Acute Pain
- Opioids are a mainstay of therapy for the relief of iatrogenically induced pain. Modern surgery would not be possible without readily available opioids for peri-operative and post-operative pain management.
- Opioids are highly effective for acute pain. One study of acute pain management, utilizing titration to determine dosing, concluded that the NNT for morphine for acute pain relief was less than 1.1, meaning that morphine is nearly universally effective. This compares with an NNT of 5.5 for most chronic pain medications.
Cancer Pain
- Opioids are an essential element of therapy for the relief of cancer pain. Most patients with cancer receive opioids at some point in their course of care.
- Opioids are very effective for cancer pain. One limitation is that cancer pain often persists for weeks, months or years. The doses and types of opioids often require adjustment to maintain efficacy.
Utilization of Opioids
Utilization of opioids is increasing the U.S.
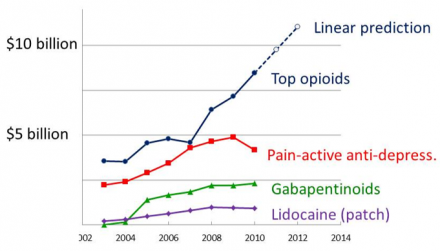
Reference
Data in part from: Pain & Policy Studies Group, University of Wisconsin .
Chronic Non-Cancer Pain
- Approximately 20% of the industrialized world suffers from persistent pain.
- Productivity is decreased and costs to employers for those with pain are 2X as high as those without.
- The leading causes of disability are arthritis and spine pain, accounting for 34% of disability in the U.S.
- The efficacy of opioids for chronic pain is well established but the balance of risks and benefits is distinct compared with acute and cancer pain conditions.
Opioid Analgesia (Efficacy)
Opioid analgesia (efficacy) decreases with persistent exposure.
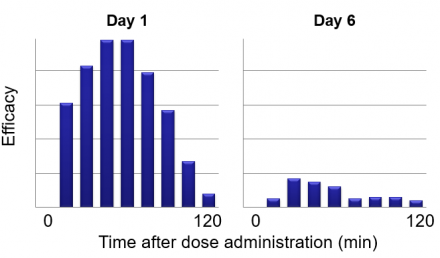
Reference
Data from: Mutsumi Ueda Mechanisms underlying morphine analgesic tolerance and dependence. Frontiers in Bioscience 14, 5260-5272, June 1, 2009.
Tolerance
A state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more effects over time.
Physical Dependence
A state of adaptation manifested by a drug class-specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist.
Physical dependence means that withdrawal symptoms will occur if drug levels in the body decrease. It is not equivalent to addiction, it is distinct from psychological dependence. Abrupt cessation of opioids produces a very unpleasant withdrawal syndrome: abdominal pain, diarrhea, sweating, myalgias, etc.
Indications for Opioids in Chronic Non Cancer Pain (CNCP)
"Clinicians may consider a trial of COT as an option if CNCP is moderate or severe, pain is having an adverse impact on function or quality of life, and potential therapeutic benefits outweigh or are likely to outweigh potential harms (strong recommendation, low-quality evidence).”
Reference
Clinical Guidelines for the Use of Chronic Opioid Therapy in Chronic Noncancer Pain, American Pain Society/ American Academy of Pain Medicine, 2009.
Benefits
- Opioids are not a panacea for chronic pain, most often it is reasonable to expect a reduction of pain of 2-3 points on VAS of 10, in response to opioids for chronic pain.
- May be appropriate in some difficult to treat populations.
- In a study of 54 SCI patients with chronic pain unresponsive to anticonvulsants alone, pain intensity decreased 7.1 point decrease in VAS with oxycodone.
Risks
- Prescription drugs abuse is a major cause of death in young adults, opioids are a huge part of this.
- Even in the absence of abuse, physical dependence will occur with prolong use.
- Constipation can be life threatening if not anticipated and treated aggressively.
- Opioids can suppress breathing, cause sedation and interfere with cognitive and sexual functioning.
- Opioids may be subject to diversion by others who come into contact with your patient.
Realities
Opioids may only be used as part of a comprehensive treatment plan.
In the case of chronic non-cancer pain this means:
- An established diagnosis or working differential diagnosis
- An established opioid safety plan (treatment contract)
- A comprehensive treatment plan that includes additional treatments which complement the action of opioids
- Pharmacological adjuncts: NSAIDs, etc.
- Non-pharmacological treatments
- cognitive behavioral therapy
- acupuncture
- physical therapy, etc.
Alternatives and Adjuncts
Think about the alternatives and adjuncts.
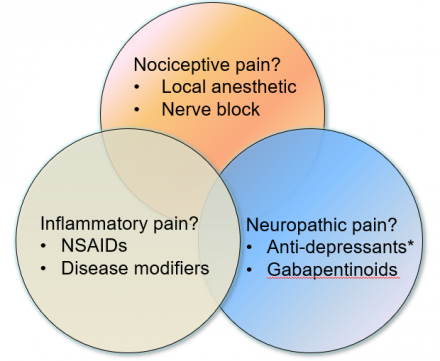
Balance Risks and Benefits
Balance risks and benefits of all components of therapy.
Remember that all pharmacological therapies have side effects that may limit therapeutic efficacy.
- NSAIDs: increased risk of cardiovascular events and GI bleeding
- Tricyclic anti-depressants: anticholinergic effects predominate: severe dry mouth, urinary retention, cardiac effects
- Gabapentinoids: cognitive impairment and dizziness
Chronic Pain Needs Treatment
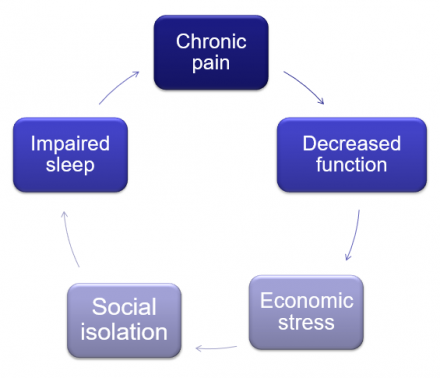
Medication is Only One Component
Medication is only one component of a multimodal, comprehensive treatment plan.
- Medication
- Physical therapy
- Massage/acupuncture/manual therapy
- Clinical psychology: cognitive behavioral therapy, etc.
- Life style modification
- Surgery or interventional care
Summary
- There are multiple indications for the use of opioids in the management of pain. It is important to make sure that opioids are used only when indicated and necessary
- Patients develop tolerance to opioid analgesia and also physical dependence on opioids when exposure is sustained over more than a few days.
- Opioids must only be used as part of a comprehensive treatment plan, that ideally includes both pharmacological and non-pharmacological approaches.

