September 2nd: Missed Party
September 22nd: Benched
September 28th: Math Test
October 3rd: About Math Class
October 9th: No School!
October 12th: Volleyball Boosters
October 16th: Social Studies
October 27th: Coach's Concern
October 31st: Excedrin
November 2nd: Picking Beth's Brain
November 8th: Mom's Purse
November 21st: Pharmacy Visit
Awareness
- The pharmacist is aware of a patron's buying habits
What to consider in Morgan's case:
- Number of headaches per month
- Is she well managed on her acute, OTC therapy?
- What impact are the headaches having on Morgan's life?
Headache Characteristics
- Throbbing pain
- Right sided behind eye
- Triggers
- Stress
- Lack of rest
Medication Overuse Headache
- Occurs when medications used to treat acute headache are taken too frequently (>15 doses/month)
- Common cause of chronic daily headache
Reference
Cortical hyperexcitability and mechanism of medication-overuse headache
http://cep.sagepub.com/content/30/9/1101.long
Pharmacist's Recommendation
Description of headache location and severity suggests migraine and the pharmacist recommends seeing Morgan's physician.
November 22nd: After Pharmacy Visit
November 22nd: Thanksgiving and Black Friday
November 26th: No More Medicine!
November 27th: Nurse Practitioner Appointment
Past Medical History
- Cyclic vomiting otherwise well except for headaches
- Vomiting treated with cyproheptadine
Family History
- Migraine and anxiety in mother and maternal grandmother
Stressors
- Wanting to do well in school, softball and volleyball, and drama
- After school activities up to twice a day including weekends
Headache Characteristics
- Location
- Quality
- Exacerbating factors such as stress at home and school
Interaction with School
- School nurse sends her home
- Misses class
- Cannot attend sports practice
- Worries about getting a headache in school so stays home
November 27th: Neurologist Appointment
Multiple interviews can often uncover information such as Morgan’s use of her mothers pain medication without mothers knowledge
Characteristics of Morgan’s Migraine
- Genetic component to migraine
- Nausea associated with headache
- Throbbing one-sided pain
Cautions about caffeine
- Caffeine is in some OTC medications used to treat migraine (ex. Excedrin migraine)
- Caffeine is also common in energy drinks
- Too much caffeine can make migraines worse and disrupt sleep
Physician Recommended Therapies
- Magnesium (supplement)
- Riboflavin (vitamin)
- Maxalt® (triptan)
- Taken at first sign of headache/aura
- Amitriptyline (anti-depressant)
- Preventive, taken daily, sedating
- Migrelief (magnesium, riboflavin, feverfew)
- Preventive
Feverfew

- Tanacetum parthenium
- Chrysanthemum species
- MOA: unknown
- Conflicting data regarding efficacy
- Several pain/inflammatory pathways have been studied without definitive results
- Avoid in pregnancy: risk of uterine contractions
- Avoid in breast-feeding: limited data
Addressing Triggers
- Low blood sugar: eat breakfast, snack every 2-3 hours
- Dehydration: Carry water bottle, urine should be pale color
- Sleep deprivation: Make restful sleep a priority, consider melatonin
- Stressors: Learn relaxation techniques
Relaxation Techniques
- Deep breathing
- Yoga
- Cognitive behavioral therapy (CBT)
- Headache diary (identify triggers)
- Acupuncture
November 27th: Nurse Practitioner Notes
Smith, Morgan
MRN: #######
♀ Female, 14 y.o. 4/4/2003
Weight: 48.5 kg (106 lb 14.8 oz)
Phone: (585) 555-5555
PCP: Brown, Mary, MD
Status: Active
Morgan Smith
Date: 11/27/2017 at 10:56 a.m.
Marina R. Connolly, MD → Lesley L. Jones, MD
Cc: Kayla Hunt, PsyD; C. Grayson, PNP
I had the pleasure of seeing your patient, Morgan Smith, in the Golisano Children's Hospital at Strong Child Neurology Headache Clinic today for evaluation of her headaches. Morgan was accompanied by her mother who contributed to the history.While you are familiar with this patient, please allow me to review their history for my edification and records. As you know, Morgan is a 14 year old, right- handed female with a history of cyclic vomiting that began at age 5 and has now transitioned to a more classic migraine presentation. She was relatively symptom free until one year ago when she began to complain of headaches. The headaches began to worsen over the past 6 months after sustaining a concussion while playing volleyball.
