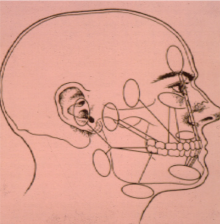
Common Facial Pain Referral Patterns
In acute tooth pulpalgia (pain arising from the dental pulp), the offending tooth usually is easy to discern as it will be very sensitive. Developing pulpalgia can make it very difficult to determine which tooth is responsible, and this can mimic many things including cluster headache, sinusitis, and trigeminal neuralgia. Diagnostic nerve blocks can be helpful, but sometimes observation is required until the offending tooth becomes more symptomatic and can be identified.
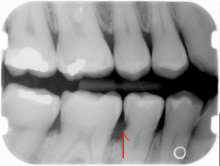
Caries
Caries (see arrows on images) can look like they should hurt, but they do not. The patient might have sensitivity to sweets or to stimulation of the dentin (tooth material under the hard enamel) that is exposed after tooth decay or a tooth fracture. Such symptoms can be expected but are not always present from exposed dentin. Temperature changes from air and fluid contact or touching the dentin will cause transitory pain. But if the tooth hurts spontaneously (by itself), one should expect a tooth nerve (pulpal) or a gum (periodontal) problem. This could be related to caries deep enough to involve the nerve tissue in the tooth but by themselves, caries do not cause pain.

Cracked Tooth: Sharp Pain With Biting
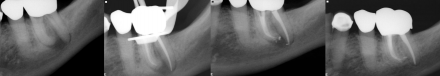
On this radiograph one observes well-healed apical tissues after excellent endodontic therapy (based on radiographic interpretation - the radiopacity in the apical 2/3 (noted by arrow on the image) of the tooth root is the endodontic root canal fill material). One would not expect this tooth to be sensitive to percussion.

If the tooth is sensitive to percussion, a tooth fracture should be considered with a casting (noted by arrow on the image) indicated to prevent separation of the fracture. Prognosis is fair; a radiolucency developing anywhere about the periodontal ligament (PDL) confirms the fracture, and the tooth would require extraction.

Pulpagia: Tooth Nerve Pain
Pain is moderate to severe and the patient will seek care immediately. The pain can awaken the patient at night and analgesics will only moderate the symptoms. Definitive treatment is required.

The following distinctions must be made:
- Acute versus chronic:
- In acute pulpalgia there are no radiographic signs of apical pathology versus in chronic pulpitis one sees positive radiographic signs of apical pathology
- Periapical abscess:
- Periapical abscess is extremely sensitive to palpation on the tooth (compressing inflamed periodontal ligament (PDL) at apex of tooth) and over the intraoral mucosa approximating the location of the tooth root apex (see arrow on image)
- Reversible:
- (sensitive to cold only and without prolonged sensitivity) versus irreversible (sensitive to hot and cold, prolonged sensitivity, and can have spontaneous pain (all signs of nerve sensitization (allodynia, hyperalgesia and spontaneous pain)
Periodontal Pain
Mild-to-moderate pain that can be tolerated. The patient will usually not seek care for periodontal (perio) pain unless an abscess develops.
A perio abscess is close to the gingival crest vs. pulpal abscess which approximates the apex (end of the root).
Perio abscess is moderately sensitive to percussion while periapical abscess is extremely sensitive to palpation on the tooth (compressing inflamed periodontal ligament (PDL) at apex of tooth) and over the intraoral mucosa approximating the location of the tooth root apex.

Root Canal Therapy for Chronic Periapical Periodontitis (CPP)
Note apical (end of root) radiolucency UL radiograph indicative of CPP. Tooth can be sensitive to percussion and biting, with a dull aching pain that can become spontaneous and constant. Note how the apical radiolucency heals after endodontic therapy is completed, removing all of the pulpal irritants that led to the periodontitis. Bone eventually fills in the apical area (LR radiograph).
Periapical Radiolucency: Is It Pathology?
This radiograph of a lower right 2nd bicuspid has had endodontic treatment followed by placement of retrograde amalgam (see arrow on image) after apical surgery (after failed endodontic treatment, the end of the root was amputated and a silver filling placed at the end of the tooth root to seal the canal). There is a periapical radiolucency at the apex (end, see dark area) of the endodontically (endo) treated tooth. If the tooth is sensitive to percussion consider a diagnosis of chronic periapical periodontitis from failed endo surgery. If it not sensitive to percussion, consider the radiolucency to be a bone scar, and observation without treatment is indicated.

