Equianalgesic Dosing
Equianalgesic Example
From this table, you can compare potencies or "strengths" between the different opioids.
For instance, oral hydromorphone is more potent than oral oxycodone, which is more potent than oral morphine. Thus, lower doses of hyrdomorphone are needed for a similar effect of a higher dose of oxycodone.
| Oral/Rectal Dose (mg) | Opioid Analgesic | Intravenous Dose (mg) |
|---|---|---|
| 30 | Morphine | 10 |
| 0.4 | Buprenorphine | 0.3 |
| 200 | Codeine | 100 |
| N/A | Fentanyl | 0.1 |
| 30 | Hydrocodone | N/A |
| 7.5 | Hydromorphone | 1.5 |
| 20 | Oxycodone | N/A |
| 100 | Tramadol | N/A |
Equianalgesic Fentanyl
Calculations for transdermal fentanyl should be made based on the manufacturer's recommendations using the table below.
| Oral 24-Hour Morphine Equivalent (mg/day) | Transdermal Fentanyl Dose (mcg/hour) |
|---|---|
| 60-134 | 25 |
| 135-224 | 50 |
| 225-314 | 75 |
| 315-404 | 100 |
| 405-494 | 125 |
| 495-584 | 150 |
| 585-674 | 175 |
| 675-764 | 200 |
| 765-854 | 225 |
| 855-944 | 250 |
| 945-1034 | 275 |
| 1035-1124 | 300 |
Equianalgesic Methadone
There are numerous calculation methods for conversion to methadone. One method commonly used in practice is listed below.
| Oral 24-Hour Morphine Equivalent (mg/day) | Oral Dose Ratio (Morphine:Methadone) |
|---|---|
| greater than 100 | 3:1 |
| 101-300 | 5:1 |
| 301-600 | 10:1 |
| 601-800 | 12:1 |
| 801-1000 | 15:1 |
| greater than or equal to 1001 | 20:1 |
Pain Information
- International Association for the Study of Pain: http://www.iasp-pain.org/
- American Pain Society: http://americanpainsociety.org/
- Academy of Integrative Pain Management: http://www.aapainmanage.org/
- American Academy of Pain Medicine: http://www.painmed.org/
- American Chronic Pain Association: https://theacpa.org/
- National Fibromyalgia and Chronic Pain Association: http://www.fmcpaware.org/
Assessment Tools
11-point Numerical Rating Scale (NRS)
There are several different scales that can be used to assess for pain severity.
The most common is the 11-point Numerical Rating Scale (NRS), which uses the range 0-10. The benefits of the NRS are its simplicity and validity. Possible drawbacks include response variability and moderate correlation with functional status.

Opioid Risk Tool
Link opens a PDF version of the Opioid Risk Tool.
Numeric Risk Tool
Link opens a PDF version of the Numeric Risk Tool.
Quick DASH
Link opens a PDF version of the QuickDASH.
Functional Pain Scale (FPS)
Instructions:
Ask the patient if pain is present. If the patient has pain, ask him or her to rate the pain subjectively as either "tolerable" or "intolerable."
Finally, find out if the pain interferes with function.If the patient rates the pain as "tolerable," establish whether the pain interferes with any activity. If the pain is "intolerable," determine whether the pain is so intense as to prevent passive activities. See the chart below for guidelines.
- 0 No pain
- 1 Tolerable (and does not prevent any activities
- 2 Tolerable (but does prevent some activities
- 3 Intolerable (but can use telephone, watch TV, or read)
- 4 Intolerable (but cannot use telephone, watch TV, or read)
- 5 Intolerable (and unable to verbally communicate because of pain)
Scoring:
The patient's subjective rating of pain and the objective determination of the pain's interference with activities will produce a corresponding score on a scale of 0-5.
A lower score equates to less severe pain and less interference with functional abilities, if any. Ideally, all patients should reach a 0 to 2 level, preferably 0 to 1.
It should be made clear to the respondent that limitations in function only apply if limitations are due to the pain being evaluated.