Onset of symptoms
Cyclic vomiting from age 5 through 10. She was followed by Child Neurology and Pediatric GI during that time. Her episodes were managed prophylactically with Cyproheptadine and acutely with Ondansetron and Benadryl. She has had several ED amissions due to dehydration during her more intense episodes. She presents today with gradually increasing frequency and intensity headaches over the past 6 months. She has had recent complaints of stomachache with burning sensation. She has had multiple visits to the school nurse for prn analgesics for headache management. The school nurse frequently sends her home instead of allowing her to rest in the office and then go back to class.
Frequency, Timing, and Duration of Headaches
Headaches occurring 2-3 days per week at random times and last from 3-4 hours up to all day until she goes to bed at nightl. Intensity: Majority of her headaches have an intensity level reported at 7-9 on a scale of 1-10. She doesn't feel that she has ever really had a 10/10 headache. Most headaches cause her to cease activity and are now interfering with school attendance and ability to participate in activities, sports, and social events with friends.
Description/Quality of pain
Unilateral, right-sided temporal throbbing pain. She also endorses sharp pain and feeling of fullness behind her right eye.
Prodrome/Aura
Endorses feeling irritable the day prior to headache onset. She states that she experiences left-sided numbness in her lips and tongue approximately 10 minutes prior to headache onset at times. She also experiences left-handed tingling in her fingers, occasionally has difficulty "getting the words out" just prior to headache onset.
Associated symptoms
Nausea, no vomiting, photophobia, phonophobia.
History of previous head trauma/concussion
Concussion approximately 6 months ago while playing volleyball-spike ball to the head. Headaches began to worsen since.
Triggers
Sleep deprivation, stress, overscheduling, possibly dehydration.
Menstrual cycle
normal monthly cycle.
Appetite
Healthy diet, but skips breakfast frequently during the school week. Irregular eating pattern due to school/activities schedule. No significant changes in weight.
Hydration
Primarily drinks water. Caffeine intake 2-3 times/week (iced coffee beverages). She doesn't carry a water bottle at school. She reports drinking approximately 24 oz/day. She also drinks energy drinks 2-3 times/week in the afternoons prior to her activities. She reports that the energy drinks have vitamins in them and believes them to be healthy.
Sleep pattern
Goes to bed at 10:30 pm each night during school year. She has late nights trying to get her school work completed after her numerous extracurricular activities that take place in the evening. It often takes her 1 to 1-1/2 hours to fall asleep. She states that she lies in bed and just can't fall asleep as she is thinking of all that she needs to do the next day. She awakens at 6am for school.
Mood
Escalating level of anxiety due to feeling overwhelmed, pressured, and overscheduled. Occasionally feels "panic" and worries that this will happen to her when she is at school. This has led to some occasional school absences.
School/extracurricular activity days missed due to headache
7-8 full days since September, some late arrivals or early departures. Increased frequency of absences over the last 6-9 months. She also admits to using her mother's prescription for Tylenol with Codeine (mom unaware). She also tries cool compresses when she has a headache.
Current Acute Headache Medication/Treatments
Using Excedrin migraine on an almost daily basis. She takes been taking 1-2 doses/day for the past 3 months.
Current Preventative Headache Medication
none
Previous Headache Evaluation (Imaging, Labs, Other Testing)
none
Date of last Ophthalmologic Exam
two months ago-dilated exam-reported as normal.
Other specialists involved in Morgan's care
n/a
Past Medical History
Cyclic vomiting syndrome, anxiety, seasonal allergies
Social History
9th grade in high school. She has excellent grades (high honor roll/high achiever). She participates in softball and volleyball (school and travel), drama, singing, dance, and plays guitar. She also goes to an after school homework program which is used to provide a structured, quiet, proctored environment in which to complete academic work and receive extra help if needed. She lives with mom, dad, and younger sister.
Family History
Migraine: mom, MGM, maternal aunt.
Fainting episodes: mom
Anxiety: mom, dad, MGM.