Pericoronitis
Impacted wisdom teeth, as seen on this radiograph, are commonly asymptomatic. However, partially erupted teeth (see red arrow) can cause pericoronitis, localized inflammation of the gingiva surrounding the partially impacted tooth. Pericoronitis can be easily identified by visual exam, confirmed by palpation, and treated with warm salt water rinses and stimulation with a soft tooth brush. It is important to also rule out lymphadenopathy, which can indicate developing cellulitis requiring antibiotic therapy and definitive treatment.
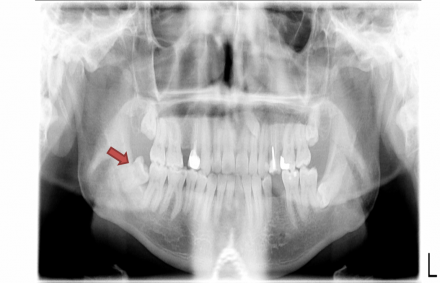
Pericoronitis of a partially-erupted left mandibular third molar
Treated with warm salt water rinses and stimulation with a soft tooth brush. If the problem reoccurs extraction is indicated.

Sinusitis
This radiograph highlights the proximity of the maxillary sinus (see tip of arrow) to the first molar. Although usually asymptomatic, when congestion occurs in the sinus the adjacent tooth can be sensitive to percussion (and biting) but not temperature.

Temporomandibular Joint Pain
The temporomandibular joint (TMJ) begins to translate at about 20 mm of jaw opening. If there is a disc displacement (DD), the jaw opening will deviate to the affected side giving an S shape to the opening pattern. If the displaced disc reduces (DD with reduction) the mandible will go back to midline (see arrow). If the disc does not reduce, the mandible will remain displaced to the affected side giving the diagnosis of DD without reduction. The “jerky” opening on the far right depicts a pattern consistent with a TMJ with arthritic changes in the joint which commonly is associated with course crepitus.
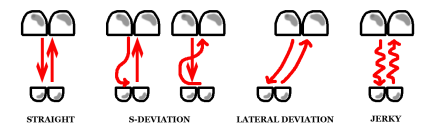
Image reproduced from: Fricton JR, Kroening RJ, Hathaway KM: TMJ and Craniofacial Pain: Diagnosis and Management. St. Louis, 1988, Ishiyaku EuroAmerica Inc.pg 46 Figure 5.5 (out of print, permission granted by author)
Temporomadibular Examination
Three-Part Protocol
- Range of motion
- Palpation
- Auscultation
Differential for Decreased Range of Motion
- Contracture
- Cranial nerve
- Muscle spasm
- Myositis
- Myalgia (myofascial pain)
- Disc displacement
TMD Exam: TMJ Arthralgia Diagnosis
To confirm, the patient must have pre-auricular pain with at least two of these three maneuvers:
- Palpation
- ROM
- Joint Loading (upwards and/or distal pressure on the mandible)
TMD Exam: Masticatory Muscle Diagnosis
Muscle pain differential:
- Spasm
- Contracture
- Myofascial disease
- Myositis
TMD: Myofascial Pain Diagnosis
This is the most common diagnosis.
- Dull aching pain
- Somewhat limited ROM
- Trigger point
- Hypersensitive area
- Referred pain
- Passive stretch
Osteoradionecrosis
While there is no true "cutoff" for the risk of osteoradionecrosis (ORN), many consider 5500-6000 cGy to be such a cutoff. If a tooth area received 30 Gy, you're okay to extract with low risk of ORN, whereas an area with 65 Gy would be at high risk.
The risk of ORN is lower in the maxilla because of increased vascularity. With traditional 2-D radiation modalities in the past, the maxilla also was believed to receive lower doses of radiation than did the mandible.
Hyperbaric oxygen (HBO) is generally not considered effective, aside from anecdotal cases of success and use as a means to "legally protect" oneself from possible legislation. There isn't much high-level clinical evidence for its efficacy. Also, it can be very expensive and not covered by insurance. Finally, there is anecdotal evidence that HBO can increase vascularity to quiescent tumor cells, which would be a problem.
Recommendations for Preventing Osteoradionecrosis
- Work with radiation oncologists/radiation physicists to "contour" and measure specific radiation doses to tooth-borne areas prior to extraction. This may be possible with radiation treatment planning software.
- If the specific areas of the patient’s dentition receive less than 5500 cGy, extract with caution after consenting the patient.
- If the areas receive greater than 5500 cGy, inform patient of likelihood of ORN prior to exodontia.
- HBO should only be considered at extremely high radiation doses to specific tooth areas, and only after considering the remote possibility of awakening dormant tumor cells as well as its high costs.

