
Questions you might consider for Mr. Gateway's Dental Consult:
- How do you manage acute dental pain episodes in a patient already on opioids to control chronic pain?
- How do you distinguish tooth pain from reversible (requiring a normal filling) and irreversible (requiring endodontic (root canal treatment)) pulpitis?
- How do you distinguish between a temporomandibular joint and/or a masticatory muscle-based problem?
- Describe the protocol for managing a patient suffering from xerostomia. (Learn more about side effects of treatment for mouth and throat cancer and oral complications)
- Describe the priorities for dental treatment planning for a patient who is about to undergo radiation for head and neck cancer?
More information about various dental pain and exams to determine potential causes and diagnoses can be found by clicking the "Dental Pain" button at the bottom of the page.
You can find a summary of important articles, documents, and references for a dental consult by clicking the resources/references tab.
Dental Pre-Chemotherapy and Radiation Protocol
- Oncology asks for dent
- al evaluation
- Full radiographic and clinical dental exam to be reviewed by dentist to identify dental disease pre-treatment
- Dental intervention of acute disease
- Surgery for tumor removal
- Dental re-evaluation pre chemo-radiation
- Chemo-radiation therapy
- Dental maintenance
Mr. Gateway's Squamous Cell Carcinoma of the Tongue

A clinical photo of Mr. Gateway's tongue shows intraoral mixed red-white lesion. Such a lesion has an 80% chance of having pre-cancerous dysplasia. An unexplained white lesion (leukoplakia) has a 20% chance of containing dysplastic cells.
Surgery is scheduled to remove the affected region.
Mr. Gateway's Dental Imaging Pre-Treatment
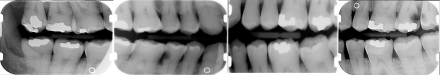
Bitewing radiographs
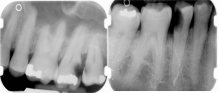
Periapical Radiographs
Pre-Surgery Dental Treatment
Mr. Gateway had hopeless and guarded teeth #1, #15, and #29 extracted before his tumor removal.
A periodontal debridement (gross teeth cleaning) was completed to control gingival inflammation.
Carious lesions #2 and #16 were restored.
Post-Surgery/Pre-Radiation Evaluation
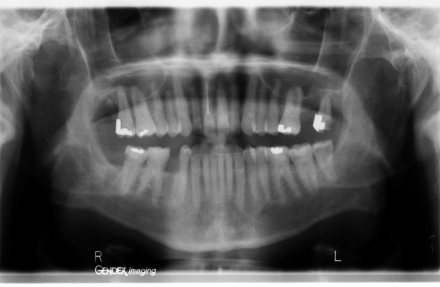
Panograph of Mr. Gateway's Dentition
Bitewing Radiographs
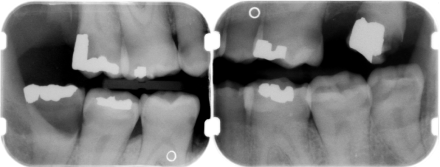
Tooth #32 was extracted and multiple carious lesions were identified (by tooth # and surface) and restored: 3LB, 4BLD, 5BD, 6B, 7B, 8I, 10B, 12BD, 13D, 14L, 18M, 19D, 21D, 28B, 30B
Teeth # 16, 17 were scheduled for extraction.
Mr. Gateway's TMD Examination Results
History
Patient has had limited range of motion (ROM) since his initial surgical procedure. Pain is a dull ache left > right at a 3-4 of 10 aggravated with jaw function such as eating or talking. His left maxillary teeth are sensitive, especially with jaw function.
Examination
(normal values: vertical ROM 40 mm, lateral symmetrical of at least 5-6 mm)
- Pain free jaw ROM was 22 mm, 34 mm with pain in the left masseter. Passive ROM via assistance 38 mm. He points to left superficial masseter at the insertion of the masseter on the zygoma as the pain’s location with increased ROM.
- Palpation: The patient is sensitive to palpation bilaterally under his mandible. Able to duplicate his chief complaint with palpation of the left superficial masseter which brings on his left posterior tooth pain.
- No joint sounds are evident
- Intraoral exam reveals numerous unrestored teeth. But he does contact bilaterally on his posterior teeth when closing his teeth together indicating that his occlusion is stable. No teeth are sensitive to palpation.
Mr. Gateway's TMD Diagnosis Summary
- Why rule out arthralgia?
-
- Patient has good lateral ROM and is negative to TMJ palpation.
- Why rule out contraction and spasm?
-
- Due to patient’s moderate pain level and ability to stretch muscle to increase ROM.
- Why is the myofascial pain diagnosis supported?
-
- Patient has moderate pain level aggravated with function, duplicated ULQ tooth pain with trigger point palpation, i.e. referred pain causing familiar pain.
- Treatment
-
- Jaw stretch exercises to improve pain free ROM, TMD self care therapies, PT referral based on response to home therapy.
Radiation Therapy and Risk of Osteoradionecrosis
Mr. Gateway is a 52-year-old male with a history of laryngeal cancer and tongue invasive squamous cell carcinoma invading tonsillar tissues who will be treated with 3 cycles of TPF chemotherapy. He will receive cisplatin therapy during radiation.
Radiation will be given over 60 treatment fractions:
- Tongue and regional lymphatics PTV1 dose 5400 cGy (180 per fraction) for 60 fractions. Rapid Arc technique with 6MV machine.
- PTV2 900 cGy (180 per ) for 5 treatments
- PTV3 900 cGy (180 per) for 5 treatments
- Total dose 7200 cGy
So the questions for you to consider are:
- What is the chance of developing osteoradionecrosis with future extractions?
- Do we consider just the dose to V2 of 900 cGy or the total dose of 7200 cGy?
- Does the increased vascularity of the maxilla as compared to the mandible reduce the chances of necrosis?
- How does hyperbaric oxygen (HBO) influence post-operative healing?

