There are many reasons for orofacial pain, but a thorough assessment and examination of a patient should result in a limited list of differential diagnoses. Chronic pain without definitive underlying pathology may be included on this list. Treatment of pain should address both the mechanisms of pain and, if identified, the underlying pathology that prompted the patient’s pain.
Patient Symptoms
Your patient reports jaw clicking without and with pain, and frequent headaches for three months.
During the neurophysiology visit you will learn about performing a thorough exam. In subsequent visits you will learn how to further assess your patient’s pain, the underlying mechanisms for the pain and consider treatment options to address these mechanisms and your patient’s pain.
Considerations
What could be the potential causes of your patient’s pain?
Were there any findings from your assessment and physical examination of your patient that are concerning, i.e. RED FLAGS?
During this visit, the major causes of oral and facial pain will be outlined and RED FLAG findings that require immediate attention or additional diagnostic procedures will be highlighted. Consider the many potential causes of your patient’s jaw clicking and accompanying pain.
Review of Symptoms
Jaw Clicking Without Pain
Your patient reports jaw clicking without pain. This is very common. Pain-free clicking does not require additional diagnostic tests or imaging (MRI, CT).
Jaw Clicking With Pain
Your patient also reports jaw clicking with pain.
Additional Considerations
- Is it localized or diffuse?
- What are the pain characteristics?
- Onset
- Intensity
- Quality
- Frequency
- Duration
- Aggravating & alleviating factors
Suggested Diagnostic Procedures
- HEENT and intraoral exam including lymph node palpation
- Cranial Nerve screening
- X-Ray of the maxillofacial region to rule out infections and bony pathology additional diagnostic tests as needed
Frequent Headaches
Your patient reports frequent headaches for 3 months.
Additional Considerations
- Rule out life-threatening sources of headache:
- Use SNOOP to rule out secondary headaches, malignancy
- Consider lab tests and imaging
SNOOP
Snoop is an acronym to assist healthcare providers in thoroughly examining patients with headaches and identifying serious pathology Red Flags. Snoop is a concise screening method to determine if a headache is a primary or secondary headache.
Presence of headache with positive finding during SNOOP:
- SYSTEMIC SYMPTOMS or SYSTEMIC DISEASE
- NEUROLOGIC SYMPTOMS or SIGNS
- ONSET (new onset, sudden)
- OLDER (age >40 years)
- PATTERN CHANGE
Red Flags from History/Patient Report
- Oral and Facial Pain in the Absence of Headaches
Be sure to:
- Assess Neurological signs or symptoms
- Assess Systemic signs or symtoms
- Be suspicious of Temporal Arteritis
RED FLAG
Any patient who has failed conservative therapy for more than 2-3 weeks (pharmacotherapy, physical medicine, etc.) should be re-examined for the potential of progressive pathology that could not be detected during the initial examination.

Red Flags from Physical Exam
- Papilledema
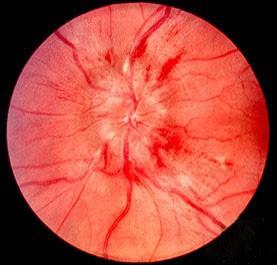
* image retrieved from https://en.wikipedia.org/wiki/Papilledema#/media/File:Papilledema.jpg
- Abnormal cranial nerve screening or neurological signs including paresthesias and dysesthesias
- Sudden limited ROM of jaw opening to less than 15-20mm
- Tender enlarged temporal artery
Be sure to:
- Rule out infection or trismus
- Rule out malignancy or pathology
- Rule out internal joint derangement (*not a red flag: however benefits from prompt treatment)

