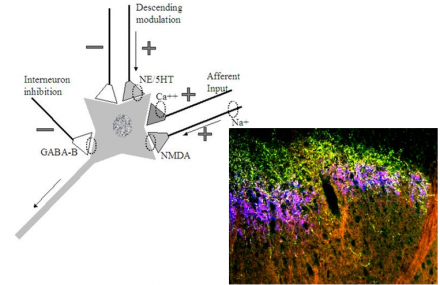
Modulation of Pain by Neuromodulating Agents
Image
Treatment of Neuropathic Pain
- The current state of neuropathic pain treatment is not satisfactory
- It is estimated that over 2/3 of patients do not obtain sufficient pain relief
- Existing treatments do not fully target suspected pain-generators
Reference
Pain 2011;152:2204-5
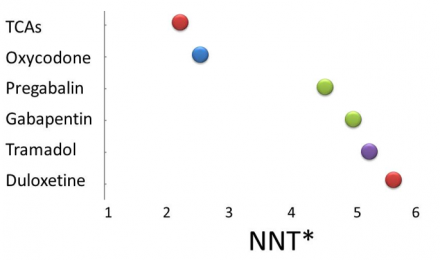
Neuropathic Pain is Difficult to Treat
Image
Reference
Adapted from Wong, 2008; Chong 2007, and other sources.
Neuropathic Pain Guidelines
- Guidelines generally concur that TCAs and gabapentin are first line agents: e.g. post-herpetic neuralgia, diabetic neuropathy, central neuropathic pain.
- Selective noradrenergic reuptake inhibitors (SNRIs) are generally recommended as first or second-line agents
- Opioids mostly 3rd line agents, after other agents have been tried.
- Local anesthetics may be used in topical preparations, e.g. patch or cream
Reference
*Canadian, European and IASP NeuPSIG
Guidelines: Diabetic Peripheral Neuropathy
- Pregabalin should be offered for the treatment of painful diabetic neuropathy (PDN) (Level A)
- Gabapentin and sodium valproate should be considered for the treatment of PDN (Level B)
- Amitriptyline, venlafaxine, and duloxetine should be considered for the treatment of PDN (Level B). Data are insufficient to recommend one of these agents over the others.
- Venlafaxine may be added to gabapentin for a better response (Level C)
- Morphine, tramadol, oxycodone, dextromethorphan should be considered
Reference
Neurology 2011;76:1–1
Gabapentinoids
Gabapentin
- Originally developed as an anti-convulsant
- Inhibits calcium influx through the a2d calcium channel sub-unit
- Among the first-line drugs for neuropathic pain
- Good safety profile; minimal drug-drug interactions
- May start at 300 mg/day or 100 mg/day for elderly
- QHS dosing during first week may minimize complaints of dizziness
- Wide dosing range: 600 – 3600 mg daily, divided doses
- renal dosing adjustment may be necessary
- Half-life means 3X/daily dosing is optimal
Pregabalin
- Inhibits calcium influx through the a2d calcium channel sub-unit
- Among the first-line drugs for neuropathic pain
- FDA approved for painful diabetic neuropathy and PHN
- May have quicker onset of action compared to gabapentin
- May be associated with dizziness, sleepiness, ankle edema, weight gain
- Schedule V controlled substance: mild euphoria reported in some patients during clinical trials
- Twice daily dosing, more convenient for some patients
- Begin as 50mg tid or 75mg bid
- May require renal dosing
Pain-Active Anti-Depressants
- Evidence is best for tricyclics (TCAs)
- Selected SSRI/SNRIs antidepressants may have more favorable side effect profile
- Proven efficacy for various forms of neuropathic pain
- Treatment effects begin after a delay that ranges from 1 week (desipramine), to two weeks or longer.
- Tricyclics generally require lower doses for efficacy against pain, compared with the treatment of depression. By contrast, newer SNRIs require treatment at standard antidepressant doses to be effective against pain.
Tricyclic Antidepressants
TCAs
- Long track record of efficacy against neuropathic pain
- Adverse effects range from:
- Life threatening at higher doses (QT prolongation)
- Dangerous: glaucoma, urinary retention
- Bothersome: dry mouth leading to accelerated dental decay
- Potentially useful: sedation with amitriptyline can be helpful to patients with delayed sleep onset due to night-time neuropathic pain
- Drug interactions (P450 2D6) need to be checked
- Not generally subject to abuse
- Due to cardiac profile, screening EKG recommended for those with cardiac history or over 50 prior to initiation of therapy.
