
The Emergency Department (ED) calls you and says, “We have a 52-year-old male smoker with a history of substance abuse with recurrent laryngeal cancer who presents with increased throat and neck pain, dysphagia (pain with swallowing), and dehydration.”
You are part of the inter-professional team that will manage Mr. Gateway during his hospitalization. You are asked to come evaluate the patient who will be admitted to the surgical service and help advise on how to manage his pain.
Watch the video to review Mr. Gateway's history and presentation. You'll want to take notes on his history for reference during the case.
Mr. Gateway's History and Presentation
Dr. Barreveld wants to know what brings Mr. Gateway to the emergency department. She then asks him some questions about his medical history. Mr. Gateway explains his troubles with his mouth and throat.
Physical Exam
Vital Signs:
Temperature 97.2, Blood Pressure 152/88, Heart Rate 96, oxygen saturation 96% on room air
General appearance:
Thin man, mild distress
Head, ears, eyes, nose, throat and mouth exam:
Normocephalic, sclera anicteric, conjunctivae pale, oral mucosa dry, oropharynx clear, tongue midline and mobile. Missing molars in the left lower quadrant, mandibular incisor mobility. Decreased mouth opening and jaw range of motion. Numerous broken and unrepaired teeth and some gingival bleeding. There is a 6mm reddish white plaque on the left posterior lateral surface of his tongue
Neck:
Normal range of motion but neck pain radiating to right shoulder with neck extension, post-radiation skin changes, palpable thyroid with irregularly shaped anterior mass, bilateral submandibular lymphadenopathy
Lungs:
Soft expiratory wheezes otherwise clear
Heart:
Tachycardic, regular rhythm, no murmurs
Abdomen:
Soft, palpable liver tip, no masses, no tenderness to palpation
Extremities:
No cyanosis, clubbing or edema
Skin:
No rashes
Musculoskeletal:
Strength 5/5 upper and lower extremities
Neurological:
Alert and oriented, normal gait, cranial nerves intact
Lab Results
| Hematology: | |
|---|---|
| Lab Value | Result |
| White blood cell | 6.2 |
| Hematocrit | 31.4 |
| Platelets | 172 |
| Chemistry | |
| Lab Value | Result |
| Sodium | 145 |
| Potassium | 3.2 |
| Chloride | 109 |
| Bicarbonate | 29 |
| Blood Urea Nitrogen (BUN) | 33 (elevated level: patient may be dehydrated) |
| Creatinine | 1.5 |
| Liver enzymes | |
| Lab Value | Result |
| Total bilirubin | 0.8 |
| aspartate aminotransferase (AST) | 82 (AST:ALT ratio of 2:1 may be a sign of chronic alcohol abuse, but other lab values examining liver synthesis are within normal limits: e.g. INR - not shown - and platelet count) |
| Alanine aminotransferase | 39 |
| Alkaline Phosphatase | 135 |
| Urine Toxicology | |
| Lab Value | Result |
| oxycodone | negative (patient has not taken oxycodone in likely over a week as the oxycodone is not detected by a urine screen 3-4 days after the last dose) |
| Tetrahydrocannabinol (THC) | positive (patient has used marijuana in the recent past) |
| All other substances | negative |
Imaging Studies
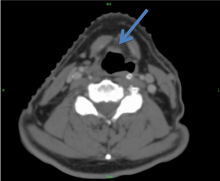
The arrow on this axial image from a computered tomography (CT) scan of the neck shows cancer invading the thyroid.
The CT scan overall demonstrates post-surgical/radiation changes and recurrence of laryngeal mass with thyroid cartilate invasion. Imaging also notable for mass at the base of the tongue and lymphadenopathy (image not shown).
Next Steps
In addition to radiation oncology and oncology input to guide with staging and treatment, a dental consult is initiated to evaluate Mr. Gateway's limited mouth range of motion and mouth pain.
The National Cancer Institute offers excellent guidelines on oral and dental management prior to cancer therapy.

