaviors, and nicotine dependence has been identified as the key predictor of cessation success in several large-scale prospective studies.3,4
References
- Cofta-Woerpel L, et.al. Behav Med. 2007;32:135-149
- Heishman SJ. Nicotine Tob Res. 1999;1:S143-S147
- Hyland A, et.al. Nicotine Tob Res. 2004;6:S363-S369
- Hyland A, et al. Tob Control. 2006;15:iii83-iii94.
Benefits of Quitting
- Reduces
- risk of all-cause mortality among patients with coronary heart disease1
- mortality among those who have had a myocardial infarct2
- cancer risk3
- risk of stroke4
- Improves
- airflow obstruction regardless of baseline lung function5
References
- Critchley JA, Capewell S. JAMA. 2003;290:86-97
- Wilson K, et.al. Arch Intern Med. 2000;160:939-944
- U.S. Department of Health and Human Services. Health Benefits of Smoking Cessation. A Report of the US Surgeon General. Rockville, MD: U.S. Department of Health and Human Services; 1990
- Wannamethee SG, et.al. JAMA. 1995;274:155-160
- Scanlon PD, et al. Am J Resp Crit Care Med. 2000;161:381-390.
Personalize Technique
- Express empathy, indicate you care for their well-being
- Address health, financial, and cosmetic benefits of quitting
- Use a positive approach
- Focus on the product not the smoker
Reference
Blum AM, Solberg EJ. In Fundamentals of Clinical Practice: A Textbook on the Patient, Doctor and Society. Ed: Mengels MB, Holleman WL, Fields SA, New York: Plenum, 2002.
Assess Motivation to Quit Smoking
- Ask patient to:
- list reasons to smoke versus reasons to quit
- rate desire to quit
- (0 = no desire to quit to 10 = I will quit today)
- rate confidence that they can quit
- (0 = no confidence to 10 = I can do this easily)
Identify Possible Interventions
- Behavioral
- Self-help
- Brief advice
- Counseling
- Exercise/diversional techniques
- Pharmacologic
- Nicotine replacement therapy
- Buproprion
Individualize Treatment
- Listen to the patient
- Draw on patient’s past experience
- Address psychosocial issues
- Use a multidisciplinary approach
- Re-assess
Re-assess/Revise Treatment
- Always use the same scale to re-assess pain and associated symptoms (e.g., sleep, mood)
- Evaluate for changes in frequency and intensity
- Make treatment changes sequentially whenever possible
- Re-assess AGAIN!
Behavior Change
Transtheoretical Model of Change
- Produces high-impact change programs for entire populations
- Applied to a wide range of problem behaviors
- Applied to a wide range of populations.
- Data driven
“Stage” of Change
- An index (i.e., measure) of readiness to change
- Predictive of who will change successfully after this specific visit
- Dynamic (not static) client/patient characteristic
- Inclusive, empathic, optimistic
Stage of Change Theory
- Guides the selection of both what the provider communicates to the patient (content, methods) and the selection of treatments, which should be matched the patient’s present stage
- Patients move between stages based on factors separate from health status and health care
- clinicians must assess stage at every visit and tailor communication and treatment to match
Stage 1: Precontemplation
- Cons > Pros
- Defensive
- Resistant
- Change experienced as coerced
- Demoralized
- From 30 to 85% of population at risk
Stage 2: Contemplation
- Pros = Cons
- Ambivalent
- Lack commitment
- Lack confidence
- ‘Chronic’ contemplation
- From 10 to 50% of population at risk
Stage 3: Preparation
- Pros > Cons
- Have a plan
- Have taken small steps
- Decisive/committed
- More confident
- Ideal program participants!
- From 5 to 35% of population at risk
Stage 4: Action
- Individuals working to make change
- Individuals may experience strong urge to revert back to old behavior
- Recycling to earlier stage is common
- Greatest risk of relapse at this stage
Stage 5: Maintenance
- Higher self-efficacy
- Dynamic (not static)
- Consolidate gains
- Improve coping skills
- Life-long struggle
Stage 6: Termination
Maintained Behavior Change for >= 5 Years
- New behavior has become a habit
- Little/no temptation
- High degree of confidence, self-efficacy
Risk Factors for Relapse
- Inappropriate goals
- Inadequate preparation
- Not enough time
- Giving up too easily
Relapse
- Relapse is norm rather than the exception
- On average, smokers attempt to quit 7 times before succeeding
- Only a small percentage of relapsers slip back to Stage 1: Precontemplation.
Motivational Interviewing
- Encourages a partnership between patient and health professional
- Used to facilitate patient behavior change
- Explores patient’s ambivalence to change
- 5 Principles:
- Expressing empathy
- Developing discrepancy
- Rolling with resistance
- Avoiding argumentation
- Supporting self-efficacy
Chiropractic Care
The patient history performed by the Chiropractor is similar to that of the primary care provider. The exception occurs when the level of questioning relates to:
- Neurology
- Spinal function
- Patient mobility and pain
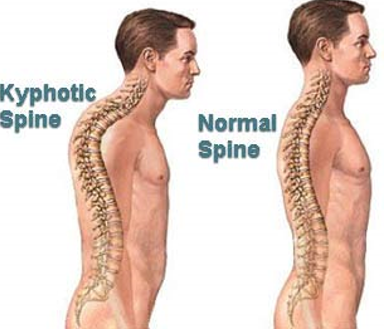
Physical Examination: Some Important Concepts
- Assess balance status
- Gait (wide based/ataxic/shuffling)
- Observation of spine
- (curvature/antalgia)
- Range of motion
- Spinal
- Extremity
Neurologic Examination in the Older Adult
- Special considerations:
- Myotomes
- Myotome- muscles innervated by a single nerve root
- Reflexes
- Dynamic Testing
- Sensory evaluation
- Dermatome- sensory region of skin innervated by a nerve root
- Pinprick
- Vibration
- Proprioception
- Myotomes
Orthopedic Exam
- Standing, seated, supine, prone
- Always perform what is most comfortable for the patient and gains the most information
- Named tests often do not provide the entire picture
- Anatomy
- Stretch, Compress, Distract, Translate the spine.
