Mrs. Christine Farley has been suffering from temporomandibular joint (jaw) and myofascial (muscular) pain, and you are asked to be part of her inter-professional team to advise on how to best help manage her pain.
You are part of an inter-professional team composed of health care specialists from the following disciplines:
- Medicine
- Dentistry
- Pharmacy
- Nursing
History and Presentation
Mrs. Farley arrives to see you for help with managing her chronic pain. Please watch the video to review her history and presentation.
Review of Mrs. Farley’s Physical Exam
Vital signs
Blood pressure 124/78, Heart Rate 82
General
Well-appearing female in no distress
Oral Exam
Oropharynx clear. Vertical range of motion (ROM) of her jaw without pain increase was 33 mm, she can open to 43 mm with pain bilaterally in her temporomandibular joints (TMJs) and cheeks (masseter muscles). Adequate lateral ROM of 6mm bilaterally with pain in her TMJ's and masseter muscles. Her palpation exam significant in that she is sensitive to palpation of her masticatory muscles bilaterally including the superficial masseter, anterior and middle temporalis, medial pterygoid muscles. Palpation of these areas aggravates jaw pain and her headache. Her TMJ and jaw pain best duplicated by palpating her deep masseter muscles especially on the right side. She has deep masseter and TMJ pain with having her clench her teeth.
Cardiovascular
Regular rate and rhythm
Lungs
Clear
Abdomen
Soft, non-distended, no masses
Extremities
Warm, mild tenderness in bilateral upper extremities (biceps, triceps, and forearm)
Skin
No rashes
Musculoskeletal
Strength intact in upper and lower extremities, full range of motion of all major joints
Neck Exam
Full range of motion of her neck with mild pain with neck extension. Pain with palpation of bilateral paraspinal muscles, splenius capitis, and trapezius.
Back Exam
Full range of motion of her back with mild pain with lateral rotation and extension. Diffuse pain with paraspinal palpation at thoracic and lumbar levels.
Neurological
Alert and oriented. Slightly depressed affect. Cranial nerves intact. Sensation intact to light touch. Normal gait. Mild pain over bilateral occipital ridges. 2+ brachial and patellar reflexes
Temporomandibular, Mouth, and Head and Neck Exam
The video shows Mrs. Farley's temporomandibular, mouth, and head and neck exam.
Mrs. Farley’s Imaging Studies
Panorex radiograph does not reveal any pathology of the maxilla or mandible. The osseous contours of the TMJs are normal bilaterally with smooth, well-defined outlines of the condylar eminence and fossa. Joint spaces are well-maintained.

MRI of her neck and back were essentially normal with some mild degeneration in her cervical spine.

Assessing Mrs. Farley’s Pain
A Review on Questions to Ask a Patient with Pain
When assessing a patient’s pain, it is important to ask certain questions to get a full understanding of the patient’s pain history. There are different methods you can use to remember the important questions to ask. One option is the pneumonic “OPQRST.”
O – Onset: When did the pain start? What was happening at that time?
P – Palliative and Provocative factors: What makes the pain better? Worse? (Include specific activities, positions, or treatments.)
Q – Quality: Describe the pain. Is it burning, sharp, shooting, aching, throbbing, etc.?
R – Region and Radiation: Where is the pain? Does it spread to other areas?
S – Severity: How bad is the pain? (There are several scales to use; these will be discussed in the following slide.)
T – Timing: When does the pain occur? Has it changed since onset? If so, how?
Reference
Powell RA, Downing J, Ddungu H, Mwangi-Powell FN. Pain Management and Assessment. In: Andrea Kopf NBP, editor. Guide to Pain Management in Low-Resource Settings. Seattle: IASP: International Association for the Study of Pain; 2010. p. 67-79
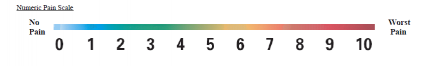
Numeric Pain Rating Scale
You can also ask her what her pain is from 0 to 10 on a numeric rating scale.
There are several different scales that can be used to assess pain severity.
The most common is the 11-point Numerical Rating Scale (NRS), which uses the range 0-10. The benefits of the NRS are its simplicity and validity. Possible drawbacks include response variability and moderate correlation with functional status.
Effective Assessment and Reassessment of Pain
Screen
Ask are you experiencing any discomfort right now?