Source:
Gloth FM III, Scheve AA, Stober CV, Chow S, Prosser J. The Functional Pain Scale: reliability, validity, and responsiveness in an elderly population. J Am Med Dir Assoc. 2001;2(3):110-114.
OPQRST
When assessing pain, it is important to ask certain questions in order to get a full understanding of the patient’s pain history. There are different methods you can use to remember the important questions to ask. One option is the pneumonic “OPQRST.”
O – Onset: When did the pain start? What was happening at that time?
P – Palliative and Provocative factors: What makes the pain better? Worse? (Include specific activities, positions or treatments.)
Q – Quality: Describe the pain. Is it burning, sharp, shooting, aching, throbbing, etc.?
R – Region and Radiation: Where is the pain? Does it spread to other areas?
S – Severity: How bad is the pain? (There are several scales to use, which will be discussed in the following slide)
T – Timing: When does the pain occur? Has it changed since onset? If so, how?
Reference:
Powell RA, Downing J, Ddungu H, Mwangi-Powell FN. Pain Management and Assessment. In: Andrea Kopf NBP, editor. Guide to Pain Management in Low-Resource Settings. Seattle: IASP: International Association for the Study of Pain; 2010. p. 67-79 http://www.iasp-pain.org/AM/Template.cfm?Section=Home&TEMPLATE=/CM/HTML….
Screening
Ask, "Are you experiencing any discomfort right now?"
If No: document “zero” pain and reassess periodically
If Yes: ask about its nature (verbal description) pattern (over time) and location
Try to quantify the intensity of the pain, show the patient the rating tools we use and determine which one is easiest and most meaningful for them.
Try to quantify the intensity of the pain, show the patient the rating tools we use and determine which one is easiest andmost meaningful for them.
Starting with the Numeric Risk Tool (remember, this is an eleven point scale of 0-10, not 1-10), ask the patient if they would recognize:
- if the discomfort were completely gone ("a rating of 0")
- or the worst they or anybody else could possibly experience ("10")
Have the patient rate the intensity of their pain/discomfort "right now" verbally with a number of by pointing to the number that represents their pain intensity.
Once the patient understands this scale, follow-up questions may be tried without the visual aid:
- "On a scale of 0 to 10, how much pain (or discomfort) are you experiencing now?"
If the Numeric Risk Tool is not easy and meaningful, use the Verbal Descriptor Scale:
- Determine if discomfort is "none" (chart 0) or the worst possible (chart 10).
- Ask if the discomfort or pain is mild, moderate, severe, or extreme.
-
- Record 2 (for mild), 4 (for moderate), 6 (for severe), or 8 (for extreme) accordingly.
- If the patient reports it's between two words, select the odd number between them (e.g. the score of a report of pain between mild and moderate = 3)
If that isn't easy and meaningful, use the Functional Pain Scale.
Determine if it is tolerable ("less than or equal to 5") or intolerable ("greater than or equal to 5").
- Tolerable pain that does not interfere with activities = 2
- Tolerable pain that interferes with physically demanding activities = 4
- Intolerable pain that interferes with physically demanding activities = 5
- Intolerable pain that interferes with active but not passive activities = 6
- Intolerable pain that interferes with passive acitivities (e.g. reading) = 8
- Pain so severe the patient can't do any active or passive activities (e.g. can't even talk about pain without writhing/screaming) = 10
Reassess using the 4-A's determining safety and efficacy of therapy:
- Analgesia: To what extent did the treatment reduce the pain and make it more tolerable? This can be evaluated using one of the pain intensity scales above, the percent that pain intensity is reduced by (e.g., 30%, 50%, etc.) or adjectives (good, excellent effect) the patient uses.
- Activity: To what extent did the patient's activity and rest patterns improve as a result of the treatment? Does pain interfere less with usual and prescribed therapeutic (e.g. physical therapy) activity? Does pain interfere less with sleep? Does the treatment affect safety?
- Adverse effects: What side effects, toxicity, technology-related complications are experienced?