- Assessment of the spine in each of these directions assists in determining treatment plan.
- Directional preference
- Provides information for both treatment and home exercise
Treatment
- Fall prevention
- Nutritional Recommendations
- Osteoporosis: Calcium/Magnesium/Vit D
- Confirm with pharm D and primary care provider
- Encourage activity and exercise
- Activity is often better than specific exercises
- Referral to Physical Therapy for continuation of exercise program
Joint Dysfunction/Spinal Hypomobility
- The capsular ligament is the primary soft tissue affected.
- It has poor blood supply so damage (e.g., sprain) heals slowly.
- During the reparative stage, if further macro-or micro-trauma is occurring by repetitive forces, fibroblasts will infiltrate the damaged area, and secrete collagen.
- Fibroblasts come mainly from the damaged ligaments or by blood supply from other areas, and will form in irregular patterns that create scar tissue or adhesions.
- Once adhesions are formed, (6-8 weeks), functional disability can occur and decrease segmental mobility.
- Scar tissue/adhesions create functional disability and pain because the two main functions of scar tissue are to:
- protect from further trauma by forming a less elastic tissue.
- prevent further movement at the level of injury
Two types of clinical presentation most commonly seen in chiropractic offices:
- Trauma
- Overuse injuries- (usually seen at the soft tissue level)
Artificial immobilization of joints can produce:
- Intra-articular edema
- Joint capsule shrinkage
- Calcification
- Osteophytic formation
- Intra-articular adhesions
- Shortening of peri-articular connective tissue.
- Adhesions between the capsule and the meningeal covering of the nerve root
Therefore:
- The objective of any manipulative procedure/treatment, such as motion flexion distraction, is restoration of full and painless range of motion.
- Forced movement (e.g., manipulation) ruptures adhesions about a joint and can be curative.
Motion flexion distraction (manipulation and passive motion) is designed to disrupt fibrosis by breaking up adhesions. New blood flow will occur especially in areas that had been ischemic permitting new movement in a hypomobile joint, and allowing synovial fluid to reaccumulate.
Safety of Spinal Manipulation
In the older adult, safety is critical given the reduced strength, endurance, and tissue capacity associated with aging and disease.
Spinal manipulation has been shown to be safe in the general population.
Six prospective studies have been done looking at spinal manipulation; these studies evaluated over 2000 patients.
In these six prospective studies, no incident of serious complication was noted.
Reference
Ernst E. Prospective investigations into the safety of spinal manipulation. J Pain Symptom Manage 2001 21(3):238-242.
Relative Contraindications In the Older Adult
- Severe osteopenia and osteoporosis can be relative contraindications to SMT.
- Exercise extreme caution when performing manipulation on these patients.
- Specifically avoid any axial loading forces
Some Types of Commonly used Chiropractic Techniques
- Diversified Spinal Manipulative Therapy (High Velocity Low Amplitude)
- Cox Flexion Distraction Decompression
- Activator (Instrument Assisted)
- Gonstead (High Velocity Low Amplitude)
- Thompson Drop Table
SPINAL MANIPULATION: Flexion Distraction Decompression
“A form of chiropractic adjustment of the Intervertebral Disc, posterior facet elements, and osseoligamentous canals."

Flexion Distraction Decompression Benefits
- Increases intervertebral disc height to remove annular distortion in the pain sensitive peripheral annular fibers
- Allows the nucleus pulposus to assume its central position within the annulus and relieve irritation of the pain sensitive fibers
- Restores vertebral joints to their physiological relationships of motion
- Improves posture and motion while relieving pain and improving function
Flexion Distraction Decompression Treatment Conditions
The following spinal conditions are treated on a motorized Flexion Distraction Decompression table:
- Sciatica
- General back pain
- Scoliosis
- Facet Syndrome
- Spondylolisthesis
- Joint Dysfunction
- Degenerative Joint Disease
Spinal Manipulation: HVLA Manipulation
“Consists of a thrusting, impulse-like force of specific intensity, direction, and time history applied to the target vertebrae on the spine.”

Reference
Herzog: Mechanical and Physiologic Responses to Spinal Manipulative Treatments. JNMS 3(1): 1-9
Adverse Events Associated with Spinal Manipulation
- Most adverse events
- Are benign and transitory although there are reports of complications that were life threatening
- The frequency of adverse events of all types varies between 33% and 60.9% (the vast majority of these events are benign and self limited)
- The reported frequency of serious adverse events has varied greatly
- 1.46 serious adverse events/10,000,000 manipulations
- 2.68 deaths/10,000,000 manipulations
Reference
Gouveia LO, Castanho P, Ferreira JJ. Safety of chiropractic interventions: a systematic review. Spine 2009 May 15;34(11):E405-13.