Current Medications
Excedrin migraine
Allergies (drug, environmental, food or latex)
none reported
Review of Systems
A 10 point review of systems was completed and was negative except for what was mentioned in the HPI.
No reported history of seizures, incoordination, behavior change, nocturnal or morning headaches with emesis, or headache that is worse in recumbent position or with cough/strain.
Focal Neurological Symptoms
Visual: Negative for reduced vision, decreased visual fields, sudden vision loss, or diplopia.
Vestibular: Negative for loss of coordination or imbalance.
Auditory: Negative for difficulty hearing or tinnitus.
Motor: Negative for paralysis, unilateral weakness, loss of muscle control, increased muscle tone, loss of muscle tone, or involuntary movements.
Sensory: Negative for paresthesias, numbness or changes in sensation.
Mental Status: Negative for confusion, disorientation
Speech/Swallow: Negative for aphasia, dysarthria, poor enunciation, poor understanding of speech, impaired ability to read or to understand writing. No reports of swallowing difficulty, or choking.
Physical Exam
General Appearance: Well-appearing, well-groomed, no acute distress
Lungs: clear to auscultation
Cardiac: regular rate and rhythm, no murmurs
Extremities: No deformities noted
Skin: No significant birthmarks noted
Neurologic Examination:
Mental Status: Awake, alert and oriented. Attention was normal. Speech was intelligible.
Language: Appropriate for age
Cranial Nerves:
II: Visual fields full to confrontation
III, IV and VI: EOMs full in all directions of gaze. No nystagmus.
V: No facial sensory loss.
VII: No weakness of facial muscles.
VIII: Hearing intact.
IX and X: Palate elevates symmetrically.
XI: Normal shoulder shrug
XII: Tongue bulk and strength normal
Motor: Normal tone and bulk throughout. 5/5 strength throughout all major muscle groups tested. Good finger to nose coordination.
Involuntary movements: None noted
Muscle stretch reflexes: 2+, symmetric throughout with flexor plantar responses
Sensation: Intact to touch in all extremities
Coordination: No appendicular or truncal ataxia.
Station/Gait: Casual gait shows normal base. Able to walk on heels and toes and perform tandem walk well forward and back without difficulty.
Assessment
Morgan is a 14-year old female with a history of headaches and associated symptoms consistent with a diagnosis of Migraine with Aura, Tension Type Headache, and Medication overuse headache. Additionally, she exhibits symptoms associated with anxiety/panic. Mom seems to over or misinterpret Morgan's migraine symptoms due to her own history of migraine which often increases Morgan's anxiety level. SCARED rating scales completed and will be shared with psych provider. Mom very concerned and requesting imaging which is not indicated at this time.
Plan
The exam and history make a structural brain abnormality, intracranial hypertension, or subacute bleed unlikely. Based on the history and exam, neurodiagnostic imaging is not necessary at this time.
- Begin Amitriptyline 10 mg nightly for migraine prophylaxis
- Begin Migrelief-1 tablet twice daily for migraine prophylaxis
- Use Rizatriptan 10 mg at onset of migraine for acute management
- Discontinue use of OTC analgesics for 2 weeks; counsel to expect possible withdrawal headache
- Keep track of headaches in a calendar or log to identify possible triggers or patterns.
- Maintain routine patterns of sleeping, eating, and exercise.
- Eat small, healthy meals and snacks throughout the day. Try not to allow more than 3 hours without a snack. Do not skip meals!
- Avoid over-scheduling. Consider decreasing number of extracurricular activities throughout the week to lighten the load.
- Referral to psych for Cognitive Behavioral Therapy (CBT) to promote relaxation, anxiety reduction, coping with pain.
- Educate school nurse about managing headaches at school without sending Morgan home. Provide School Headache Management plan which includes medication consent that allows Morgan to receive prn medication at school.
- Consider alternative and complementary therapies that do not involve the use of medication. They may help to relieve symptoms and prevent migraines. Possible treatment options include biofeedback, yoga, meditation, aromatherapy, cell phone apps for meditation, mood tracking, and mindfulness.
