Meet Allison Tatum

Ms. Tatum is a 30 year-old woman with a history of opioid use disorder (heroin and fentanyl) who has been treated for 2 months with buprenorphine/naloxone (Suboxone) in a substance use disorder treatment program.
Understanding Addiction
Addiction is a disease, not a moral failing.
Substance use disorder is defined as a problematic pattern of substance use leading to clinically significant impairment or distress manifested by clinical criteria (DSM-V).
The terms addiction and substance use disorder are equivalent and accepted diagnostic terms.
Appropriate language by providers is paramount. Stigmatizing terms such as “addict”, “abuse”, “habit” and “user” are demeaning, deny the medical nature of the disease, and may negatively impact care.1-2
Opioid use disorder is defined by impaired control, social impairment (e.g. failure to meet major work, school, or home responsibilities), risky use, and other medical criteria for substance use disorder.3
References
- Kelly JF et al. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int J Drug Policy 2010; 21(3):202-207.
- Wakeman SE, Barnett ML. Primary Care and the Opioid-Overdose Crisis – Buprenorphine Myths and Realities. NEJM 2018; 379(1):1-4.
- https://www.samhsa.gov/disorders/substance-use
Opioid Use Disorder (OUD) Treatment Principles
Not one strategy or modality alone will treat OUD.
A multidisciplinary, team-based approach guarantees the best success for treatment. This may include:
- Counseling services, behavioral medicine
- Peer support
- Medication management
- Co-management of psychiatric illness
Possible treatment locations may include
- Outpatient (e.g. counseling, medication management visits, group support visits, peer support, etc.)
- Intensive outpatient treatment programs (IOPs)
- Inpatient and residential treatment programs
"Detox" Versus Medication Management
- Traditional “detoxification” or abstinence-based programs alone have not been shown to be effective in treating opioid use disorder and may even increase the likelihood of overdose death by eliminating tolerance in a patient.1
- Medication management using buprenorphine/naloxone or methadone, for instance, is not a “replacement” but rather a daily pharmacologic treatment for a chronic disease, like what is needed to treat diseases such as diabetes or asthma.
- The medication management of OUD is associated with decreased illicit opioid use and recurrent use, increased treatment engagement, and decrease in mortality.2-4
References
- Wakeman SE, Barnett ML. Primary Care and the Opioid-Overdose Crisis – Buprenorphine Myths and Realities. NEJM 2018; 379(1):1-4.
- Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med. 2014;370:2063–2066.
- Nielsen S, Larance B, Degenhardt L, Gowing L, Kehler C, Lintzeris N. Opioid agonist treatment for pharmaceutical opioid dependent people. Cochrane Database Syst Rev. 2016:CD011117.
- Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550
Medication Management for OUD
In conjunction with her provider and discussions about goals of care and appropriate treatment, Alison was started on buprenorphine/naloxone
Goals of therapy
- Minimize harms from ongoing use
- Reduce or eliminate OUD symptoms (withdrawal, cravings)
- Provide protection against risk of overdose and death
- Improve physical and psychological health
- Initiate long-term recovery
Followup with Ms. Tatum and Her Medication Management
Alison has a follow-up appointment with her doctor to review her progress and medication management.
Indications for Outpatient Medication Management for Opioid Use Disorder
General indication
- For any patient with a history of opioid addiction
Drug-specific indications
- Buprenorphine/naloxone – discussion to follow
- Methadone – patient meets criteria for an opioid treatment program (OTP)
- Diagnosis of opioid addiction
- History of at least 1 year of opioid addiction before admission
Naltrexone
- Prevention of return to opioid dependence following medically-supervised opioid withdrawal
- Adequate period of abstinence with no signs of opioid withdrawal
- Willing to receive monthly IM injections
Comparison of Medical Management for OUD
|
|
Methadone |
Buprenorphine |
Naltrexone |
|
Mu-opioid receptor activity |
Full agonist |
Partial agonist |
Full antagonist |
|
FDA-Approved Formulations |
Oral solution, dissolvable tablet |
Transmucosal buprenorphine/naloxone (Suboxone, Bunavail, Zubsolv) Injectable buprenorphine (Probuphine, Sublocade) |
Oral tablets, Extended-release IM injection (Vivitrol) |
|
Dosing |
Oral: 20-30 mg once daily; titrated up to 80-120 mg once daily as tolerated |
Transmucosal: typically dosed 8-16 mg (or equivalent) once daily (or in divided doses) Probuphine (for patients maintained on ≤ 8 mg/day): 1 dose (4 implants) for 6 months Sublocade (for patients maintained on ≤ 8 mg/day): 300 mg subcutaneous injection monthly for 2 doses then 100 mg monthly |
Oral: 25 mg on day 1 then 50 mg daily Vivitrol: 380 mg IM every 21-28 days
Dose IM 7-14 days after last opioid dose to prevent withdrawal |
|
Setting |
Licensed outpatient treatment program |
Any medical setting; X waiver required |
Any medical setting |
|
Additional benefits |
Use in co-morbid pain, high potency, high structure of delivery setting |
Safety compared to methadone, use in co-morbid pain, dosing flexibility, less structured treatment setting |
Low diversion, no physical dependence, verifiable dosing, less stigma, less structured treatment setting |
Buprenorphine/Naloxone Pharmacology Review
Buprenorphine
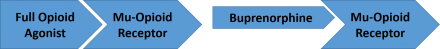
- Buprenorphine is a partial mu-opioid receptor agonist and kappa-opioid receptor antagonist
- Binds to the mu-opioid receptor and produces only a partial response
- Activity at the receptor reaches a plateau where increased doses do not result in increased activity; ceiling effect on respiratory depression
- Blocks effects at the kappa-opioid receptor, which in theory may be associated with reducing dysphoria, depression, and stress responses
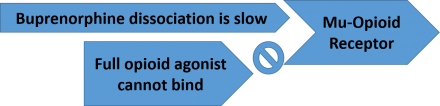
- Buprenorphine has strong affinity for the mu-opioid receptor and will displace full agonists like heroin

- Buprenorphine dissociates slowly from the mu-opioid receptor and has a long elimination half-life (24-42 hours). It is typically dosed once per day but can also be dosed two or three times per day depending on the clinical scenario.
- Buprenorphine/naloxone transmucosal products are abuse-deterrent formulations
Naloxone
- Naloxone is a short-acting opioid antagonist that is poorly-absorbed when administered via the oral, sublingual, or buccal routes
- Induces withdrawal in patients that are physically dependent on opioids
- Addition of naloxone to buprenorphine formulations reduces the potential for misuse
- Mitigates the effects of buprenorphine if the formulation is manipulated (e.g., crushing tablet for snorting or injecting)

