Mrs. Johnson returns to Dr. Kent’s office after she has had a consultation with the chiropractor to discuss her progress. She meets with the nurse manager to discuss a variety of quality of life issues.
Next, Mrs. Johnson meets with Dr. Kent.
Test Your Knowledge
What single imaging study of her lumbar spine would be the most appropriate at this time?
Follow Up
Mrs. Johnson meets again with Dr. Kent.
Dr. Kent discusses Mrs. Johnson getting an MRI.
Dr. Kent discusses the results of Mrs. Johnson's MRI.
Dr. Kent discusses the cross-sectional results of Mrs. Johnson's MRI.
MRI Demonstrates Central Stenosis at L4-5
Sagittal image of lumbar spine:

Cross section image through the L4-5 level demonstrating central stenosis and Cross section image of a vertebral segment that does not have spinal stenosis.
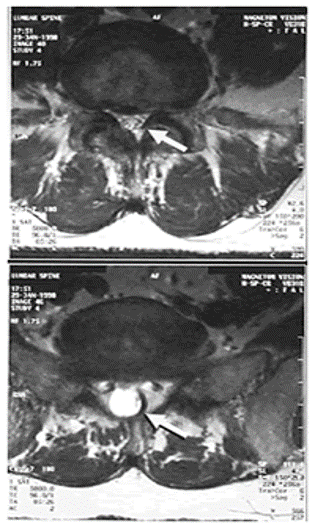
In these T2 weighted images the spinal fluid appears as a bright white signal. At the L4-5 level the volume of spinal fluid is diminished on both the sagittal and cross-sectional images. The arrows on the cross section images point to the spinal canal which is visibly narrowed at the L4-5 level.
Spinal Pathophysiology
As the lumbar region ages, it is common for degenerative changes to develop. Changes in the intervertebral discs, facet joints and supporting ligaments can result in pressure being placed on the spinal nerves. The discs can bulge over time as they become degenerative. If they bulge directly posteriorly they can compress multiple spinal nerves at a time as they traverse the central spinal canal. If the discs bulge posterio-laterally they can impinge nerve roots as they traverse an intervertebral foramen. As facet joints become arthritic, they hypertrophy and can also contribute to either central spinal canal stenosis and/or foraminal stenosis. Lastly, hypertrophy of the ligamentum flavum, located in the dorsal aspect of the spinal canal can contribute to spinal stenosis. All three of these phenomenon are contributing to central stenosis on the MRI images above.
On the sagittal image the spinal canal is narrowed anteriorly by a bulging L4-5 disc and posteriorly by hypertrophied ligamentum flavum. These two factors result in the spinal fluid appearing to have an “hour glass” waist at this level since it is being impinged both from the anterior and posterior sides. On the cross section view enlarged facets joints are seen contributing to the spinal stenosis by impinging the canal from the posterior-lateral direction.
Central spinal stenosis can effect multiple nerve roots simultaneously. Most patients will present with bilateral lower extremity pain, but the presentation can very in location from one patient to another depending on which roots are most symptomatic. Patients tend to report that the pain is relieved with rest and predictably reproduced with standing and walking. This symptom complex is known as “neurogenic claudication”. Patients often reporting that lumbar flexion will reduce or relieve their symptoms. This is because flexion maneuvers tend to widen the central canal. That is why many of these patients report decreased pain and improved walking tolerance when using a walker or grocery cart. If the nerves of the cauda equina become severely impinged, neurological impairments develop. These can present with lower extremity motor deficits, sensory impairment (often most prominent in the perineum and groin and is often referred to as “saddle anesthesia”) and autonomic impairment (this presents as incontinence and loss of anal tone). This constellation of neural impairments is known as “cauda equina syndrome”.
Foraminal stenosis causes symptoms in the distribution of the involved nerve root. The anticipated symptoms and examination findings can be found in figure #1 of the AHCPR guidelines for the management of low back pain.
Test Your Knowledge
Which management options below are appropriate at this time?
Treatment Plan Following Review of MRI Findings
- Patient is referred for physical therapy
- Patient encouraged to pursue acupuncture as we had discussed at the prior visit
- Continue counseling given depression is still burdening her
- She may continue to use hydrocodone in moderation for severe pain and it will be weaned over time.