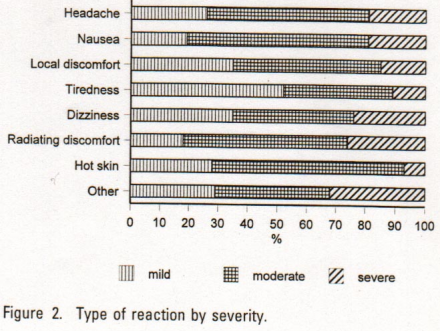
Side effects from Spinal Manipulation
- Local Discomfort: 53% (50-56)
- Headache: 12% (10-14)
- Tiredness: 11% (9-13)
- Radiating discomfort: 10% (8-12)
- Dizziness: 5% (4-6)
- Nausea: 4% (3-5)
- Hot skin: 2% (1-3)
- Other: 2% (1-3)
Spinal Manipulation: Maximizing the Benefits
Treatment based on patient goals:
- Decrease Pain
- Increase Mobility
- Stabilize Spine
- Increase Proprioception
References
Clark B; Gross D. et al. Neurophysiologic effects of spinal manipulation in patients with chronic low back pain. BMC Musculoskelet Disord. 2011 Jul 22;12(1):170
Learman KE, Myers JB, et al. Effects of spinal manipulation on trunk proprioception in subjects with chronic low back pain during symptom remission. J Manipulative Physiol Ther. 2009 Feb;32(2):118-26.
Chou, R, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007 Oct 2;147(7):478-91
Cochrane Database
Evidence for spinal manipulation in low back pain.
The efficacy of spinal manipulative therapy has been found to be equal to:
- general practitioner care
- analgesics
- physical therapy
- exercises
- back school for patients with low back pain
Reference
Spinal manipulative therapy for low-back pain. [Systematic Review] Cochrane Back Group Cochrane Database of Systematic Reviews. 3, 2004.
Review of the Literature
- Identifying safe and effective interventions for acute and chronic musculoskeletal pain syndromes
- high prevalence
- negative impact on quality of life
- long term risks associated with chronic medication use
Non-pharmacologic therapies for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline.
- For acute low back pain, spinal manipulation is recommended.
- For chronic or sub-acute low back pain recommended treatments include
- intensive interdisciplinary rehabilitation
- exercise therapy
- spinal manipulation
- acupuncture
- massage therapy
- yoga
- cognitive-behavioral therapy
- progressive relaxation
UK BEAM (back exercise and manipulation) Trial
- Participants:
- 1334 patients consulting their general practices about low back pain.
- Randomly assigned to one of 4 groups.
- Conclusions:
- Relative to "best care" in general practice, manipulation followed by exercise achieved a moderate benefit at three months and a small benefit at 12 months;
- spinal manipulation achieved a small to moderate benefit at three months and a small benefit at 12 months;
- exercise achieved a small benefit at three months but not 12 months.
References
- Selim AJ, Berlowitz DR, et al. The health status of elderly veteran enrollees in the Veterans Health Administration., J Am Geriatr Soc. 2004 Aug;52(8):1271-6.
- Hestbaek L. Kristian Larsen, Flemming Weidick, and Charlotte Leboeuf-Yde Low back pain in military recruits in relation to social background and previous low back pain. A cross-sectional and prospective observational survey, BMC Musculoskeletal Disord. 2005 May 26; 6:25
- Sutlive TG, Mabry LM, et al. Comparison of short term response to two spinal manipulation techniques for patients with low back pain in a military beneficiary population. Mil Med. 2009 Jul; 174 (7): 750-6
- Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007 Oct 2;147(7):478-91
- UK Beam Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM randomised trial: effectiveness of physical treatments for back pain in primary care. BMJ. 2004 Dec 11;329(7479):1377. Epub 2004 Nov 19
How is Function Measured?
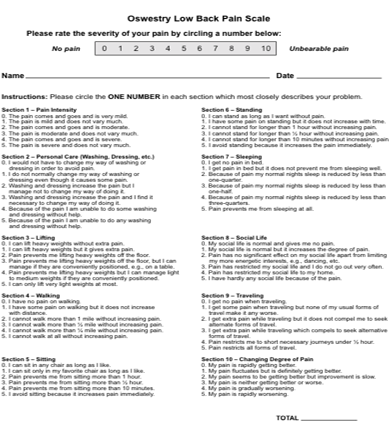
Oswestry Disability Index
Fear Avoidance Belief Questionnaire
Bournemouth Disability Questionnaire
References
- Fairbank JCT & Pynsent, PB. The Oswestry Disability Index. Spine (2000) 25(22):2940-2953.
- Davidson M & Keating J. A comparison of five low back disability questionnaires: reliability and responsiveness. Physical Therapy 2002;82:8-24.
Oswestry Disability Index
The Oswestry Disability Index (also known as the Oswestry Low Back Pain Disability Questionnaire) is an extremely important tool that clinicians, researchers and disability evaluators use to measure a patient's permanent functional disability. The test is considered the ‘gold standard’ of low back functional outcome tools.
Serotonin Syndrome
- Caused by increased serotonergic activity within the central and peripheral nervous system
- Clinical features: neuromuscular hyperactivity, mental status changes, and autonomic instability
- Synergistic effects from use of multiple serotonergic agents and/or drug interactions that decrease the clearance of serotonergic agents
Drugs Associated with Serotonin Syndrome
| Drug Classes | Drugs |
|---|---|
| Monoamine Oxidase Inhibitors (MAOIs) | Dextromethorphan |
| Tricyclic Antidepressants (TCAs) | Tramadol/Tapentadol |
| Selective Serotonin Reuptake Inhibitors (SSRIs) | Fentanyl |
| Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) | Lithium |
| Serotonin Receptor (5HT3) Antagonists | Metoclopramide |
| Atypical Antipsychotics | Buspirone |
| Triptans | Trazodone |
| St. John's Wort | |
| Cocaine | |
| Meperidine |
Serotonin Syndrome Signs and Symptoms
| Severity | Serotonin Syndrome Signs and Symptoms |
|---|---|
| Mild | Hyperreflexia, Clonus (LE>UE), Shivering, Diaphoresis, Mydriasis, Diarrhea, Tachycardia Afebrile |
| Moderate | Hyperreflexia, Clonus (LE>UE), Shivering, Diaphoresis, Mydriasis, Diarrhea, Tachycardia HTN, Hyperthermia (< 40°C), Hyperactive Bowel Sounds, Mild Agitation, Hypervigilance, Pressured Speech |
| Severe |
Hyperreflexia, Clonus (LE>UE), Shivering, Diaphoresis, Mydriasis, Diarrhea, Tachycardia, Hyperactive Bowel Sounds |
Reference
N Engl J Med. 2005;352(11): 1112-1120.