Reference
Pain 2011;152:2206-2210
TCAs
- Amitriptyline
- Most sedating TCA (profound sedation, helpful for night-pain)
- Severe dry mouth may lead to accelerated tooth loss, requires a plan for dental care
- Highly effective against neuropathic pain,
- May be effective at doses as low as 10 mg QHS
- may be safely used for long periods of time
- Nortriptyline
- Prodrug, metabolized to amitriptyline
- Favorable side effect profile although constipation, urinary retention and sexual dysfunction may occur
- Desipramine
- Least sedating, causes tachycardia in some patients
Duloxetine: Pain-active SNRI
- FDA approved for painful diabetic neuropathy, chronic musculoskeletal pain and fibromyalgia as well as major depressive disorder and generalized anxiety disorder
- Side effects can include – nausea, somnolence, urinary hesitancy, seizures, withdrawal syndrome, serotonin syndrome, suicidal ideation, headache
- CYP1A2 inducers decrease effect
- Dose: can start at 30 mg/day and increase to 60 mg/day, doses can range as high as 120 mg/day under appropriate supervision
- Compared with TCAs, patients are somewhat less likely to attain a clinically significant benefit, the NNT is 5.3-6
Venlafaxine: Pain-active SNRI
- Demonstrated to be effective for the treatment of neuropathic pain, moderate effect size
- FDA approved for the treatment of major depressive disorder
- Side effects include headache, hypertension, nausea, constipation, seizures, somnolence
- Serotonin syndrome may be prominent. In addition medication cessation syndrome may occur as well, gradual tapering on and off is recommended.
- Treatment can start at 37.5mg bid or 37.5mg daily
- Max dose: 225mg daily
- Extended release formulations may be better tolerated
- NNT 3.1-5.2
Reference
Pain 2007;132:237-251, 2011;152:2206-2210
Opioid Analgesics
- Opioids have been shown to be effective against neuropathic pain in RCTs (PHN, PDN)
- Guidelines generally recommend opioids as third line agents however prescriber discretion is permissible, e.g. for those patients unable to tolerate, or allergic to first and/or second line agents
- Opioids have established side effect profiles that may exacerbate underlying syndromic problems, e.g. constipation in those with peripheral neuropathy
- Opioids have a complimentary mechanism of action and can be used in conjunction with other neuromodulating agents in appropriate clinical settings
Other Neuromodulating Agents
Tramadol
- Synthetic, centrally-acting analgesic: reuptake inhibition of NE and serotonin, in addition, a major metabolite is an opioid agonist
- Published trials in PDN and polyneuropathy
- Adverse effects include nausea, diarrhea, constipation, dizziness, somnolence, orthostatic hypotension, seizures, serotonin syndrome
- Often well-tolerated and quite effective
- Dose ranges from: 50-400mg/day, typical starting dose: 50 mg twice daily
Lidocaine
- Lidocaine Patch 5%
- Shown to be effective in patients with PHN (RCTs)
- Minimal blood levels of lidocaine
- Patch must be worn 12 hours on, 12 hours off
- Mild skin reactions can occur
- Patches may be cut and tiled, with oversight
- Lidocaine cream
- Lidocaine and other neuromodulating agents can be compounded into creams and topical preparations
- A reputable compounding pharmacist should be contacted directly by the prescriber.
Clonidine
- α-2 Adrenergic agonist
- nonspecific analgesic effects at the dorsal horn
- FDA approved for cancer pain via epidural administration
NMDA-Receptor Antagonists
- Ketamine: widely used in children, also used in management of polytrauma, dissociative anesthetic; generally administered in combination with midazolam I.V.
- Dextromethorphan: most widely used as an antitussive; occasionally used as an adjunct to other pain therapies. Effects demonstrate rapid tachyphylaxis, generally not appropriate to pain management in a primary care setting.
Summary
- There are multiple agents that are effective against neuropathic pain, however no single agent has been proven completely effective and therapy must be individualized.
- Selected anticonvulsants are effective against neuropathic pain, the gabapentinoids have been highlighted here as well tolerated and generally recommended for the treatment of neuropathic pain
- Selected antidepressants are effective against neuropathic pain, these include several of the tricyclic antidepressants and some of the SNRIs.
- Other agents are known to be effective against neuropathic pain in selected patients and therapeutic trials can be undertaken by experienced practitioners.