Thank you again for involving me in the care of this patient. More than 50% of this 60 minute visit was spent on face to face discussion of the diagnosis and treatment plan, teaching, counseling and coordination of care.
Please feel free to call or email me any time with questions or concerns about the treatment plan.
Electronically signed by @ME@ @NOW@ @TD@
Division of Child Neurology
Golisano Children's Hospital at Strong
601 Elmwood Avenue, Box 631
Rochester, New York 14642
585-275-2808-phone
585-275-3683-fax
November 27th: School Management Health Plan
(video)
Name of Child: Morgan Smith
School year: 9th Grade
Medical Problem: Headaches
Permission: from parent to discuss care with School Nurse ✔
Current School Management for Headaches
- Student often sent home from school "right away"
- Limited resources in school nursing office
- Morgan unclear about ability to self-manage
Student's Symptoms of Migraine
Headaches in this student typically include:
- Moderate to severe pain
- Photophobia, phonophobia
- Nausea, but no vomiting*
- Aura (numbness, tingling, trouble speaking)
*Vomiting would require being sent home by school protocol
Recommended Treatment
At the onset of a headache, Morgan should request to go to the nurse's office and be given:
- Medication Name: Maxalt
- Route of Administration: PO
- Tall glass of water/snacks
Notify the parent if: Headache does not respond within 1-2 hours
No Excedrin Migraine
November 28th: Pharmacist Consultation
First Step
- The first step is to determine patient understanding of the reason for taking a medication, the benefits, and the risks
Amitriptyline (Elavil®)
- Tricyclic anti-depressant (TCA)
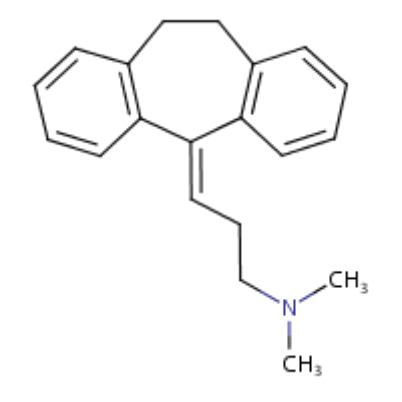
- Preventive
- Morgan's dose: 10 mg/po/at bedtime
- AE: sedation, xerostomia
- ½ life: 13-36 hr
Major Psychiatric Warning
- Suicidal thinking/behavior: Antidepressants increase the risk of suicidal thinking and behavior in children, adolescents, and young adults (18 to 24 years of age) with major depressive disorder (MDD) and other psychiatric disorders
- Look for:
- Agitation
- Depression
- Anxiety
Uncommon
Reference
American Academy of Neurology Quality Standards Subcommittee and the Practice Committee of the Child Neurology Society 2004 practice parameter for the pharmacological treatment of migraine headache in children and adolescents
Rizatriptan (Maxalt®)
- Triptan
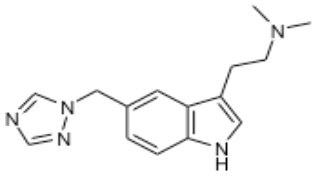
- Acute therapy
- Morgan: as needed as soon as migraine starts
- AE: Triptan phenomenon (rare): chest pain, chest tightness, flushing
Maxalt Potential Side Effect: Serotonin Syndrome
Signs and Symptoms of Serotonin Syndrome
Autonomic Hyperactivity
- Abnormal blood pressure
- In moderate cases, severe hypertension
- In severe cases, hypotension
- In moderate cases, severe hypertension
- Dilated pupils
- Diarrhea
- Fever, diaphoresis, shivering
- Tachycardia, tachypnea, dyspnea
Mental Status Changes
- Agitation, nervousness, hypervigilance, insomnia
- Confusion, agitated incoherent speech, delirium
- Semicoma, coma
Neuromuscular Abnormalities
- Akathisia, mydriasis, impaired coordination
- Myoclonic twitching, tremors, ataxia, rigidity, hyperreflexia, clonus (including ocular clonus)
- Seizure
November 28th: Neurologist?