- Aberrant behaviors: Has the medication affected medication-focuxed behaviors or personality?
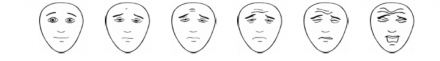
The Faces Pain Scale can also be used for any patient, but is especially useful with children or non-verbal patients. This is a well-studied and validated scale.
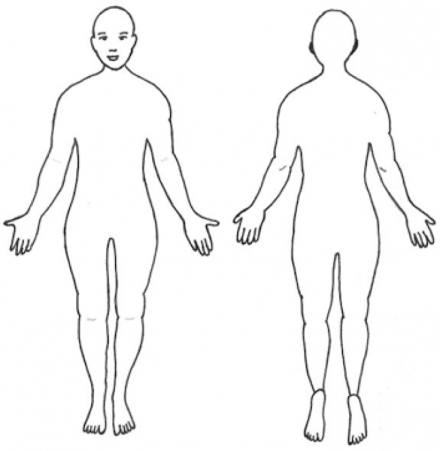
A body diagram can allow patients to pinpoint their pain site(s) to help guide your examination.
Additionally, observing patients when they move or during the exam is a useful addition to these scales, and is essential with young children and non-verbal adults.
Physical manifestations associated with acute pain, opioid withdrawal and opioid overmedication should be distinguished.
The table below matches the signs and symptoms to their corresponding condition(s) so you can see the similarities and differences for each condition.
| Signs/Symptoms | Acute Pain | Opioid Withdrawal | Opioid Overmedication |
|---|---|---|---|
| Tachycardia (fast heart rate) | Yes | Yes | No |
| Hypertension (high blood pressure) | Yes | Yes | No |
| Disphoresis (sweating) | Yes | Yes | No |
| Vasoconstriction (cold hands/feet) | Yes | Yes | No |
| Mydriasis (dilated pupils) | Yes | Yes | No |
| Tremors (shaking) | No | Yes | No |
| Dysphoria/anxiety (emotional state characterized by depression, anxiety, unease) | No | Yes | No |
| Flu-like symptoms (runny nose, congestion, malaise, etc.) | No | Yes | No |
| Depression (low mood) | No | Yes | No |
| Diarrhea/vomiting | No | Yes | No |
| Respiratory Depression (low respiratory rate) | No | No | Yes |
| Bradycardia (low heart rate) | No | No | Yes |
| Miosis (constricted pupils) | No | No | Yes |
| Vasodilation (warm extremities) | No | No | Yes |
| Myclonic jerks (sudden muscle contractions/twitches) | No | No | Yes |
Institute of Medicine Report
In 2011, the Institute of Medicine (IOM) released a report regarding pain as a public health problem in the United States. The IOM recommended relieving pain become a national priority [9].
National Pain Strategy
In 2016, The U.S. Department of Health and Human Services outlined the nation’s first coordinated plan for reducing chronic pain in The National Pain Strategy (NPS). It was developed by a diverse team of experts from around the nation. The National Pain Strategy is a roadmap toward achieving a system of care in which all people receive appropriate, high quality and evidence-based care for pain [10].
CDC Guideline for Prescribing Opioids for Chronic Pain
In 2016, the Center for Disease Control released the guideline for prescribing opioids for chronic pain.
Additional References Used In Module
- AGS Beers Criteria Update Expert Panel. American Geriatric Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60(4): 1-16. Available online at http://www.americangeriatrics.org/files/documents/beers/2012BeersCriteria_JAGS.pdf
- American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57 (8):1331-1346.
- American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012;116(2):248-273.
- Attal N, Cruccu G, Baron R, Haanpää M, Hansson P, Jensen TS, et al. (2010). EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17(9):1113-e88.
- Bril V, England J, Franklin GM, Backonja M, Cohen J, Del Toro D, et al. Evidence-based guideline: Treatment of painful diabetic neuropathy: Report of the American Academy of Neurology, the American Association of Neuromuscular and Electrodiagnostic Medicine, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2011;76(20):1758-1765.