- If No: document “zero” pain and reassess periodically
- If Yes: ask about its nature (verbal description) pattern (over time) and location
Try to quantify the intensity of the pain. Show the patient the rating tools we use, and determine which one is easiest and most meaningful to them.
Starting with the NUMERIC PAIN SCALE
It is important to recognize that this is an 11-point scale (0-10 not 1-10).
Ask the patient if they would recognize:
- if the discomfort were completely gone (“rating of 0”)
- or the worst they or anybody else could possibly experience (“10”)
Have the patient rate the intensity of their pain/discomfort “right now” verbally with a number or by pointing to the number that represents their pain intensity.
Once the patient understands this scale, follow-up questions may be asked without the visual aid:
“On a scale of 0 to 10, how much pain (or discomfort) are you experiencing now?”
Verbal Descriptor Scale
If that is not easy and meaningful, use the Verbal Descriptor Scale.
Determine if discomfort is “None” (chart 0) or the worst possible (chart 10).
Ask if the discomfort or pain is mild, moderate, severe, or extreme.
- Record 2 (for mild), 4 (for moderate), 6 (for severe), or 8 (for extreme) accordingly.
- If the patient reports it is between 2 words, select the odd number between them
- (e.g., when the patient reports the pain to be between mild and moderate, the score =3).
Functional Pain Scale
If that is not easy and meaningful, use the Functional pain scale.
- Determine if discomfort is “None” (chart 0) = 0
- Determine if it is tolerable (“<5”) or intolerable (“>5”)
- Tolerable pain that does not interfere with activities = 2
- Tolerable pain that interferes with physically demanding activities = 4
- Intolerable pain that interferes with physically demanding activities = 5
- Intolerable pain that interferes with active but not passive activities = 6
- Intolerable pain that interferes with passive activities (e.g., reading) = 8
- Pain so severe the patient can’t do any active or passive activities = 10 (can’t even talk about pain without writhing/screaming)
4 A's Determining Safety and Efficacy of Therapy
Reassess using the 4-A’s determining safety and efficacy of therapy.
Analgesia
To what extent did the treatment reduce the pain and make it more tolerable? This can be evaluated by using one of the pain intensity scales above, the percent the pain intensity is reduced by (e.g., 30%, 50%, etc.), or adjectives (good, excellent effect) the patient uses.
Activity
- To what extent did the patient’s activity and rest patterns improve as a result of the treatment? Does pain interfere less with usual and prescribed therapeutic (e.g., physical therapy) activity. Does pain interfere less with sleep? Does the treatment affect safety?
Adverse Effects
What side effects, toxicity, technology-related complications are experienced?
Aberrant Behaviors
Has the medication affected medication-focused behaviors or personality?
Additional Assessment Tools
Faces Pain Scale
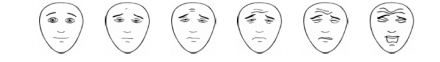
The Faces Pain Scale can also be used for any patient, but it is especially useful with children or non-verbal patients. This is a well-studied and validated scale.
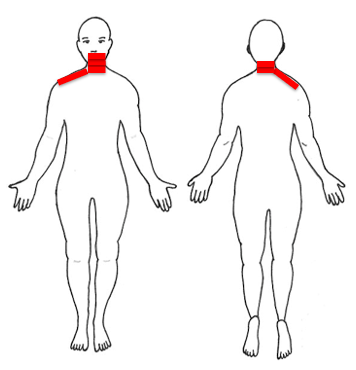
A body diagram can allow patients to pinpoint their pain site(s) to help guide your examination.
Additionally, observing patients when they move or during the exam is a useful addition to these scales and is essential with young children and non-verbal adults.
Learn more at https://www.iasp-pain.org/
Body Diagram Example
Patient is asked to mark where they experience pain.
Example Assessment for Mrs. Farley
This is a 36-year-old female with a history of depression and headache who is referred for evaluation and treatment of her temporomandibular disorder with myofascial and neuropathic pain components in addition to full body myofascial pain that may be secondary to fibromyalgia. Her pain has greatly affected her mood and her ability to work and participate in the activities she enjoys. She has tried opioids and muscle relaxants in the past with some relief of her symptoms. She occasionally takes ibuprofen and Fiorcet, which help her headaches. She presents with some risk factors for opioid misuse including using her relative’s opioid medications and current depression. She has not recently tried physical therapy or other alternative treatments besides massage. She is not undergoing regular psychological care.