December 1st: Cognitive Behavioral Therapist
Headache Diary/Thought Log
| Thoughts | Feelings | Cognitive Distortions? | Alternative, Rational Response |
|---|---|---|---|
| (Write down the repetitive thought) | (List any emotions that you feel when thinking those thoughts) | (Is there a cognitive distortion(s) in your thought? If so, write it down; there may be a few) | (Think of a more rational response to your cognitive distortion (CD) and write that here. If there isn’t a CD in your thought, leave this row blank and move on to another example) |
| Example: | |||
| "I know I'm going to fail that exam" | Anxious, discouraged, tense | Fortune telling/Predicting the future | "Actually, I've passed many exams before and I'm pretty confident that if I study enough, I'll do fine”" |
| Morgan: | Morgan: | Morgan: | Morgan: |
| "I will never get into a good college if I keep missing my classes | Scared, nervous, heart racing, tingles in lips and fingers | Predicting the future; all-or-nothing thinking | "There are ways I can make up my work if I miss class." |
CBT: Diagram
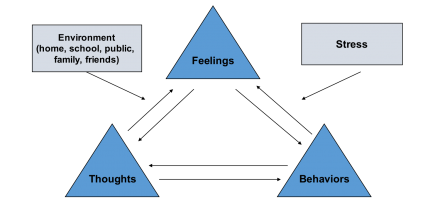
Behavioral Techniques
The therapist demonstrates the Relaxation Strategy of Guided Imagery/Visualization
Close your eyes and experience this segment in the video above.
- Behavioral techniques are often used in conjunction with cognitive techniques (hence the C and B in CBT)
- Behavioral interventions can help target:
- Avoidance
- Physiological symptoms
- Mood
- Motivation
Cognitive Techniques
- Replace or reframe cognitive distortions or maladaptive thoughts with more balanced and realistic thoughts and beliefs about oneself, the future, and the world around us
December 2nd: Therapist?
December 12th: Home Early Again
December 14th: After Neurology Visit
December 15th: Acupuncture?
December 18th: Acupuncture Appointment
Acupuncture Assessment: History
The patient history is considered the most important part of diagnosis in Chinese medicine.
- Inquiry about the chief complaint, its onset and characteristics is critical.
History of Menses
Because the menstrual cycle is considered physiologically important in Chinese medicine a clinician will ask about its characteristics and its relationship to the presenting complaint.
- Pain prior to and during menses suggest stagnation of qi and blood.
- Association of headache with onset of menses suggest qi constraint.
History of GI Function
Early history of cyclic vomiting can be associated with abnormal GI function later in life. Inquiry about bowel movements help in understanding the relationship between the normal qi dynamic (peristalsis and evacuation) and the chief complaint.
- Reduction of headache intensity or resolution upon bowel movement indicates restoration of normal qi dynamic is palliative.
- Loose stool can suggest abnormal GI physiological function due to disruption of qi dynamic.
Acupuncture Assessment: Examination
- Pulses
- Tongue
- Abdomen
Acupuncture Assessment: Pulse Palpation
- The radial pulse is palpated bilaterally to assess rate, rhythm, arterial volume and force, and wave form.
- The index, middle, and ring finger are applied to the artery.
- A specialized vocabulary is used to describe the findings.
Acupuncture Assessment: Tongue Inspection
- The tongue exhibits a range of signs.
- Tongue coating can provide information about the digestive system and the health of the microbiome.
- The color of the tongue body can provide insight into the quality of perfusion and the status of the cardiovascular system.
- The sublingual veins are examined to assess for gross signs of blood stasis (reduced perfusion).
Acupuncture Assessment: Abdominal Palpation
- Abdominal palpation provides tactile information and information from the patient that can help clarify the diagnosis.
- The clinician is palpating acupuncture points and regions associated with specific organs to help understand Morgan’s presentation.
- Regions associated with the liver and the primary organs of digestion (spleen/stomach) are sensitive.
- Alarm point of the stomach is reactive.
Morgan's Findings: Summing Up
- Childhood history of cyclic vomiting may have been an early sign of liver qi depression and digestive weakness.
- Vomiting is "counter flow" movement of qi in Chinese medicine
- Repeated vomiting can harm the qi dynamic (normal peristalsis)
- This leads to body disorganization (disruption of qi dynamic), predisposition to headaches, irritability, and later dysmenorrhea associated with liver depression.