- Chou R. et al. Management of Postoperative Pain: A Clinical Practice Guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee and Administrative Council. 2015 (12) 8. Journal of Pain.
- Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P, et al. (2009) Clinical guidelines for the use of chronic opioid therapy in noncancer pain. J Pain. 2009;10(2):113-130.
- Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012; 64(4):465-474.
- Institute for Clinical Systems Improvement . Assessment and Management of Chronic Pain, 5th edition. http://www.icsi.org/pain__chronic__assessment_and_management_of_14399/pain__chronic__assessment_and_management_of__guideline_.html. Published November 2011. Retrieved October 22, 2012.
- Management of Opioid Therapy for Chronic PainWorking Group. VHA/DOD clinical practice guidelines, management of opioid therapy (OT) for chronic pain. Department of Veterans Affairs and Department of Defense. http://www.healthquality.va.gov/cot/cot_310_full.pdf. Published 2010. Retrieved October 22, 2012.
- Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain. Pain Physician. 2012;15(Suppl):S1-S116.
- National Comprehensive Cancer Network (2012). NCCN Guidelines: Adult Cancer Pain, Version 1.2012. http://www.nccn.org/professionals/physician_gls/pdf/pain.pdf. Published 2012. RetrievedSeptember 11, 2012.
- McCracken LM, Boichat C, Eccleston C. Training for general practitioners in opioid prescribing for chronic pain based on practice guidelines: a randomized pilot and feasibility trial. J Pain. 2012;13(1):32-40.
- Page, M. Gabrielle et al. Risk of opioid abuse and biopsychosocial characteristics associated with this risk among chronic pain patients attending a multidisciplinary pain treatment facility. 2015. The Clinical Journal of Pain.
- Pain Terminology, International Association for the Study of Pain. Www. Iasp-pain.org.
- Rosenquist RW, Benzon HT, Connis RT, De Leon-Casasola OA, Glass DD, Korevaar WC, et al. Practice guidelines for chronic pain management: An updated report by the American Society Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 2010;112:810-833.
- Trescot AM, Datta S, Lee M, Hansen H. Opioid pharmacology. Pain Physician. 2008 Mar;11(2 Suppl):S133-53http://www.ncbi.nlm.nih.gov/pubmed?term=18443637.
- Turk, Dennis et al. Interdisciplinary Pain Management. American Pain Society White Paper American Pain Society.
Guide to the Dental Consult
Oncology, Temporomandibular Disorders, Acute Dental Pain
Dental Evaluation Protocol
- Evaluation
- Staging
- Patient Workup
- Treatment
- Management
Oncology Reference Links
Comprehensive guide for managing oral complications, such as oral mucositis and xerostomia, during cancer treatment from the National Cancer Institute.
Xerostomia in elderly (Turner M, Ship J. Dry mouth and its effect on the oral health of elderly people. JADA 2007:138:15s-20s.
Mucositis treatment (Epstein JB, Epstein JD, Epstein MS, Oien H, Truelove EL. Oral doxepin rinse: the analgesic effect and duration of pain reduction in patients with oral mucositis due to cancer therapy. Anesth Analg. 2006 Aug;103(2):465-70, table of contents.
Oropharyngeal tumor staging (Trotta BM, Pease CS, Rasamny JJ, Raghavan P, Mukherjee S. Oral cavity and oropharyngeal squamous cell cancer: key imaging findings for staging and treatment planning. Radiographics. 2011 Mar-Apr;31(2):339-54.)
Extra- and intraoral soft tissue exam video from the University of Minnesota)
Oral examination for Squamous Cell Carcinoma (Epstein JB, Güneri P, Boyacioglu H, Abt E. The limitations of the clinical oral examination in detecting dysplastic oral lesions and oral squamous cell carcinoma. J Am Dent Assoc. 2012 Dec;143(12):1332-42.
Temporomandibular Disorders (TMD)
TMD exam and treatment recommendations (PDF handout)
TMD care handouts: TMD clicks and locking; TMD self care therapies; stretching your jaw muscles.