Serotonin Syndrome Treatment
- Symptoms usually resolve with 24-72 hours
- Longer if drug has a long half life or active metabolite
- Stop offending agent
- Benzodiazepines
- Supportive care
Depression is Extremely Common in Patients with Chronic Pain
Mean rates of current depression among patients with chronic pain in various settings:
- Primary Care: 27%
- Pain Clinics: 52%
- Orthopedics: 56%
- Rheumatology: 56%
- General Population: 27%
Reference
Bair et al. Archives of Internal Medicine. 2003;163(20):2433-45.
Sociodemographic Risk Factors for Depression Among Patients with Chronic Pain
- Poverty
- Persons of color, particularly African Americans
- Older Adults
- Women
Other Risk Factors for Depression
- History of depression
- Family history of major depressive or bipolar disorder
- Personal or family history of suicide attempts
- Substance abuse
- Recent stressful life events and lack of social supports
Patients with Depression Usually Present with Physical Symptoms Only
69% presented ONLY with physical symptoms. (Out of N = 1146 patients with major depression.)
Reference
Simon GE, et al. N. Engl J Med. 1999;341(18):1329-1335. Courtesy of Matthew Bair, M.D.
Depression is Often Missed
Providers are aware of the presence of depression in approximately 20% of their patients with chronic pain.
Detection rates of depression drop as number of physical symptoms increase.
References
- Poleshuck EL, et al. J Women’s Health. 2006; Mar;15(2):182-93
- Bair MJ, et al. Archives of Internal Medicine. 2003;163(20):2433-45.
Why is it Important to Address Depression in Patients with Pain?
- Depression is the leading cause of disability in the US
- Pain patients with depression have more disabling pain and worse prognosis for treatment of their pain than pain patients without depression
- Untreated depression is a risk factor for difficulties with treatment adherence, treatment outcomes, and relapse among patients with pain
- Treatment of depression improves pain outcomes
References
- Burton AK, et al. Spine. 1995;20(6):722-8.
- Farmer TC et al Psychosomatic Medicine. 2010; 72(1):61-67.
- Greenberg PE, et al, Journal of Clinical Psychiatry. 2003;64(12):1465-75
How to Introduce the Topic of Depression
- Emphasize that the pain is real and not “in your head”
- Normalize experience of depression in response to living with pain
- Identify reciprocal nature of pain and depression exacerbating one another
- Acknowledge depression responds to treatment
DSM-IV Definition of Major Depressive Episode
- At least one of the following symptoms present most of the day nearly every day for 2 weeks or more:
- Depressed mood
- Markedly diminished interest or pleasure
And 4 or more of the following symptoms present 2 weeks or more:
- Significant weight loss/gain
- Insomnia/hypersomnia
- Psychomotor agitation/retardation
- Fatigue or loss of energy
- Feelings of worthlessness or excess guilt
- Impaired concentration or indecisiveness
- Recurrent thoughts of death or suicide
Screens
- Screens can be very useful ways to identify patients who may have depression
- Screens must be used in combination with interview and clinical assessment; they are not diagnostic tools
- The PHQ-9 is a well-validated 9-item depression screen that has 88% sensitivity and specificity for a Major Depression Episode diagnosis
Reference
Kroenke K, et al. Journal of General Internal Medicine. 2001;16(9):606-13.
PHQ - 9 Depression Scale
Scoring and Interpreting the Personal Health Questionnaire-9
- Sum each item (0-3 points)
- Cut points for depression severity:
- greater than or equal to 5: mild
- greater than or equal to 10: moderate
- greater than or equal to 15: moderately severe
- greater than or equal to 20: severe
Suicide and Chronic Pain
- Patients with chronic pain experience elevated rates of:
- Suicidal ideation
- Suicide attempts
- Suicide completion
- Management of suicidality is associated with lower rates of suicide among patients with chronic pain
References
- Gilbert JW, et al The International Journal of Neuroscience. 2009; 119 (10): 1968-1979.
- Fishbain DA. Semin Clin Neuropsychiatry. 1999;4:221-7.
How to Assess Suicidal Risk
- Listen for themes of hopelessness and helplessness
- Ask questions such as:
- In the past week, have you wished you were dead or thought things would have been better if you had never been born?
- Have you thought about killing yourself?
- What kinds of ideas did you have about how you would kill yourself?
- Plan, means, intent
- Have you tried to kill yourself in the past?
When to Make a Referral to a Mental Health Specialist
- Significant depression and/or suicidal concerns
- Patient prefers to minimize pain medication use
- Patient needs more time and attention than provider can offer
- Poor response to medical treatments
- Patient, provider, or family member frustration
Following up with Patients with Depression
- Schedule regular appointments
- Include important support people
- Collaborate with the mental health professional
- Reassure patient you:
- Believe the pain is real
- Will not abandon him/her
MacArthur Initiative on Depression in Primary Care: Depression Management Tool Kit
- Excellent resource for more detailed information on the assessment and treatment of depression:
- Includes easy to use tools to assist with:
- Recognizing and diagnosing depression;
- Educating patients about depression, assessing treatment preferences, engaging their participation and explaining the process of care;
- Using evidence-based guidelines and management tools for treating depression; and
- Monitoring patient response to treatment.