Concussion
- In Chinese medicine any traumatic injury can produce blood stasis.
- Persistent disruption of the qi dynamic can also cause blood stasis.
- The hesitant quality of the pulse is important is assessing blood stasis.
- Tongue signs also support this diagnosis.
Blood Stasis
- Blood stasis (blood not moving smoothly).
- Can be produced by trauma (sharp blow to the head) persistent disruption of orderly movement of qi and blood (early cyclic vomiting), and manifest in menstrual pain, headache and pulse and tongue signs.
- Impaired circulation may be associated with the vascular components of migraine
Chinese Medicine Diagnoses
- Liver overacting on the spleen (Qi and Blood Vacuity Pattern)
- Blood stasis in the liver and gallbladder channels (Obstructing the Network Vessels Pattern)
Evidence
- focal pain
- menstrual exacerbation
- relief with bowel movement
- tongue stasis signs
- tender Alarm Point of the Stomach
Findings Suggest:
- Diagnostic Patterns of Liver depression – Qi & Blood Vacuity and Blood Stasis Obstructing the Network Vessels both leading to migraine headache
- Acupuncture may be helpful
- 6-8 weekly treatments
- Key markers are reduction in frequency and severity
Acupuncture Needles

Treatment Planning
- Acupuncture point selection is an important part of treatment planning
In Morgan's case, points would be selected- based on the diagnostic patterns
- based on the regionalization of headache pain
- According to channel distribution
- based on the tenderness of established acupuncture points
- based on the presence of transiently reactive points on the channel sinews
- Treatment would be revised based on the patient's response
Acupuncture and Pediatric Migraine
- The evidence base for the use of acupuncture in pediatric migraine headache pain is quite limited. One prospective interventional cohort study (case series) examined acupuncture as treatment for emergent pediatric migraine in the ED.
- Conclusion: "With all subjects showing improvement or resolution of migraine headache, this pilot study introduces an alternative intervention to pediatric migraine management. Further studies are needed to evaluate the duration of symptom resolution and comparative effectiveness."
Reference
Graff et al. 2016 Auricular Acupuncture for the Treatment of Pediatric Migraines in the Emergency Department. Pediatric Emergency Care.
December 18th: Acupuncturist was Okay
December 27th: Coach Called
December 27th: Morgan's Doing Better
December 31st: Biofeedwhat?
January 2nd: Biofeedback Appointment
Biofeedback and Relaxation Exercise
Perception of sensation
Headache Intensity is Variable
0-1 to 10
Able to control headache at 3-4 level to avoid escalation
Distraction Techniques
- Read a book
- Talk to friends
Afferent Nerve Fiber Conduction
| Information Carried | Conduction Speed (mi/hr) |
|---|---|
| Pain (sharp, burning) | 2 mi/hr leisurely walk |
| Pain (cold, pressure) | 60 mi/hr highway driving |
| Awareness of the environment | 200 mi/hr airplane taking off |
Nerve Fibers and Pain Perception
The pain in your head has not gone away but very few nerve fibers carry that information to your brain. It’s so few that your brain doesn’t perceive the pain.
- When your mother asks you about your headache you stop paying attention to the TV.
- Now all these nerve fibers are carrying information about your headache.
- What you feel is your headache
Change Focus from Headache
If you’re able to do something else that takes your mind off your headache, you can actually not feel the headache
Biofeedback-Enhanced Relaxation
Identify strongest relaxation strategies:
- Deep breaths
- Favorite place
- Resting
- Music
Headache Intensity is Variable
0-1 to 10
Able to control headache at 3-4 level to avoid escalation
Thermal Biofeedback
Thermal biofeedback is based on blood flow changes occurring in the stress reaction.
Stress Reaction
Blood goes to the vital organs
- Brain
- Heart and Lungs
- Large muscles of the arms (fight) and legs (flight)
Stress vs. Relaxation
- During the stress response, blood does not flow to the small muscles of the hand
- Finger temperature goes down
- During the relaxation response, blood circulation returns to normal
- Finger temperature goes up
January 5th: Biofeedback's Cool
January 13th: Neurologist Again
January 17th: Neurologist Appointment
January 21st: Neurologist was Happy