Can be accessed here: https://www.aetnabetterhealth.com/content/dam/aetna/medicaid/maryland/providers/pdfs/Macarthur%20Depression%20Toolkit.pdf
Suicide Risk Factors
- Caucasian
- Hopelessness
- Living alone
- General Medical illness
- Psychosis
- History of prior suicide attempts
- Family history of suicide attempts or substance abuse
- Recent crisis or loss
Assess Suicidal Ideation
- In the past week, have you wished you were dead or thought things would have been better if you had never been born?
- Have you thought about killing yourself?
- What kinds of ideas did you have about how you would kill yourself?
- Plan, means, intent
- Have you made a previous attempt?
Evaluate Treatment Response and Re-assess
- Schedule regular appointments
- Invite feedback
- Reassure patient you:
- Believe the pain is real
- Will not abandon him/her
When to Make a Referral to a Mental Health Professional
- Any chronic problem
- Patient’s request
- You can’t meet patient’s needs for time and attention
- Further assessment or consultation needed
- Frustration
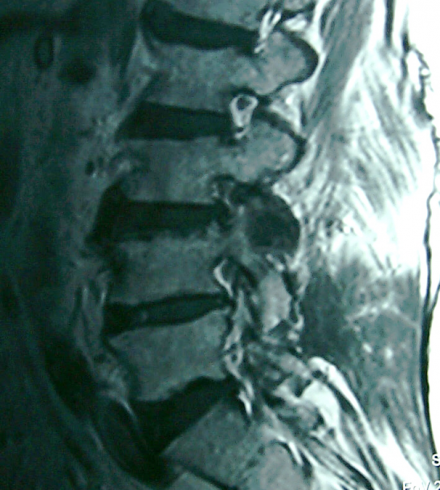
Pathophysiology of Stenosis
Progressive narrowing of the spinal canal may occur alone or in combination with acute disc herniations. Congenital and acquired spinal stenoses place the patient at a greater risk for acute neurologic injury. Spinal stenosis is most common in the cervical and lumbar areas.
Lumbar spinal stenosis implies spinal canal narrowing with possible subsequent neural compression. Although the disorder often results from acquired degenerative changes-spondylosis.
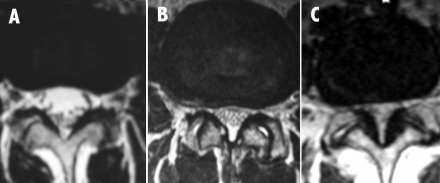

Compresses the exiting nerve root.
Differential Diagnosis
- Vascular claudication
- Osteoarthritis of hip or knee
- Lumbar disc protrusion
- Intraspinal tumor
- Unrecognized neurologic disease
- Peripheral neuropathy
Canal stenosis in the lumbosacral region often results in findings of:
radicular pain, neurogenic claudication, or both.
Lateral stenosis: radicular pain, weakness and numbness a long side of distribution.
Foramenal Stenosis
- Root symptoms
- Unilateral
- No claudication
- Acute or chronic
Lateral Recess Stenosis
- Claudication
- Radicular pain
- Weakness is rare
- Acute or chronic
Central Stenosis
- Varied presentation
- Classically with neurogenic claudication
- Some may only have back pain
- Rarely painless progressive weakness
Overview of Traditional Chinese Medicine (TCM) and Patterns of Disease
Before continuing please review the following references:
Comparative study on WHO Western Pacific Region and World Federation of Chinese Medicine Societies international standard terminologies on traditional medicine: Syndrome Differentiation According to Eight Principles https://pubmed.ncbi.nlm.nih.gov/20550884/
TCM Diagnosis http://www.sacredlotus.com/diagnosis/eleven_treatments.cfm
Diagnosis
- Diagnosis in Chinese medicine identifies the disease process and the “pattern” that characterize expression pathophysiological disease process.
- At the root of TCM concepts of physiology and pathology is the normal functioning of organ systems in receiving, transforming, and circulating blood, nutrients, and fluids.
- Fundamental to this process is an amorphous dynamic substance called “qi” (pronounced chee).
qi
- Qi can be translated as finest matter influences, fine substances that circulate throughout the body, producing movement, communication between body systems, and reaction to environmental changes.
- Today, qi is understood as physiological activity and material substrates that support it.
- Qi, depending on its role in a particular condition, is involved in the conversion of nutrients to energy, respiration, the function of body systems, immune response, and temperature regulation.
- Qi is considered to circulate with blood and the two substances are closely linked in traditional theory.
- Many observations about the behavior of qi that inform acu-puncture theory are believed to be neurovascular phenomena.
Pain in Chinese Medicine
- Pain is thought to be produced by the failure of qi to circulate freely in the area where the pain is experienced.
- No matter how the free movement of qi is inhibited, acupuncture treatment for pain involves selecting locations for needling on the body that improve local circulation and support physiological functions that can eliminate the causes of the inhibited movement.
Deciding to Seek Acupuncture for Low Back Pain
- Patients may seek out a Licensed Acupuncturist based on information received from numerous sources including positive experiences reported by members of their social network.
- Alternatively, they may be referred by a health care provider.
- Chronic low back pain is a common reason for seeking acupuncture treatment.
Evidence Base
Although the evidence base for acupuncture is limited by many factors, both low back pain and osteoarthritis of the knee have been shown to respond to treatment in a number of studies.
Structure of Acupuncturist Assessment
- Subjective
- Inquiry
- Objective
- Inspection
- Listening & Smelling
- Palpation
- Assessment
- Treatment plan
Acupuncturists typically use an assessment methodology that is organized along the SOAP format. Gathering data on the patient using questionnaires, transmitted patient records, and history taking. Generally physical examination in the form of visual and palpatory assessment of the patient is performed in the course of the intake process or immediately preceding treatment. These two methods constitute the subjective and objective aspects of data collection. An assessment is made and treatment is planned on the basis of the assessment and relevant findings on examination. Traditionally the assessment is based on four areas of data collection: Inspection, Inquiry, Listening and Smelling, and Palpation.
Inquiry
Inquiry examination includes:
- History of the present illness
- History of previous disease conditions
- General circumstances
- Personal life circumstances
- Family history
In general, patients presenting for acupuncture are seeking help for a specific problem although as is the case with Mrs. Johnson, the may have numerous comorbidities. As the medical history is taken the acupuncturist may discern relationships between the presenting or chief complaint and other clinical conditions or life style issues.
Inquiry: Present Disease History
10 Questions
- Body Temperature (Hot/Cold)
- Sweat
- Head/Body
- Urine/Stool
- Drink/Food/Taste
- Ears & Eyes
- Chest/Rib-side/Abdomen
- Thirst/Beverages
- Sleep
- Children, Men, Women, Geriatrics
The 10 Questions are a flexible rubric of areas of systematic inquiry concerning the patient’s condition and chief complaint. They are used to organize subjective findings and relate it to Chinese medicine perspectives on disease processes. In this segment that follows the acupuncturist explores aspects of the patients other clinical conditions, in effect conducting a review of systems while addressing several of the clinical areas addressed in relation to the 10 questions. In this case the acupuncturist is inquiring about pain in the body with questions concerning the patient’s history of osteoarthritis and shoulder pain. Questions concerning smoking and COPD pertain to the chest. A discussion of sleep disturbances leads to a conversation about abnormal urination (stress incontinence).
Inquiry about Head and Body
Questions about sensations and experiences of the head and body, including pain, elicit information about the region, type, and nature pain.
Ask:
- about the presence or absence of sensations of heaviness and numbness
- whether the lumbus (lower back and sides between the ribs and pelvis), back, and four limbs can move flexibly.
- Interior Pattern:
- Phlegm damp blocking and stagnating the channels and networks.
- Heaviness/numbness of the lumbus, back, and limbs.
- Qi and blood vacuity weakness
- Numbness of the limbs
- Limbs are relatively withered/weak, or without strength
- Vessels and channels lack nourishment.
- Kidney vacuity
- Lumbus and legs are always sore, painful, and without strength; worse with exertion
- Phlegm damp blocking and stagnating the channels and networks.
- Impediment Pattern
- Entire body may be painful
- Pain is especially seen in the lumbus, back, or joints of the four limbs
- Pain comes and goes
- Pain appears each time there is a change in the weather
- wind, cold, damp and heat evils cause the pattern
- Moving
- Moves/flows without definition; joints hurt successively
- Fixed
- Does not move, accompanied by general heaviness of the body and cumbersome fatigue
- Painful
- Violent and persistent; slightly reduced with warmth
- Heat
- Accompanied by fever, redness, and swelling of the painful area; slightly reduced with cold
Scope of Acupuncture Practice
- Licensed Acupuncturists collect and evaluate the patient’s medication history to be aware of side effects of drugs that may influence treatment outcomes.
- When the patient is taking many medications or has not had them reviewed recently, referral to a pharmacist may be appropriate.
- If herbal therapy is contemplated, risks for pharmaco-kinetic or pharmacodynamic interactions need to be assessed.
Making a Chinese Medicine Diagnosis
- Degenerative changes to bone are considered an aspect of the decline of the kidney system and are encountered in aging patients.
- Painful joints, including the back, and pain worsened by cold and improved by heat suggest a wind cold damp impediment, inhibiting the movement of qi and blood in the acupuncture channels (meridans).
Disease and Pattern
Most diseases in Chinese Medicine are associated with a pattern based on the presenting signs and symptoms.
- The patients age and clinical signs such as stress incontinence suggest kidney vacuity lumbar pain.
- The signs of damp accumulation such as overweight, osteoarthritis relieved slightly by heat, and the increased severity of symptoms when the weather is cold suggest cold-damp lumbar pain.
Disease
- Lumbar pain 腰痛 yao tong
- a disease presenting with pain in the lumbus on one or both sides or affecting the spine.
- causes include taxation detriment, debility in old age, depletion of kidney qi, contraction of external evils, and external damage.
Population Based Health Care
What Is Population Health?
- A cohesive, integrated, and comprehensive approach to health care that considers:
- the distribution of health outcomes
- the health determinants that influence distribution of care, and
- the policies and interventions that impact and are impacted by the determinants.
Health Disparities
Differences in the incidence, prevalence, mortality, or burden of diseases as well as other adverse health conditions or outcomes by population group. For example, by groups defined by:
- Socioeconomic status
- Disability
- Sexual orientation
- Geography
- Age
- Special needs
- Race and ethnicity
Cultural Competency
- Understanding social and cross-cultural influences of different populations’ values, health beliefs and behaviors, disease prevalence and incidence and treatment outcome;
- Considering how these factors interact with and impact multiple levels of health care delivery systems;
- Implementing interventions to assure quality care to diverse patient populations
Population Health
A health care delivery approach that addresses the underuse and overuse of health care resources, seeking increased clinical quality at optimal expense via:
- Patient-centered care
- A responsible primary care provider
- Patient-Centered Medical Home
- Assessment of health determinants
- Clinical, public health and community integration
- Evidence-based guidelines
- Appropriate health education that promotes self care
- Health Information Technology
Health Promotion
- The provision of clinical and public health services to collaboratively address the impact of health determinants for the purpose of improving and sustaining the highest quality of well-being attainable.
- The process of enabling people to increase control over their health and its determinants to improve their health.
- To reduce avoidable expense, clinical burden and the unsustainable trend in health care costs.
Prevention
The interlocking and mutually supportive strategies and interventions aimed at the deterrence, early detection, and minimization or cessation of disease and injury at a population level.
- Primary: before asymptomatic disease appears
- Secondary: early identification of asymptomatic disease
- Tertiary: aimed at slowing the progression of confirmed disease
Screening
The presumptive identification of unrecognized disease or health risks by applying population level surveys or laboratory or other test results in electronic medical records, or other procedures. Important to consider:
- distribution of disease
- evidence supporting screening
- validity of available tests
- benefits and risks of screening
- availability and costs of treatment
- determination of whether evidence-based and eligibility criteria exist
Disease Management
- A system of coordinated health care interventions and communications for populations with conditions in which patient self-care efforts are significant
- Evidence suggests it can reduce costs related to congestive and coronary heart disease, diabetes, and depression
- Studies are underway to address its impact on health care utilization; clinical outcomes; primary and secondary disease; prevention; pharmaceutical utilization; productivity measures; reductions in co-morbidities and indirect costs
Behavior Change
- Modifying the physical, emotional, habitual and cultural factors that influence health status
- Paired with usual health care
- Relies on non-physician staff to educate, support, follow-up, and evaluate effectiveness.
- At the population level, uses health information and other technologies to assess and support patient status and progress.
Health Information Technology (HIT)
- “Meaningful Use” of Health IT
- HIT implementation incentives paid to physicians and hospitals (via Medicare) from 2009 stimulus funds to establish electronic medical records (EMRs)
- “Meaningful use” required by 2015 to avoid reduced Medicare payments.
- “Meaningful use”= use HIT to improve clinical decision making, enhance efficiency & patient safety, reduce health disparities, engage patients & families, monitor & improve quality, or improve cost-efficiency
Examples of Meaningful Use in Pain Management
Imagine:
- An interactive voice response technology (IVR) system (commonly used by pharmacies to ask of prescription should be refilled), that queries patients about their pain in between visits? Patients reporting uncontrolled pain could be telephoned and counseled about medications, referrals, or office visits.
- An EHR linked to a community-wide regional health information organization that warns a prescriber of active opioid prescriptions written by other providers.
Personal Health Records
- Particularly useful for adult children helping to manage an elderly parent’s care
- Two basic models:
- Patient portal into a provider’s EHR—patient may view their record and exchange “secure e-mail” with their physician or other provider
- Stand-alone system, designed to operate with multiple providers’ EHRs
Think, Pair, Share
Your Patient-Centered Medical Home has 1,000 patients who are clinically similar to Mrs. Johnson. Your PCMH plans to offer a new evidence-based intensive weight management program. To start, the program can only be offered to 100 patients.
How might you meet Medicare’s meaningful use of electronic medical records criterion and identify the 100 patients who would best benefit from the new program?
A range of answers are possible, such as:
- Use the PCMH EMR text field to identify patients who are currently planning or actively working on weight loss using text mining software. Call those patients to recruit them to the new program before their regularly scheduled visit.
- Using interactive voice response technology (IVR) conduct a telephone survey of the 1,000 patients to identify those at the “Action” or “Planning” phase for weight management, specifically. Be sure to offer the IVR survey in Spanish and other languages common among the group of 1,000 patients like Evelyn. Be sure to design the survey so that it may be understood with low levels of health literacy. Similarly, the intervention should be designed to manage low health language literacy.
Reference
Barkley EF, Cross KP, Major CH. (2005) Collaborative Learning Techniques: A Handbook for College Faculty. Jossey Bass. San Francisco, CA.
Self Care
- Consumers can readily learn to:
- care for themselves
- participate in goal-setting
- engage in collaborative decision making
- Patients who are actively managing their health often demand more health care services; Self-care may reduce the demand (and costs).
The Patient
Provider-Patient Relationship Models
- Szasz and Hollender’s
- Consumer model
- Patient-centered model
- Biopsychosocial model
Szasz and Hollender
- Activity-Passivity
- Patient is a passive recipient of care
- Analogy: Parent-infant relationship
- Guidance-Cooperation
- Patient defers to medical expertise
- Communication and more independence/input
- Analogy: Parent-adolescent relationship
- Mutual Participation
- Patient and physician are interdependent
- Dependent on EXCELLENT communication skills!
Consumer Model
- Reverses traditional prescriber/patient balance of power
- Informed and skeptical buyers of medical care
Patient-Centered Model
- Holistic approach.
- Point of view of the patient
- All aspects of care are considered
- Opposite
- Disease-Centered Care: Focus on the accurate diagnosis and treatment of the organic pathology until cure is not possible.
Biopsychosocial Model
- Developed at the University of Rochester
- George Libman Engel (1913-1999)
- Incorporated into medical school training
- Disease /well-being the result of the interplay of:
- Physical context
- Social context
- Emotional state
- Psychological state
- Applied in funded NIH Pain Collaborative Pain Education Grant (2012-2014)
Adherence
Adherence vs. Compliance
- Compliance
- Patient following or “complying” with a health professional’s recommendations.
- Adherence implies a patient choice in compliance
- Also acknowledges that non-adherence may not be the result of a decision by the patient to not take the medication as prescribed, but rather may be due to a variety of other factors that might be modified.
Adherence Factors
- Factors influencing adherence:
- Health system
- Social/economic
- Condition-related
- Patient-related
- Therapy-related
- Moriskey Scale (8 items: cost, side effects, etc.)
- Example: Rochester Hypertension Collaborative
Health Literacy
- The degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.
- 90 million Americans lack necessary literacy skills to function in the health care system.
- Institute of Medicine (IOM) (2011) has noted that intensive population efforts in health literacy necessary to improve care quality.
- Screening questions for low health literacy:
- How often do you have someone help you read hospital materials?
- How confident are you filling out medical forms by yourself?
- How often do you have problems learning about your medical condition because of difficulty understanding written information?
- Communication Strategies
- Communicate message at the 5th grade level or lower
- Use pictures and models
- Use the teach-back or show-me techniques to assess patient understanding
- Encourage patients to use “Ask me 3”
National Patient Safety Foundation
Ask Me 3. What are the “3” Questions?
- What is my main problem?
- What do I need to do?
- Why is it important for me to do this?
Patients should be encouraged to ask. Providers should always encourage their patients to understand.
Studies show that people who understand health instructions make fewer mistakes when they take their medicine or prepare for a medical procedure. They may also get well sooner or be able to better manage a chronic health condition.
Important Trends Affecting Health Care Professionals
US Health Care in Transition
Compared to the US, the UK, Germany and Canada are all characterized by:
- Lower % of GDP spent on healthcare
- Lower total health expenditures per capita
- Higher life expectancy, lower infant mortality
- Universal heath care
Population Based Health Care
- A critical new tool for moving toward the Triple Aim
- Leverages technology, models of behavior change, education and communication science to collect data, monitor patient changes, manage patient expectations and support behavior change at low cost in groups of patients with similar needs.
- May assist providers by eliminating data collection/assessment time for managing existing chronic conditions (but not new diagnoses) or supporting health promotion and disease prevention.
- A 1-credit hour (semester) section of material on this new field appears in the appendix of this unit.
Interdisciplinary Care
Interdisciplinary care: Many different professionals communicate effectively among themselves and with the patient to care for the patient.
Multi-disciplinary care: Many different professionals work for the good of the patient, albeit somewhat independently.”
Analogy: Have you ever worked on a group assignment for school for which you split up the work and copied and pasted it back together later? That is analogous to multidisiplinary care and the current fee-for-service health care system in which providers get paid for “doing” regardless of the quality of the service or patient outcome. Interdisciplinary care is burdensome in that it requires providers to collaborate effectively, but it may save time in data collection (consider the many duplicative questions asked of the patient) and patient burden.
Reference
McCarthy & Schafermeyer (2007). Ch. 2. p. 57.
Interprofessional Education
- Interdisciplinary training is now being required for accreditation
- Sponsored by the Interprofessional Education Collaborative
- American Association of Colleges of Nursing
- American Association of Colleges of Osteopathic Medicine
- American Association of Colleges of Pharmacy
- American Dental Education Association
- Association of American Medical Colleges
- Association of Schools of Public Health
- Sponsored by the Interprofessional Education Collaborative
Reference
Core Competencies for Interprofessional Collaborative Practice: Expert Panel report, May 2011
Patient-Focused Care
Characterized by:
- decentralization of services
- cross-training of personnel from different departments to provide basic care
- interdisciplinary collaboration
- various degrees of organizational restructuring
- simplification and redesign of work to eliminate steps and save time
- increased involvement of patients in their own care
Critical Care Pathways
- Optimal sequencing and timing of interventions for a particular diagnosis or procedure
- Minimization of delays and resource utilization
- Maximization of quality of care
Continuous Quality Improvement (CQI)
- Also referred to as total quality management (TQM) or total quality improvement.
- Cross-functional, interdisciplinary teams examine processes and revise them on an on-going basis.
- Employees generally more receptive to change when they are active participants in the change process.
Pay for Performance (P4P)
- Defined as: quality based purchasing , the use of payment methods and other incentives to encourage high quality and patient-focused, high value care.
- Model built on defined measures, data collection, and public reporting that includes payment incentives aimed at quality, efficiency, and patient satisfaction.
- P4P programs increasingly are focusing their efforts on outcome and cost-efficiency measures, rather than clinical process measures alone.
Defining Quality
- “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge”
- Institute of Medicine (IOM)
- “Doing the right thing for the right patient, at the right time, in the right way, to achieve the best possible results”.
- Agency for Healthcare Research and Quality (AHRQ )
Components of Healthcare Quality
| Component | Description |
|---|---|
| Effective | Providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit |
| Safe | Avoiding injuries to patients from the care that is intended to help them |
| Timely | Reducing wait times and harmful delays for both those who receive and those who give care. |
| Patient centered | Providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions. |
| Equitable | Providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status. |
| Efficient | Avoiding waste, including waste of equipment, supplies, ideas, and energy. |
Reference
Agency for Healthcare Research and Quality (AHRQ). (2009, March). 2008 National healthcare quality & disparities reports (AHRQ Publication No. 09-0001). Available at www.ahrq.gov/qual/qrdr08.htm
Measures of Quality
- Clinical performance measures of how well providers deliver specific services needed by specific patients.
- Assessments by patients of how well providers meet healthcare needs from the patient’s perspective
- Aggregated population outcomes outcome measures (e.g., mortality rates from cancers preventable by screening)
How is Quality Reported?
- Accreditation of hospitals, other institutions
- Joint Commission
- Report Cards for physicians, health plans, hospitals
- Patient Ratings of providers
- Medicare: CAHPS Survey: Satisfaction with Pharmacy Care

